Vogt-Koyanagi-Harada disease occurring during pegylated interferon-α2b and ribavirin combination therapy for chronic hepatitis C
Article information
Abstract
Vogt-Koyanagi-Harada (VKH) disease is a multisystem syndrome characterized by ocular (uveitis and retinal detachment), neurological (headache, tinnitus, and meningitis), and integumentary (vitiligo, alopecia, and poliosis) involvement. Although the pathogenesis of VKH disease is not well understood, an autoimmune T-cell response to a melanocyte-associated antigen is considered to be a cause of VKH disease. The complex immunological response to interferon and ribavirin may induce or exacerbate the autoimmune condition; however, VKH disease is a very rare complication associated with interferon therapy in chronic hepatitis C. We report a case of VKH disease occurring during pegylated interferon-α2b and ribavirin combination therapy for chronic hepatitis C.
INTRODUCTION
Interferon combined with ribavirin is commonly used in treating chronic hepatitis C. Interferon sometimes results in common side effects such as flu-like symptoms, fatigue, myalgia, headache, and in rare but fatal ones such as depression, suppressed bone marrow, interstitial pneumonia, diabetes, or autoimmune diseases.1 Vogt-Koyanagi-Harada (VKH) disease is a multi-systemic granulomatous inflammatory disease with ophthalmic involvement (uveitis and retinal detachment), ear and meningeal involvement (headache, tinnitus, and encephalomeningitis), and skin and hair change (vitiligo, alopecia, and poliosis). It is a very rare complication associated with the interferon treatments.2 The mechanism of VKH disease has not been known yet, but it is presumed that interferon brings alterations to the immunological responses to melanocytes.3 We report a case of VKH disease which occurred during pegylated interferon and ribavirin therapy for chronic hepatitis C.
CASE REPORT
A 58-year-old woman visited our hospital for evaluation of chronic hepatitis C. The patient was diagnosed as chronic hepatitis C 10 years ago, but had not received any treatment. She had been taking amlodipine 5 mg for hypertension for 8 years. She had no history of alcohol consumption, smoking, or injection drug use. Dermatological, pulmonary, cardiac and neurological examinations were normal. On her first visit to our hospital, the liver function test and the complete blood cell count were normal, and the serologic tests for hepatitis A and B and HIV were negative. She was infected with hepatitis C virus (HCV) genotype 1b, and HCV RNA level was 3.8×106 copies/mL. There were no specific findings except for the hepatic cyst from abdominal CT scan. Liver biopsy was recommended to evaluate liver inflammation and fibrosis, but she refused. She was commenced on pegylated interferon-α2b 80 µg (1.5 µg/kg) weekly by subcutaneous injection and ribavirin 400 mg orally twice daily. Serum HCV RNA level decreased below 25 copies/mL within 12 weeks after the start of interferon, thus she achieved an early viral response.
