Causes and risk profiles of mortality among individuals with nonalcoholic fatty liver disease
Article information
Abstract
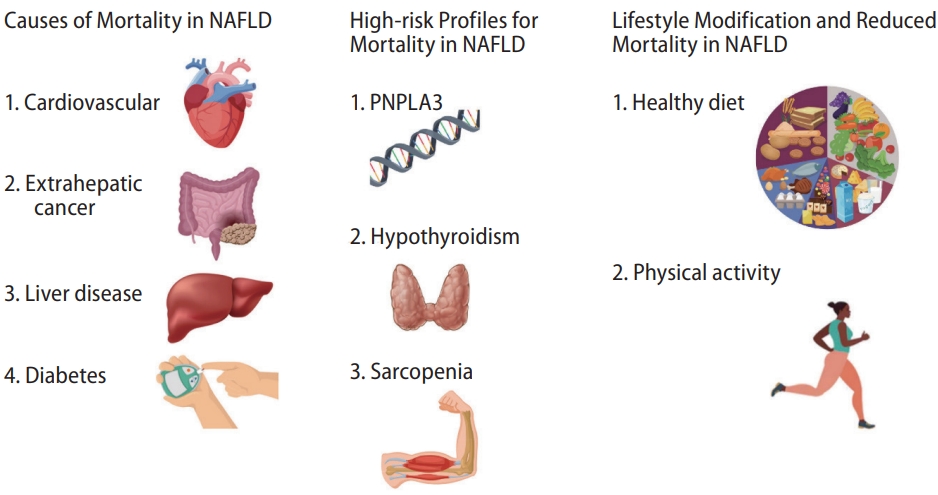
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease in the United States and worldwide. Though nonalcoholic fatty liver per se may not be independently associated with an increased risk for all-cause mortality, it is associated with a number of harmful metabolic risk factors, such as type 2 diabetes mellitus, hyperlipidemia, obesity, a sedentary lifestyle, and an unhealthy diet. The fibrosis stage is a predictor of all-cause mortality in NAFLD. Mortality in individuals with NAFLD has been steadily increasing, and the most common cause-specific mortality for NAFLD is cardiovascular disease, followed by extra-hepatic cancer, liver-related mortality, and diabetes. High-risk profiles for mortality in NAFLD include PNPLA3 I148M polymorphism, low thyroid function and hypothyroidism, and sarcopenia. Achieving weight loss through adherence to a high-quality diet and sufficient physical activity is the most important predictor of improvement in NAFLD severity and the benefit of survival. Given the increasing health burden of NAFLD, future studies with more long-term mortality data may demonstrate an independent association between NAFLD and mortality.
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is defined as hepatic steatosis in the absence of significant alcohol consumption or other alternative explanation for hepatic fat deposition, such as underlying other chronic liver diseases [1,2]. It is closely associated with type 2 diabetes mellitus, hyperlipidemia, obesity, gallstone disease, a sedentary lifestyle, and an unhealthy diet [3-5]. NAFLD is the most common cause of chronic liver disease in the United States, where prevalence passed over 30% in 2017–2018 [6]. Prevalence of NAFLD is similarly high in other parts of the world, particularly the Middle East and South America [1]. While the prevalence of chronic viral hepatitis has decreased over the past decade, the prevalence of NAFLD has steadily increased over the same period, coinciding with increasing rates of obesity and type 2 diabetes [7,8]. The US national prevalence of NAFLD-related advanced fibrosis increased from 2.6% in 2005–2008 and 4.4% in 2009–2012 to 5.0% in 2013–2016 [7]. Age-standardized mortality in individuals with NAFLD has also been steadily increasing over the past decade at an annual rate of 7.8% [9]. Though projected to further increase by 44% between now and 2030 [10], mortality for NAFLD still remains lower than those seen in chronic hepatitis C virus (HCV) infection or alcohol-related liver disease (ALD) [9]. The most common cause-specific mortality in individuals with NAFLD is cardiovascular disease, followed by mortality due to extra-hepatic cancer, liver-related mortality (including hepatocellular carcinoma, HCC), and diabetes [11]. When controlling for comorbid conditions such as diabetes, hypertension, smoking status, hyperlipidemia, and obesity, NAFLD per se is not associated with increased allcause or cause-specific mortality, likely because a large proportion of this mortality is due to cardiovascular deaths driven by comorbid metabolic abnormalities [12,13]. In contrast, metabolic dysfunction-associated fatty liver disease, which requires the presence of metabolic risk factors in the setting of hepatic steatosis, is associated with increased all-cause and cardiovascular mortality [13,14]. In this review, we focus on the causes and risk profiles of mortality among individuals with NAFLD (Fig. 1).
