Inactıve hepatitis B surface antigen carriers and intrafamilial tramsmission: results of a 10-year study
Article information
Abstract
Background/Aims
The aims of the present study were to determine the outcomes of inactive hepatitis B virus (HBV) surface antigen (HBsAg) carriers over a 10-year study period and to elucidate the HBV serological profile of their family members.
Methods
We retrospectively analyzed the medical files of inactive HBsAg carriers followed up at the Department of Infectious Diseases of Kocatepe University Medical Faculty Hospital between March 2001 and January 2011.
Results
In total, 438 inactive HBsAg carriers were enrolled in this trial. The follow-up period was 33.7±22.5 months (mean±SD). Anti-hepatitis-B surface antibody seroconversion occurred in 0.7% of cases, while chronic hepatitis B was found in 0.5%. The anti-hepatitis-D virus (HDV) status was evaluated in 400 patients and anti-hepatitis C virus (HCV) in 430. It was found that 1% and 0.2% were positive for anti-HDV and anti-HCV, respectively. HBV serology was investigated in at least 1 family member of 334/438 (76.3%) patients. The HBsAg positivity rate was 34.6% in 625 family members of 334 patients. A comparison of the HBsAg positivity rates in terms of HBV DNA levels in index cases revealed that HBsAg seropositivity rates were higher in family members of HBV DNA-negative patients than in family members of HBV DNA-positive cases (P=0.0001).
Conclusions
The HBsAg positivity rate was higher in family members of inactive HBsAg carriers than in the general population; these family members therefore have a higher risk of HBV transmission. Furthermore, despite negative HBV DNA levels, transmission risk was not reduced in these patients, and horizontal transmission seems to be independent of the HBV DNA value.
INTRODUCTION
Inactive carriers are the largest group of chronically infected hepatitis B virus (HBV) patients and are diagnosed by the absence of HBe antigen and the presence of anti-HBe antibody, undetectable or low HBV DNA levels, and normal alanine transaminase (ALT) levels. There are an estimated 300 million inactive hepatitis B surface antigen (HBsAg) carriers worldwide; however, this clinical condition is associated with a better prognosis than chronic active hepatitis B infection.1,2,3
HBV is a major health concern worldwide and is mainly transmitted via infected blood and blood products, in addition to parenteral/permucosal contact with genital secretions. Intra-familial transmission, which is a form of horizontal transmission, is more common in countries located in moderately endemic areas of HBV infection.4,5 Therefore, the aims of the present study were to determine the outcomes of inactive HBsAg carriers over a 10-year study period and to analyze the HBV serological profile of their family members.
METHODS
In the present study, we retrospectively assessed the medical files of patients presenting to the outpatient clinic of the Department of Infectious Diseases of Kocatepe University Medical Faculty Hospital between March 2001 and January 2011 and diagnosed as inactive HBsAg carriers, who were followed-up regularly in the same outpatient clinic thereafter, with a minimum follow-up period of 1 year. The interval of follow-up was 3, 6 or 12 months according to characteristics of the patient but this time was no more than 12 months. The patients who were not regular follow-up aren't included to the study.
Diagnosis as an inactive HBsAg carrier was based on HBsAg positivity for at least 6 months, HBV DNA-negative or below 2,000 IU/mL, negative HBeAg, and normal ALT values.1 Patients were followed-up yearly by assessment of ALT, HBV DNA, HBsAg, and anti-HBs serologies, as well as abdominal ultrasonography. The duration and outcome data of follow-up visits were evaluated. HBV DNA values and anti-HDV and anti-HCV serologies of the participants were recorded.
In follow-up period the patients, who their HBV DNA and HBsAg became negative and their anti-HBs antibody became positive, were evaluated in "seroconversion status". On the contrary the patients who their HBV DNA and ALT became above 2,000 IU/mL and upper limit of normal, respectively, were evaluated as chronic hepatitis B (CHB).3
Also, the HBV serologies were assessed in at least one family member of the patients (i.e., spouses, children, parents, and siblings) to calculate the sero-positivity rates. Individuals with anti-HBs positivity only were regarded as vaccinated cases, while individuals with positive anti-HBcIgG and anti-HBs antibodies were considered as having natural immunity.
Statistical assessment of the study was performed using Pearson's chi-square test and Student's t-test by SPSS version 15.0 (IBM Co., Armonk, NY, USA).
RESULTS
A total of 438 inactive HBsAg carriers [180 (41.1%) women (mean age, 39.68±12.31 years) and 258 (58.9%) men (mean age, 38.99±12.20 years)] were enrolled in the trial and followed-up for a mean period of 33.71±22.5 months (range, 12-84 months). HBV DNA was negative in 192 patients (43.8%) and positive, but under 2000 IU/ml in 246 cases (56.2%). The mean HBV DNA value among HBV DNA-positive participants was 1758.66±4125.82 IU/mL. During the follow-up period, anti-HBs seroconversion developed in three patients (0.7%) and CHB was determined in a patient (0.5%). Patient characteristics are presented in Table 1.
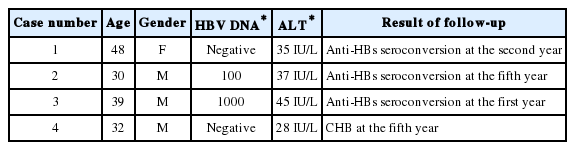
First-admission characteristics of patients with anti-HBs seroconversion or CHB that developed during the follow-up period
Anti-HDV status was evaluated in 400 patients and anti-HCV in 430 cases. Four (1%) patients were classified as anti-HDV-positive and one (0.2%) as anti-HCV-positive.
