Co-development of autoimmune hepatitis and Sjögren's syndrome triggered by the administration of herbal medicines
Article information
Abstract
Autoimmune hepatitis (AIH) has been reported in association with Sjögren's syndrome (SS). Drug-induced AIH has been rarely reported. A rare case of the co-development of AIH and SS in a 53-year-old woman after the consumption of herbal medicines is described. After admission, the patient complained of dryness in her mouth, and she was subsequently diagnosed with SS, which had not been detected previously. The patient's bilirubin and aminotransferase levels initially decreased following conservative management; however, they later began to progressively increase. A diagnosis of AIH was made based on the scoring system proposed by the International Autoimmune Hepatitis Group. The patient was administered a combination of prednisolone and azathioprine, and the results of follow-up liver-function tests were found to be within the normal range. This is an unusual case of AIH and SS triggered simultaneously by the administration of herbal medicines.
INTRODUCTION
Autoimmune hepatitis (AIH) is a chronic necroinflammatory liver disorder that is characterized by hypergammaglobulinemia, presence of autoantibodies in serum, and presence of periportal hepatitis. It can be associated with a number of other autoimmune diseases, such as Sjögren's syndrome (SS), scleroderma, or systemic lupus erythematosus (SLE).
In persons genetically predisposed to AIH, environmental agents, such as viruses, certain drugs, and herbal agents, have been postulated to trigger a cascade of T cell-mediated events directed at liver antigens resulting in progressive liver injuries.1 Druginduced immune-mediated injury is an adverse immune response that affects the proteins in the liver and leads to AIH.2-4 Although an association of lupus-like syndrome or immunological responses with some chemical agents have been reported, the literature on herb-induced AIH mainly consists of case reports and a few very small case series.4,5
To our knowledge, co-development of AIH and other autoimmune diseases such as SS, triggered after the consumption of herbal medicines, has not yet been reported. Here, we report an unusual case in which AIH and SS developed simultaneously after the administration of herbal medicines.
CASE REPORT
The patient was a 53-year-old woman who presented to our hospital with a 10-day history of yellowish skin coloration. She took herbal medicines of unknown origin as health supplements for 4 weeks until 4 weeks before the development of jaundice. She was healthy, and her medical history was unremarkable. She was not prescribed of any medications and rarely consumed alcohol.
Her vital signs were unremarkable she denied travel history and past illness. Family history (including autoimmune disease) was not specific.
Laboratory tests revealed the following results: aspartate aminotransferase (AST) level, 1,136 U/L (normal range, 5-34 U/L); alanine aminotransferase (ALT) level, 1,415 U/L (normal range, 0-55 U/L); alkaline phosphatase (ALP) level, 203 U/L (normal range, 40-150 U/L); and total bilirubin, 8.5 mg/dL (normal range, 0.2-1.4 mg/dL). The findings of serologic tests for hepatitis A, B, and C viruses and tests for detecting other viruses, including Epstein-Barr virus, cytomegalovirus, and herpes simplex virus, were negative. The titer of antinuclear antibody was 1:320, with the antigen-antibody reaction showing a speckled pattern. The results of studies for autoimmune markers, including anti-smooth muscle, antimitochondrial, liver-kidney microsomal, anti-ds DNA, anticentromere, and anti-Scl-70 antibodies, were negative. The levels of anti-Ro and anti-La antibodies were 258 and 429 U/mL (normal range, <150 U/mL), respectively, and immunoglobulin G (Ig G) level was 2,347 mg/dL (normal range, 700-1,400 mg/dL).
Abdominal ultrasonography revealed slightly coarse echotexture of the liver parenchyma, indicating diffuse parenchymal disease. After admission, the patient complained of dryness in her mouth and foreign body sensation in her eye, which she had not experienced previously. Therefore, we performed a salivary gland scan and Schirmer's test. The salivary gland scan showed hot uptakes in both the salivary glands at 10 and 40 min and markedly diminished excretory function of both salivary glands. The Schirmer's test showed wetting of the paper by 2 mm in 5 min. We suspected primary Sjögren's syndrome (pSS) and administered conservative treatment. The results of liver function tests (LFTs) performed 21 days after admission revealed the following improved values: AST/ALT levels, 207/61 U/L; and total bilirubin level, 3.72 mg/dL. We first diagnosed the condition as drug-induced liver injury and performed follow-up evaluations in the outpatient department. The serum bilirubin and IgG levels obtained 10 days after this diagnosis repeatedly increased to 6.2 mg/dL and 3,039 mg/dL, respectively. We performed the liver biopsy for abnormal LFTs of unknown origin and biopsy findings showed interface hepatitis with moderate porto-periportal lymphoplasmacytic infiltration, periportal fibrosis, hepatic rosette formation and piecemeal necrosis (Fig. 1). There was no evidence of centrilobular zone 3 necrosis, suggestive of toxic hepatitis.