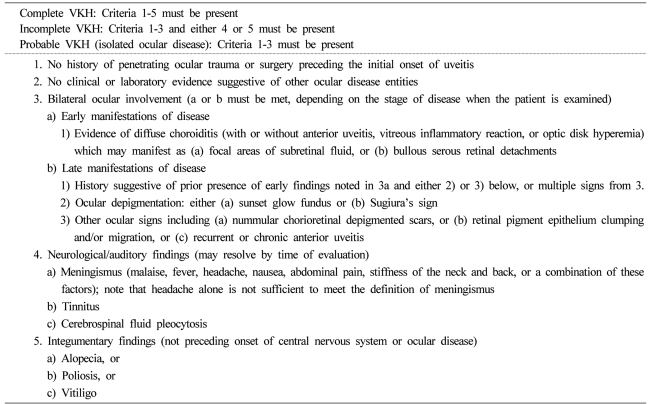
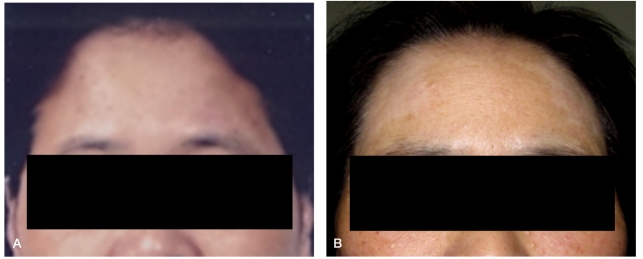
After 9 months of interferon and ribavirin treatment, the patient complained of blurred vision and headache. On physical examination, the vitiligo around her forehead and scalp was shown (Fig. 1), but there was no sign of meningeal irritation. Optic fundal examination showed uveitis and retinal edema. Retinal fluorescein angiography (Fig. 2) showed leakage of fluorescein dye from the choroid into the subretinal space. The serous retinal detachment was seen clearly in the right eye from optimal coherence tomography (Fig. 3A). Cerebrospinal fluid examination and the magnetic resonance imaging (MRI) to identify the encephalomeningitis showed no abnormal findings. The level of angiotensin-converting enzyme showed normal range, the erythrocyte sedimentation rate and the C-reactive protein were also normal, and the antinuclear antibody and the rheumatoid factor were negative. She was diagnosed as having incomplete VKH disease, therefore pegylated interferon-α2b and ribavirin were discontinued, and intravenous pulses of methylprednisolone at a dose of 1 g for 3 days, followed by daily oral administration at a dose of 60 mg prednisolone were introduced. After 2 weeks of steroid therapy, her eyesight was getting better, and retinal detachment disappeared (Fig. 3B). Prednisolone was progressively tapered to 10 mg daily during next two months, but relapse occurred. Intravenous pulses of methylprednisolone followed by oral prednisolone were performed. The uveitis and visual acuity improved. While the HCV RNA had not been detected during the treatment of pegylated interferon-α2b and ribavirin, serum HCV RNA level increased to 3.0×107copies/mL after ceasing of interferon based therapy. Oral prednisolone was slowly tapered to 10 mg daily and no relapse occurred.
The patient's face before treatment (A). The 5-cm vitiligo on the forehead appears after 9 months of pegylated interferon-α2b and ribavirin combination therapy (B).
Retinal fluorescein angiography reveals characteristic multiple pinpoint leakages of fluorescein from the choroid into the subretinal space on the right eye (A) and the left eye (B).
DISCUSSION
Most of ophthalmological complications occurring during interferon therapy are benign, transient, and characterized by interferon-related retinopathy. Incidence of interferon-related retinopathy such as hemorrhage and cotton wool spots vary from 6 to 13%.4 The rate of these complications is reported to be higher in patients with diabetes or hypertension, but is not related with HCV genotypes, platelet counts or types or dose of interferon.5 More than 90% of the retinal diseases during the interferon treatment occur within the first 8 weeks. Therefore, the retinal test must be carefully implemented from the time before interferon treatment to the 8 weeks after initial treatment. Even though it can lead to permanent vision loss without proper treatment in the early stage, most retinal complications were asymptomatic, not associated with impairment of visual acuity, and reversible after discontinuation of interferon therapy.6,7 There are two severe forms of intraocular complications which result in severe visual impairment. The first form is represented by VKH, one of the inflammatory intraocular disorders and the second form is retinal vascular disorders including central retinal arterial/venous occlusion.