EPIDEMIOLOGY OF MORTALITY IN NAFLD
All-cause mortality in NAFLD
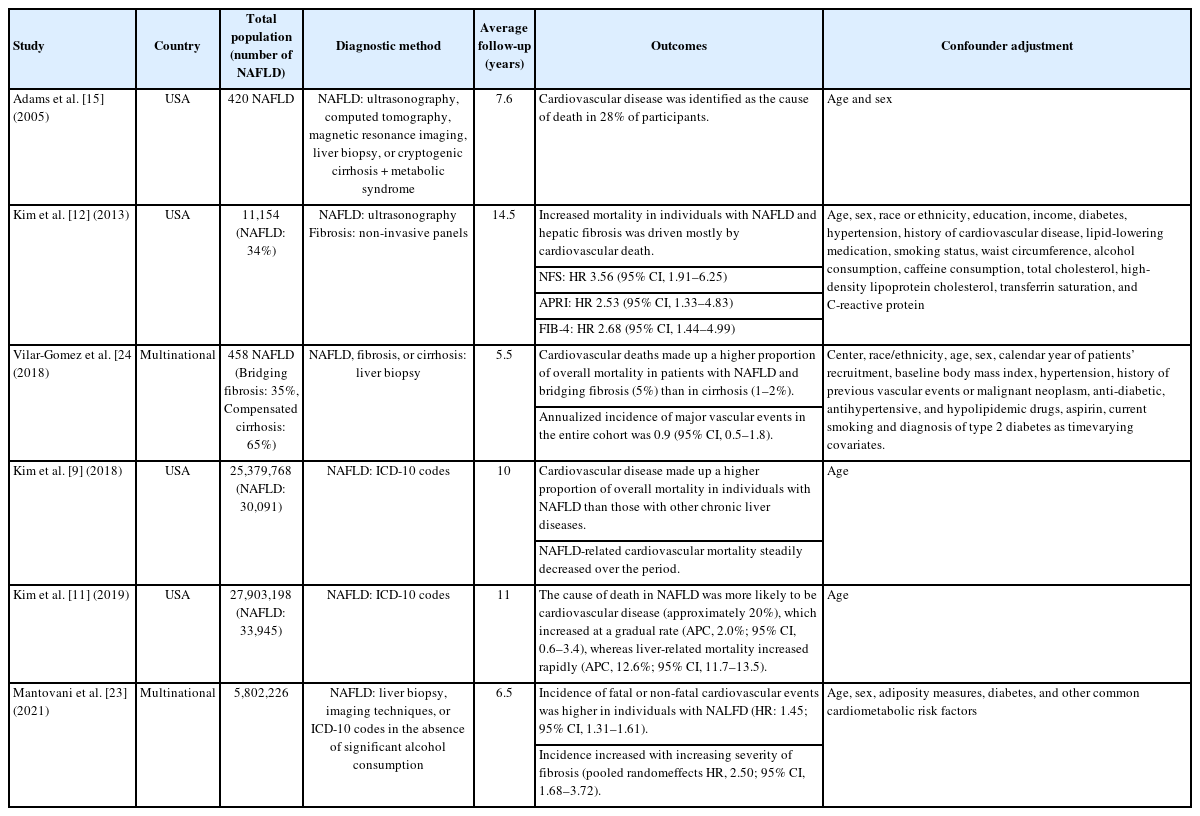
We summarized essential studies regarding all-cause mortality in individuals with NAFLD in Table 1. The first US community-based retrospective cohort study (n=435) of its kind showed there was a significantly lower survival for populations with NAFLD defined by ultrasonography or histology compared to the age- and sex-matched general population during 7.6 years of follow-up (77% vs. 87%, respectively, P<0.005) [15]. Several subsequent studies revealed similar results with a significant increase in all cause-mortality with ranges of the hazard ratio (HR) of 1.004–1.038 and standardized mortality ratio of 1.34–2.6 [16]. Although earlier studies showed that NAFLD was associated with a higher risk of allcause mortality compared to the general population of the same age and sex, it is unclear whether NAFLD-related liver disease is an independent risk factor, or if it is associated with the underlying metabolic abnormalities responsible for the increased risk of all-cause and cause-specific mortalities [17]. A US population-based study determined that NAFLD per se did not increase mortality risk after adjusting for multiple clinical and metabolic confounders beyond age and sex [12,13]. Consistent with these results, several studies have reported no significant difference in all-cause mortality in individuals with NAFLD [16,18,19]. Stratification by fibrosis using non-invasive panels was associated with a higher risk of all-cause mortality [12]. A Swedish nationwide, matched cohort study with 10,568 biopsy-confirmed NAFLD reported that significant excess mortality risk was noted in nonalcoholic steatohepatitis (NASH) without fibrosis (adjusted HR, 1.14; 95% confidence interval [CI], 1.03–1.26), non-cirrhotic fibrosis (adjusted HR, 1.26; 95% CI, 1.15–1.38) and cirrhosis (adjusted HR, 1.95; 95% CI, 1.75–2.18) compared with nonalcoholic fatty liver (simple