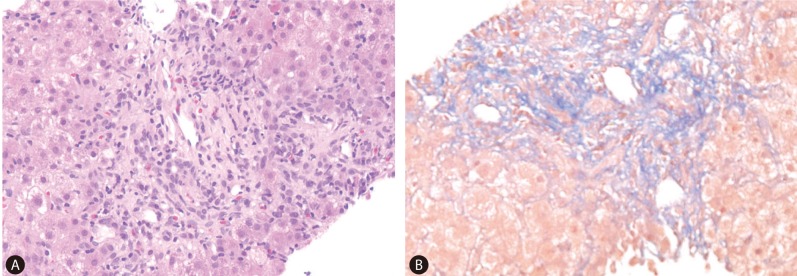
Liver biopsy showing moderate portoperiportal inflammation, periportal fibrosis, and piecemeal necrosis (magnification, ×40; (A) Hematoxylin-eosin staining, (B) Masson's trichrome staining.
On the basis of the scoring system proposed by the International Autoimmune Hepatitis Group and the Simplified Criteria for the Diagnosis of AIH, the scores for our patient's condition were 16 and 8, respectively, and she was diagnosed with AIH. Initially, she was administered 30 mg prednisolone and 50 mg azathioprine. Prednisolone dosage was tapered down to 10 mg for 2 weeks. Thereafter, her condition improved, and within 3 months after the treatment, the results of the LFTs were within the normal range. She has been receiving maintenance therapy with 10 mg prednisolone and 50 mg azathioprine for 1 year, and no complications have been observed during this period (Table 1).
DISCUSSION
Herbal products are associated with a wide spectrum of hepatic toxicities6 and have rarely been shown to cause or trigger AIH.6 However, it is unclear whether drugs and herbs unmask or induce AIH or simply cause drug-induced hepatitis with autoimmune features.1 In the previously reported small case series, the duration of follow-up was very limited, and hence, the long-term prognosis of patients remained uncertain.4 AIH by drug seems to result from idiosyncratic reactions,5 and it is postulated that reactive metabolites formed from the hepatic metabolism of some drugs bind to cellular proteins such as cytochrome P450 and are then recognized by the immune system as neoantigens.4
SS is a chronic systemic autoimmune disease characterized by lymphocytic infiltration of the exocrine glands, especially the lacrimal and salivary glands.7 The immunologic process in SS is characterized by B cell clonality that can be attributed to antigen-driven clonal expansion.8,9 SS can exist as a primary disorder or in association with other autoimmune processes.7 The mechanism underlying liver involvement in SS is not clear, but it is possible that damage to the hepatic and salivary glands shares a common pathology.7 Matsumoto et al reported that in patients with AIH, the lymphoplasmacytic infiltrate was predominantly composed of CD3+ T cells in both the liver and salivary glands.10
The co-development of diverse autoimmune diseases has been frequently reported.8 A nationwide survey in Japan indicated that SS is present in 10% of patients with AIH,11 although the exact prevalence of AIH in patients with pSS is unclear. Kocaman et al12 reported a case showing the symptoms and findings of pSS, cholestatic AIH, and latent autoimmune diabetes in adult (LADA) at the same time. In addition, the patient had experienced dry mouth and dry eyes for 6 months before the development of jaundice. However, the co-development of AIH and SS following herbal ingestion, as observed in this case, has been not reported. The concept of shared autoimmunity has been proposed on the basis of co-development of autoimmune diseases, although this concept still lacks molecular or genetic evidence.8
In our case, it is unclear whether the administration of herbal medicine to the patient directly led to the development of AIH and SS or it exacerbated some underlying autoimmune disorder that exhibited symptoms later. However, we believe that intake of herbal medicines may predispose the co-development of AIH and SS to some extent. In most previous studies on drug-induced AIH, particularly those involving minocycline and nitrofurantoin, patients had consumed the drugs for a number of months before AIH was observed.6 In our case, the patient had consumed the herbal medicine only for 4 weeks before she noticed yellow coloration of her skin. This suggests that the drug effects, if any, started very shortly after the patient started consuming the herbal medicine. This is an unusual occurrence, although in a few cases of AIH resulting from the consumption of herbal medicine, the patients had consumed herbal medicine for approximately 3-4 weeks.5,6 Therefore, it is more likely that the patient had an underlying autoimmune liver disease in addition to subclinical SS, because liver disease in patients with pSS is subclinical.13 In addition, considering the portal fibrosis observed on liver biopsy and the relatively short duration of herbal medicine consumption, although our patient had no previous history of autoimmunity, it can be speculated that herbal medicine might have triggered an underlying autoimmune disorder and revealed the clinical menifestations of them. However, we could not confirm the ingredients of ingested herb in this patient.
Liver disease in patients with pSS, especially in patients with jaundice, should be treated at the earliest.13 AIH patients with severe interface hepatitis showed a good response to immunosuppressive therapy.13 In most cases of drug-induced AIH, it is possible to stop all steroid/immunosuppressive drug treatment without any disease relapses. Therefore, we believe that our patient will have better prognosis than others.
In the future, for patients with herbal medicine-induced liver injury, the possibility of an accompanying autoimmune disorder such as SS, and/or AIH should be considered, and a careful follow-up should be conducted even if the liver function tests show improvement in the initial stages.
Acknowledgements
This paper was supported by Wonkwang University in 2013.
Notes
The authors have no conflicts to disclose.
Abbreviations
AIH
Autoimmune hepatitis
SS
Sjögren's syndrome