The VKH disease was first described as poliosis, vitiligo, anterior uveitis, and tinnitus by Vogt and Koyanagi, and described as posterior uveitis with retinal detachment by Harada in 1926. The VKH disease is a rare multisystem syndrome that attacks melanocytes-containing tissue such as eye, skin, hair, inner ear, and cerebral meninges.3 This can be divided into 4 phases; prodromal neurologic phase, acute uveitis phase, chronic convalescent phase that is characterized by a progressive depigmentation of the skin and the fundus, and chronic recurrent phase.8 This mainly occurs in 30 to 40 year old women and more frequently in Asian, Latino, Native American, or Asian Indian.8,9
The pathophysiological mechanism of this disease is not obviously known, but it is presumed to be an autoimmune response of the type 1 helper T-cell (Th1) to antigens related with melanocytes.9,10 This can be supported by the fact that when lymphocytes of the patient with VKH are exposed to melanocytes, the lymphocytes proliferate significantly.11 Cutaneous injury or viral infection may induce sensitization of melanocyte and may precipitate the VKH disease. And also, thyroid disease or rheumatoid arthritis can be associated with VKH disease.12,13
Interferon enhances lymphocyte cytotoxicity, reveals class I antigens of major histocompatibility complex, and differentiates antigen-presenting cells. It might also make people sensitive to autoimmune diseases easily get ill through increasing the productions of proinflammatory cytokines, and worsen autoimmune diseases such as lupus, rheumatoid arthritis, and psoriasis.14,15 Indeed, there are a few case reports about VKH disease occurrence in the treatment combined with interferon and ribavirin for chronic hepatitis C.16
The occurrence of VKH disease in patient with HCV infection before interferon therapy also arouses suspicion regarding the role of the HCV in the pathogenesis of the disease.16 Molecular mimicry between viral antigens and melanocyte-related antigens could lead to VKH disease. However, most reports about its occurrence during interferon treatment for chronic hepatitis C suggest that interferon therapy rather than HCV infection per se may play a role in the development of VKH.17
In order to achieve successful outcome and to prevent complications associated with interferon, selection of patients for the treatment is most important. Generally, the ones who have persistently normal alanine aminotransferase (ALT) levels were not a good candidate for the treatment since individuals with persistently normal ALT values have significantly less liver fibrosis than whom that have abnormal ALT levels.18 In this case, her liver function tests were normal on her first visit to our hospital, but levels of transaminase had been shown above than 40 IU/L several times in her family doctor's clinic. Therefore she was not a person who had persistently normal ALT levels, and was worried about progression of liver disease and wanted to treat chronic hepatitis C. Hence, we decided to start interferon and ribavirin therapy without confirm of liver histology.
The revised diagnostic criteria of VKH disease (Table 1) has been clarified.16,17 While five items must be satisfied to be diagnosed as a complete VKH disease, it is diagnosed as an incomplete VKH disease when four items including a symptom among neurologic or dermatological conditions are satisfied. The present patient had no vitiligo before the interferon therapy (Fig. 1A), after 9 months of starting interferon therapy, about 5 cm sized patches of de-pigmentation were seen around both lateral side of her forehead symmetrically. Thus the patient met the criteria for incomplete VKH disease.
The treatment of the VKH disease is performed mainly using high dose of steroid, and the aggressive treatment in the early stage is important to turn around the eye-related symptoms.9 Administration of corticosteroid and stopping antiviral agents controlled ocular manifestations in the past reports about VKH disease associated with interferon/ribavirin. Also in our case, discontinuation of interferon/ribavirin and high-dose systemic steroid therapy could improve ocular changes and visual outcomes. To treat the recurrent or steroid-resistant VKH disease, cyclosporine, antimetabolites, and alkylating agent have been used.19
Several treatment modalities can improve vitiligo. Commonly used repigmentation therapies including ultraviolet light and/or topical applications of corticosteroids or calcineurin inhibitors are sometimes effective.20 Depigmentation of the unaffected skin is another option in cases of extensive vitiligo. However, there is no cure for vitiligo. In this case, her skin lesions were not improved despite systemic and topical corticosteroid agents.
In summary, VKH disease, which can be induced by pegylated interferon-α2b and ribavirin combination therapy may lead to irreversible visual loss. Thereby, awareness of screening for ocular manifestations and early treatment are necessary.
Abbreviations
VKH
Vogt-Koyanagi-Harada
HIV
human immunodeficiency virus
HCV
hepatitis C virus
RNA
ribonucleic acid
CT
computed tomography
MRI
magnetic resonance imaging
ALT
alanine aminiotransferase