steatosis) [20]. Dose-response association along with the severity of NAFLD was observed (P for trend <0.01) [20]. A recent meta-analysis showed that compared with no fibrosis (stage 0), the unadjusted risk increased with increasing stage of fibrosis (stage 0 vs. 4) with all-cause mortality relative risk (RR) of 3.42 (95% CI, 2.63–4.46) irrespective of the presence or absence of NASH [21]. The stage of fibrosis and rate of fibrosis development associated with mortality in NAFLD may be utilized as a predictor to differentiate between low-risk NAFLD and those that will progress to fibrosis or cirrhosis, which result in all-cause mortality. Therefore, better phenotyping of NAFLD may be needed to determine the relationship of NAFLD with all-cause mortality.
The recent trends in NAFLD-related all-cause mortality showed an initial linear increase, which then accelerated in recent years in the US [9,11]. Although the International Classification of Diseases 10th revision (ICD-10) code for NAFLD underestimated the true prevalence of NAFLD, the mortality due to NAFLD increased from an annual rate of 6.1% (95% CI, 4.5–7.8%) in 2007–2013 to 11.3% (95% CI, 6.3–16.6%) [9]. Compared with other racial/ethnic subgroups, non-Hispanic whites had higher mortality due to NAFLD [9]. NAFLD-related mortality increased continuously in Hispanics and non-Hispanic whites from 2007 to 2016, while mortality remained stable in non-Hispanic blacks [9]. A recent study showed that the attributable risk of NAFLD for all-cause mortality is 7.5% (95% CI, 3.0–12.0%), although the attributable risk of diabetes was 38.0% (95% CI, 13.1–63.0%) [22]. NAFLD-related mortality is expected to increase by 44% to 1.83 million annual deaths by 2030 in the US [10].
Cause-specific mortality in NAFLD
The leading cause of death in individuals with NAFLD is cardiovascular disease (summarized in Table 2), followed by extra-hepatic cancer and then liver-related mortality (summarized in Table 3) [12,15].