In 334 (76.3%) of the enrolled 438 patients, hepatitis B serology was investigated in at least one family member. Hepatitis B serology was investigated in a total of 625 family members related to 334 index cases, of which 233 of these individuals were spouses and 392 were other family members (siblings, children, or parents). Among all family members, the rates of HBsAg positivity, HBV vaccinated, and natural immunity to HBV were 34.6%, 15.7%, and 11.8%, respectively (Table 2).
Among 185 of the 246 HBV DNA-positive index cases, a total of 345 family members were screened for HBV and 114 (33%) were determined as HBsAg-positive. Among 146 of the 192 HBV DNA-negative index cases, a total of 280 family members were screened, revealing positive values in 102 individuals (36.4%). A comparison of HBsAg positivity rates among family members of HBV DNA-positive or -negative cases revealed higher rates among the HBV DNA-negative cases compared to the positive cases (P=0.0001).
The HBV serology findings of family members of index cases are presented in Table 3.
Assessment of HBsAg positivity of each family member in terms of the HBV DNA status of index cases revealed significantly higher HBsAg positivity rates among the daughters of index cases with negative HBV DNA only, compared to the daughters of HBV DNA positive cases (P=0.001). No statistically significant differences were found among other family members (Table 3).
DISCUSSION
Inactive HBsAg carriers generally have a favorable prognosis; however, they carry a risk of cirrhosis or hepatocellular carcinoma due to infection reactivation over time. Reportedly, 1-3% of inactive HBsAg carriers are also negative for HBeAg CHB and the rate of spontaneously HBsAg loss and anti-HBs antibody occurrence among inactive HBsAg carriers has been reported 1% in the literature.6,7 Therefore, regular follow-up is of the utmost importance because, in these patients, infection re-activation and spontaneous anti-HBs seroconversion may develop.5,6
According to trial results of inactive HBsAg carriers with a mean follow-up period of 13 years, HBsAg disappeared in 8.2% of cases, anti-HBs seroconversion was indicated in 5.1%, and the annual spontaneous anti-HBs seroconversion rate was 1%. In the same trial, it was emphasized that the HBV DNA values were negative among patients with spontaneous seroconversion.8 In the current trial, the spontaneous seroconversion rate (0.7%) was lower than those previously reported in the literature. However, it is curious that the HBV DNA values were positive in both patients with spontaneous seroconversion. On the other hand, CHB developed during the study period in one patient with a negative HBV DNA value. Although the number of cases was limited in the current trial, our results indicated that inactive HBsAg carriers should be closely monitored because of the risk of spontaneous seroconversion and CHB, irrespective of the corresponding HBV DNA values.
Various HDV prevalence rates have been reported among HBsAg carriers among different regions worldwide. A previous trial conducted in Turkey reported an anti-HDV rate of 0.5% and 1.6% among inactive HBsAg carriers.9 In the current trial, the anti-HDV positivity rate was 1% among inactive HBsAg carriers residing in the central Anatolian area. Our results were generally similar to those reported in previous trials conducted in Turkey; however, we found an anti-HCV seroprevalence rate of 0.2% in inactive HBsAg carriers, whereas the anti-HCV positivity rate in the general Turkish population is reportedly 1%.10 According to our data anti-HCV seroprevalance is lower previous study published from Turkey. In recent years emphasis on viral hepatitis increased in our country. There is accelerated screening and prevention efforts by implemented health policies. So the rate of HCV seroprevalence decreased result of this effort. But our result shows that new studies should be performed about HCV seroprevalence as to verifiy our data.
In the current trial, the HBsAg positivity rate was 34.6% among the family members of inactive HBsAg carriers. The prevalence of HBsAg carriers is repored as 2-7% in Turkey, as the country is located in a moderate endemic region in terms of prevalence rates of HBV infection.11 HBsAg positivity rates in family members of inactive HBsAg carriers in this trial seemed to be relatively high, as compared to the general population. In accordance with previous studies, our data supported the opinion that family members of inactive HBsAg carriers pose a significant risk for infection transmission.12,13,14
In chronic HBsAg carriers, the risk of parenteral transmission increases as the HBV DNA blood levels increased. However, an increase in the probability of horizontal transmission is also dependent on close and prolonged contact rather than serum HBV DNA levels.5 In the current trial, HBsAg positivity in the family members of HBV DNA-negative index cases was found to be higher than the values in HBV DNA-positive index cases. Based on this finding, we propose that HBV DNA negativity among inactive HBsAg carriers does not necessarily lead to decreased transmission. On the contrary, transmission increased among patients with a negative viral load as opposed to positive cases, which might be associated with prolonged contact, although this cause was not addressed in the context of this trial.
Unfortunately in this study, we were not able to evaluate all family members of index cases. Because of our study was designed retrospectively, this is the main restirictive point of our study. However, our result may lead the way of a new study because it contains large subjects.
In conclusion, inactive HBsAg carriers is a significant clinical state, irrespective of negative or positive serum HBV DNA levels, as such cases carry a risk of CHB and spontaneous seroconversion, even if they exhibit negative HBV DNA levels. Furthermore, they constitute a significant risk group in terms of horizontal HBV transmission, irrespective of HBV DNA levels, thus HBV screening among family members and educating patients on the features of the infection is crucial to maintain public health. Although no specific symptom is evident, identification of HBsAg carriers is essential to reduce infection transmission within a community. Therefore, especially in areas where infection is highly prevalent, HBsAg assessment at various time-points, such as prior to marriage or surgery, may prove to be beneficial in determination of inactive HBsAg carriers.
Notes
The authors have no conflicts to disclose.
Abbreviations
ALT
Alanine amino transpherase
CHB
Chronic hepatitis B
HBsAg
Hepatitis B Surface antigen
HBV
Hepatitis B virus
HCV
hepatitis C virus
HDV
Hepatitis D virus