Cardiovascular mortality
NAFLD has been associated with an increased risk for the development of cardiovascular disease compared to those without NAFLD. A recent meta-analysis reported that NAFLD was associated with a moderately increased risk of fatal or non-fatal cardiovascular disease events (pooled HR, 1.45; 95% CI, 1.31–1.61) [23]. This risk markedly increased across the severity of NAFLD, especially the fibrosis stage (pooled HR, 2.50; 95% CI, 1.68–3.72) [23]. This effect is even more substantial with more advanced liver disease, especially with higher fibrosis stage, suggesting that the severity of NAFLD may independently predict risk for incident cardiovascular disease. Even relative to other causes of liver disease, such as viral hepatitis or ALD, the underlying cause of death in individuals with NAFLD is more likely to be cardiovascular disease. Though the independent association between NAFLD and increased cardiovascular mortality may be inconclusive, the underlying cause of death in individuals with NAFLD was more likely to be cardiovascular disease compared with other chronic liver diseases [9]. According to a study from the US national mortality data, the proportion of deaths due to cardiovascular disease in individuals with NAFLD was 16.2%, notably higher than that seen for those with HCV infection (10.3%), hepatitis B virus infection (7.2%), and ALD (5.0%) [7]. This is likely due to the fact that many of the comorbid metabolic abnormalities associated with NAFLD confer an increased risk of cardiovascular mortality. In particular, the accumulation of ectopic fat and resulting pro-inflammatory milieu work synergistically with associated dyslipidemia to accelerate the process of atherosclerosis. Among individuals with NAFLD, a high probability of advanced fibrosis by noninvasive markers was significantly associated with an increased risk of cardiovascular mortality (HR: 3.46, 95% CI: 1.91–6.25 for NAFLD fibrosis score; HR: 2.68, 95% CI: 1.44–4.99 for fibrosis-4 [FIB-4]; HR: 2.53, 95% CI: 1.33–4.83 for aspartate aminotransferase to platelet ratio index) [12]. A multi-national study with 458 biopsy-proven NAFLD with bridging fibrosis (n=159) or compensated cirrhosis (n=222) showed that NAFLD with bridging fibrosis had extra-hepatic cancers and cardiovascular events predominantly, while NASH cirrhosis had liver-related events predominantly [24]. Although all-cause mortality was significantly lower in NAFLD with bridging fibrosis, 50% of deaths were directly attributed to extrahepatic cancers or cardiovascular events. In contrast, patients with compensated cirrhosis were at significantly lower risk for non-liver-related deaths (12%) [24]. Therefore, it is essential to identify advanced fibrosis at increased risk of cardiovascular mortality among individuals with NAFLD.
Extra-hepatic cancer-related mortality
A Korean cohort study reported the association between NAFLD and incident cancer. During the follow-up of the median of 7.5 years, the cancer incidence rate in NAFLD was higher than that of non-NAFLD (HR, 1.32; 95% CI, 1.17–1.49) [25]. NAFLD was strongly associated with two extra-hepatic cancers: colorectal cancer in men (HR, 2.01; 95% CI, 1.10–3.68) and breast cancer in women (HR, 1.92; 95% CI, 1.15–3.20) [25]. A high probability of advanced fibrosis was associated with developing all cancers and HCC [25]. A US cohort study with age and sex-matched individuals with and without NAFLD reported that NAFLD was associated with a 90% increased risk of cancer [26]. The incidence of uterine, stomach, pancreas, and colon cancer was higher in those with NAFLD than those without [26]. Other cancers that have been demonstrated to have a higher incidence in those with NAFLD include male genital, female breast, and skin cancer in any gender [27]. Interestingly, NAFLD carries an independent association with an increased risk for cancer, while obesity alone does not [26]. NAFLD is associated with an increased risk for cancer-related mortality even outside the liver, and mortality due to extra-hepatic cancer is rising faster than any other cause of death in individuals with NAFLD at an annual percent change of 15.1% (95% CI, 13.0–17.2%) [11]. A recent meta-analysis reported that NAFLD was significantly associated with a 1.5–2 fold higher risk of incident gastrointestinal cancers (esophagus, stomach, colorectal, or pancreas) independent of age, sex, obesity, diabetes, smoking, or other potential confounders [28]. In addition, NAFLD was associated with a nearly 1.2–1.5-fold higher risk of incident lung, breast, urinary tract, or gynecological cancers [28]. Extra-hepatic cancer and cardiovascular mortality rates in NAFLD-related cirrhosis were more pronounced than in NAFLD without cirrhosis [11]. Though the mechanism of hepatic fibrosis facilitating carcinogenesis in the liver is well-described, how NAFLD and metabolic syndrome are associated with the development of extra-hepatic cancer is less well-understood. It is theorized that hepatic fat deposition results in the release of pro-inflammatory cytokines, leading to extra-hepatic tissue damage, remodeling, and immune cell dysfunction [29]. This theory partly explains why obesity in the absence of hepatic steatosis is not associated with an increased risk of cancer. However, future mechanistic studies are warranted.
Liver-related mortality
Individuals with NAFLD are at risk for progression to liver fibrosis and cirrhosis. This is especially true of the inflammatory subtype of NASH, which carries a 20% lifetime risk of progression to cirrhosis [30]. Prevalence of NAFLD-associated advanced fibrosis in the US has increased markedly in recent years, doubling from 3% in 2005–2006 to 6% in 2013–2016 [7]. Increased age, insulin resistance, and genetic polymorphisms may be associated with an increased risk for the development of fibrosis in individuals with NAFLD [31]. Liver fibrosis is one of the most important predictors of mortality in NAFLD, and liver-related mortality increases exponentially with the increasing fibrosis stage [32]. A recent meta-analysis showed that individuals with NAFLD and fibrosis were at an increased unadjusted RR of liver-related mortality and all-event liver morbidity compared with those with NAFLD and no fibrosis, and this risk was incremental according to the fibrosis stage [21]. Liver-related mortality included deaths due to compensated cirrhosis, complications of decompensated cirrhosis (ascites or bleeding esophageal varices, hepatic encephalopathy), acute on chronic liver failure, and/or HCC. A recent US national study showed that liver-related mortality among individuals with NAFLD was responsible for 58.9% of deaths in 2017, although liver-related mortality among those with NAFLD was lower than among those with other chronic liver diseases [11]. NAFLD-related liver mortality markedly increased in recent years with an annual percentage change of 4.9% (95% CI, 4.2–5.5%) during the recent decade [9].
In terms of cirrhosis-related mortality, there was an initial increase in cirrhosis due to HCV infection at a rate of 2.9% per year (95% CI, 2.3–3.5%) in 2007–2014, followed by a decrease in 2014–2016 at an annual rate of 6.5% (95% CI, –10.3% to –2.6%) after the introduction of direct-acting antiviral agents [33]. In contrast, mortality due to NASH cirrhosis increased with an average annual rate of 15.4% (95% CI, 14.1–16.7%) during the recent decade [33].
NAFLD is the fastest-growing cause of HCC in the world [34]. HCC risk associated with diabetes seemed to be highest in NAFLD, followed by ALD [35]. Based on dynamic modeling after accounting for current trends in diabetes and obesity, the annual incidence of NAFLD-associated HCC is projected to increase by 137%, from 5,160 cases in 2015 to 12,240 cases in 2030 [10]. A meta-analysis showed that the annual incidence of HCC was 0.44 per 1,000 person-years in those with NAFLD, and even higher in those with biopsy-proven NASH (5.29 per 1,000 person-years) [36]. In addition, HCC is an increasingly-recognized contributor to mortality in individuals with NAFLD, as metabolic syndrome and NAFLD cause almost 10% of cases of HCC in the world and 14.1% of cases of HCC in the US [37]. HCC usually arises in the background of cirrhosis, thought to be related to increased cell turnover from chronic inflammation leading to the formation of driver gene mutations. However, NAFLD and NASH are among the most common causes of HCC in the absence of cirrhosis [38]. HCC is the fourth leading cause of cancer-related mortalities globally, accounting for 810,000 mortalities in 2015 [39]. Globally, deaths from HCC increased by 60% from 1990 to 2013 [40], and HCC remained the second leading cause of years of life lost due to cancer from 2005 to 2015 [39]. In addition, HCC is a growing burden in individuals with NAFLD. A recent study based on the US National Vital Statistics System demonstrated an increase in the annual rate of HCV infection-related HCC mortality of 5.4% (95% CI, 3.6–7.4%) was noted from 2009 to 2014, followed by a decrease from 2014 to 2018 at a rate of 3.5% per year (95% CI, –5.9% to –1.1%) after the introduction of potent direct-acting antiviral agents [41]. In contrast, age-standardized mortality for HCC from NAFLD demonstrated a linear increase with an annual percentage change of 21.1% (95% CI, 16.9–25.4%) from 2009 to 2018 [41].
Diabetes-related mortality
Type 2 diabetes is common among individuals with NAFLD and NASH, with a global estimated prevalence of 22.5% (95% CI, 17.9–27.9%) and 43.6% (30.3–58.0%), respectively [36], compared to a contemporary US national prevalence of 14.3% (95% CI, 12.9–15.8%) [42]. This strong association reflects the overlapping pathogenesis of metabolic dysregulation shared between the two conditions. However, the relationship between type 2 diabetes and NAFLD is complex and may be bi-directional [43]. The global prevalence of NAFLD and NASH among individuals with type 2 diabetes was 55.5% (95% CI, 47.3–63.7%) and 37.3% (95% CI, 24.7–50.0%) [44]. A recent US population-based study showed that the prevalence of NAFLD by transient elastography was high in individuals with prediabetes (38.5–52.9%) and diabetes (70.7–82.1%) [45]. Significant fibrosis and cirrhosis were observed in about one-fourth of individuals with NAFLD and diabetes and one-sixth with NAFLD and prediabetes [45]. In the US general population, age-standardized mortality due to diabetes declined from 112.2 per 100,000 individuals in 2007 to 104.3 in 2017, with the decline of annual percentage change of –1.4% (95% CI, –1.9% to –1.0%) in 2007–2014 and stabilization of annual rate of 1.1% (95% CI, –0.6% to 2.8%) in 2014–2017 [46]. When looking specifically at individuals with NAFLD and diabetes, however, mortality in individuals with NAFLD increased at an annual rate of 11.6% (95% CI, 9.5–13.8%) during the same period [47]. Therefore, clinicians bear in mind the harmful impact of NAFLD among individuals with diabetes and vice versa.
HIGH-RISK PROFILES FOR MORTALITY IN NAFLD
As commented above, it is essential to identify and phenotype high-risk profiles at increased risk of all-cause mortality among individuals with NAFLD.
Genetic polymorphism
Outcomes of individuals with NAFLD are impacted by several associated factors, including genetic mutations such as polymorphisms in the patatin-like phospholipase domain-containing 3 (PNPLA3) gene. PNPLA3 encodes an enzyme involved in the hydrolysis of triglycerides, and mutations affecting its function have been associated with increased risk for the development of NAFLD, NASH, advanced fibrosis, and HCC [48]. PNPLA3 I148M polymorphism is more common among Hispanics, contributing to a higher incidence of advanced fibrosis and poorer outcomes from NAFLD compared with any other race/ethnicity [49]. PNPLA3 I148M polymorphism is associated with an earlier age of NAFLD, observation most pronounced in Hispanic Americans [50]. Earlier studies on the association between PNPLA3 I148M polymorphism and all-cause mortality have reported inconsistent results [51,52]. A US population-based study determined that individuals with NAFLD who are homozygous for the PNPLA3 I148M mutation are at increased risk of all-cause mortality as well as liver-related mortality when compared to those with NAFLD and wildtype PNPLA3 genotype during a follow up of 20 years [53,54]. Risk for cardiovascular mortality does not appear to be increased in individuals with PNPLA3 I148M polymorphism. A Chinese study with a mean age of 64 years showed that being homozygous for the PNPLA3 I148M mutation was independently associated with increased liver-related mortality (HR, 3.34; 95% CI, 1.01–11.17) but not associated with all-cause and cardiovascular mortality during 5.3 years follow-up [55]. Further studies are warranted to confirm these associations.
Low thyroid function and hypothyroidism
Low thyroid function, defined as higher levels of thyroid-stimulating hormone (TSH) level within the normal reference range of thyroid hormone (“low-normal” thyroid function and subclinical hypothyroidism), may cause adverse health effects similar to overt hypothyroidism. Hypothyroidism and low thyroid function are closely associated with increased risk for NAFLD, and a more advanced spectrum of NAFLD, including NASH, and significant fibrosis independent of clinical and metabolic risk factors [56-58]. A recent longitudinal study showed that increasing TSH levels during a median follow-up of 4 years were associated with incident NAFLD independent of other metabolic factors [59]. An US population-based study determined a strong association between NAFLD with increasing plasma TSH levels and all-cause mortality, mainly from cardiovascular mortality [60]. During the median follow-up of 23 years, low thyroid function was independently associated with an increased risk for all-cause mortality in individuals with NAFLD (HR, 1.24; 95% CI, 1.02–1.50), while this association was absent in those without NAFLD [60]. “Low-normal” thyroid function and subclinical hypothyroidism were significantly associated with an increase in the risk for all-cause mortality among individuals with NAFLD of 18% and 38%, respectively [60]. Low thyroid function was associated with cardiovascular mortality in individuals with NAFLD (HR, 1.62; 95% CI, 1.11–2.34). “Low-normal” thyroid function and subclinical hypothyroidism were significantly associated with a increase in the risk for cardiovascular mortality among individuals with NAFLD of 50% and 94%, respectively [60].
Sarcopenia
NAFLD and sarcopenia, which share various pathophysiologic mechanisms, have become increasingly prevalent conditions, resulting in a significant health burden [61]. Previous Asian studies determined sarcopenia is independently associated with NAFLD [62,63] and NAFLD-associated fibrosis [64]. A US population-based study showed an independent association between sarcopenia and NAFLD across various ethnicities [65]. During a median follow-up of 23 years, individuals with both NAFLD and sarcopenia had an increased risk for all-cause mortality (HR, 1.28; 95% CI, 1.06–1.55) compared with those without NAFLD and sarcopenia [66]. Sarcopenia was associated with an increased risk for all-cause mortality only in individuals with NAFLD after adjusting for advanced fibrosis, whereas this association was absent in those without NAFLD [66]. Other research is consistent with this finding [67,68]. Both NAFLD and sarcopenia confer increased risk for adverse outcomes mediated by a combination of additive and synergic risk factors for all-cause and cardiovascular-related mortality [61].
LIFESTYLE MODIFICATION IN NAFLD AND MORTALITY
Lifestyle modification is the staple of the management of NAFLD of any severity. Guidelines from both the American Gastroenterological Association and American Association for the Study of Liver Diseases on the management of NAFLD recommend lifestyle modification with a combination of physical activity (PA) and dietary modifications to achieve a weight loss of ≥5% of total body weight for NAFLD reduction, ≥7% for NASH resolution, and ≥10% for fibrosis regression/stability [69,70]. Though achieving weight loss is the most important predictor of improvement in NASH or fibrosis, adherence to a high-quality diet and sufficient PA have each been associated with improvement in NAFLD, even in the absence of weight loss [71,72]. Dietary modification includes restriction of caloric intake by 500–1,000 kcal as well as prioritization of foods low in carbohydrates and saturated fats, such as in the Mediterranean diet [69,70]. Higher diet quality was associated with significantly lower odds of NAFLD and a lower risk for all-cause mortality [3]. Clinicians focusing on primary prevention with high diet quality may be the ideal way to help curb the rising prevalence of NAFLD.
Practice guidelines recommend that individuals with NAFLD should achieve more than 150 minutes/week of moderate-intensity or more than 75 minutes/week of vigorous-intensity PA [70], which mirrors guideline recommendations for PA in the general population for the primary prevention of cardiovascular disease [73]. Although the prevalence of meeting the PA guidelines for leisure time increased in individuals without NAFLD from 2007 through 2016, the trends in meeting PA guidelines for any type of PA remained stable among those with NAFLD, with downtrends in transportation-related PA in the US [74]. Increasing PA beyond the amount recommended by PA guidelines may have an additional benefit to the management for NAFLD [74,75]. While 150–299 minutes/week of PA was associated with 40% lower odds of NAFLD, that risk reduction was 49% in those who achieved ≥300 minutes/week [75]. PA ≥300 minutes/week was also associated with 59% lower odds of fibrosis and 63% lower odds of cirrhosis [75]. Similar to diet quality, the level of PA has also been demonstrated to influence mortality. A recent US population cohort study with an average follow-up of 10.6 years showed that increasing duration of objectively-measured PA was associated with a reduced risk of all-cause mortality (P for trend <0.001) among individuals with NAFLD [76]. Furthermore, longer total PA was associated with a lower risk for cardiovascular mortality in individuals with NAFLD (P for trend=0.007) [76]. In summary, increasing PA has beneficial survival impacts on all-cause and cardiovascular mortality in individuals with NAFLD. Increasing PA in individuals with NAFLD should be recommended for its benefits on survival.
CONCLUSION
NAFLD is a highly prevalent and growing problem in the United States and worldwide. The overall incidence of the disease, as well as associated mortality rates, are continually increasing. While NAFLD per se may do not independently increase the risk for all-cause mortality, more severe NAFLD is associated with the underlying metabolic complications responsible for the increased risk of all-cause and cause-specific mortalities. The most common causes of death in individuals with NAFLD are cardiovascular disease, extra-hepatic cancer, liver disease (including decompensated cirrhosis and HCC), and diabetes. Mortality in NAFLD is further influenced by mutations in the PNPLA3 gene, low thyroid function, and sarcopenia. Weight loss through diet and PA is the recommended approach for NAFLD. Both diet and exercise have each been demonstrated to have significant effects on mortality, including all-cause and cardiovascular mortality. As the health burden of NAFLD increases, future studies may demonstrate an association between NAFLD and mortality, especially as more long-term mortality data is available that captures the downstream cardiovascular consequences of long-standing NAFLD and fibrosis.
Notes
Authors’ contribution
Dr. Peter Konyn was involved in the study concept and design, acquisition of data, interpretation of data, and drafting of the manuscript. Dr. Aijaz Ahmed and Dr. Donghee Kim were involved in the study concept and design, interpretation of data, drafting of the manuscript, critical revision of the manuscript, and study supervision.
Conflicts of Interest
The authors have no conflicts to disclose.
Abbreviations
ALD
alcohol-related liver disease
CI
confidence interval
HCC
hepatocellular carcinoma
HCV
hepatitis C virus
HR
hazard ratio
NAFLD
nonalcoholic fatty liver disease
NASH
nonalcoholic steatohepatitis
RR
relative risk
PA
physical activity
PNPLA3
patatin-like phospholipase domain-containing 3
TSH
thyroid-stimulating hormone