Focal type of peliosis hepatis
Article information
INTRODUCTION
Peliosis hepatis is a benign disorder, histologically characterized by blood-filled cystic cavities of various sizes and irregular shapes, communicating with the hepatic sinusoids and associated with rupture of the reticulin framework. This entity is rare, but as the use of modern cross-sectional imaging studies increases in the medical practice, it is more frequently encountered than before. While it has been described that the lesions typically involve the entire liver in the past, focal type of peliosis hepatis has been increasingly reported recently. In this article, we present imaging findings in a case of focal peliosis hepatis, which mimicked the other hepatic tumors or inflammatory masses.
CASE REPORT
An asymptomatic 31-year-old female patient presented with incidentally found liver mass on screening sonography. Her clinical history did not include any specific disease, family history was unremarkable, and physical examination was unremarkable. She denied abuse of drug or alcohol. She didn't intake steroids or oral contraceptives. The results of routine laboratory investigations were unremarkable; hemoglobin, 13.9 g/dL; leukocyte count, 8,000/mm3; platelet count, 274,000/mm3; total protein 6.6 g/dL; albumin, 4.2 g/dL; total bilirubin, 0.5 mg/dL; aspartate aminotransferase, 17 IU/L; alanine aminotransferase, 13 IU/L; gamma-glutamyl transpeptidase, 17 IU/L. Serologic tests for hepatitis A, B, and C were negative. Tumor markers including AFP, CEA, and CA 19-9 were all within normal ranges.
Abdominal sonography showed about 3 cm, oval shape mass-like lesion with heterogeneous echogenicity in the right hepatic lobe (Fig. 1A). Otherwise, echogenicity and echotexture of the background liver was unremarkable. Doppler study revealed no hypervascularity of the lesion and no remarkable perilesional hemodynamic abnormality. CT scans were obtained for further evaluation of hepatic mass. On noncontrast CT, the lesion showed mild low density compared with adjacent parenchyma (Fig. 1B). Liver density was normal, with no evidence of hepatic steatosis or iron overload. On contrast-enhanced CT during the hepatic arterial phase, the lesion showed lack of enhancement and an irregular and infiltrative margin (Fig. 1C). Most part of the lesion demonstrated isoattenuating enhancement with adjacent liver on venous phase, except small branching tubule-like low attenuation in the center (Fig. 1D). There was no evidence of portal thrombophlebitis or bile duct dilatation around the lesion. The radiological differential diagnoses were in wide range, including organizing abscess, sclerosing hemangioma, and hypovascular hepatic malignancy such as cholangiocarcinoma or metastasis.
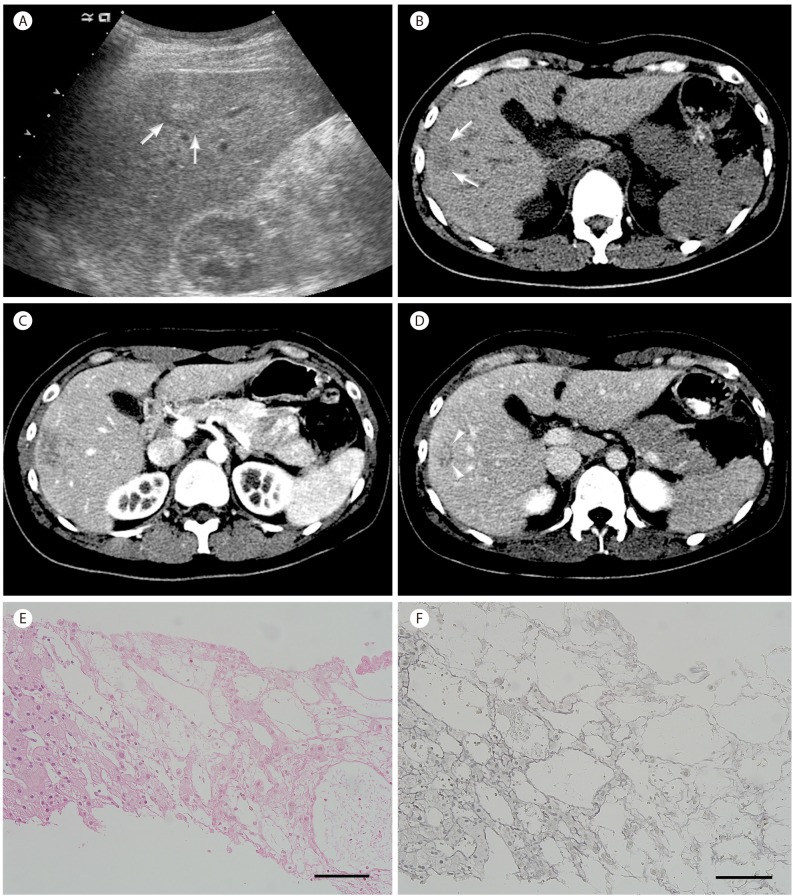
Focal type of peliosis hepatis in a 31-year-old female patient. (A) Oblique coronal sonogram obtained by intercostal scan shows about 3 cm ovoid mass-like lesion (arrows) in right hepatic lobe. The lesion shows heterogeneous echogenicity and the boundary from the adjacent parenchyma is relatively well-defined in part but ill-defined in general. (B) On noncontrast CT, the lesion shows mild low density (arrows) compared with adjacent parenchyma. (C) The lesion shows irregular and ill-defined margin and paucity of enhancement on contrast-enhanced CT during hepatic arterial phase. (D) On venous phase, most part of lesion demonstrates isoattenuating enhancement with adjacent liver, except small branching tubule-like low attenuation in the center (arrowheads). There is no thrombophlebitis or bile duct dilatation associated. (E) Marked sinusoidal dilatation and thinning of hepatic cell cords are observed on the right (Original magnification×20 objective lens, scale=100 µm). (F) Reticulin framework is lost in affected area (on the right), leading to the diagnosis of peliosis hepatis (Original magnification×20 objective lens, scale=100 µm).
Percutaneous biopsy was performed under sonographic guidance. Histopathologic examination revealed localized marked dilatation of sinusoids forming blood-filled spaces and thinning of hepatic cell cords (Fig. 1E) and reticulin fiber network was lost in the affected area leading to the diagnosis of peliosis hepatis (Fig. 1F). The dilated sinusoidal cells were negative for CD 34, but were positive for factor VIII (not shown), further supporting the diagnosis of peliosis hepatis.
The patient was discharged after the biopsy and was found to stay in good health at the recent follow-up (> 2-year period). There lesion didn't progress or regress on follow-up imaging studies (not shown).
DISCUSSION
The etiology or pathogenesis of peliosis hepatis remains unclear. It has been reported previously that this entity is diffuse, frequently related to debilitating underlying diseases, chronic alcoholism, intravenous drug abuse, or long-term use of anabolic steroids or oral contraceptives.1 However, as the use of modern cross-sectional imaging studies increases even in the asymptomatic population for the purpose of health care, more and more cases of focal peliosis hepatis are incidentally found nowadays in subjects with no underlying diseases or possible predisposing factors.23
Radiologic findings of focal peliosis hepatis may vary depending on the size of the lesion, the presence or absence of thrombus and hemorrhage within the cavities. A recent study has shown that dynamic enhancement patterns of focal peliosis hepatis may vary depending on the pathological findings.4 In their study, hypervascular enhancement mimicking hepatocellular carcinoma or hypervascular metastasis could be appreciated on the arterial phase of dynamic CT or MRI when there was fresh and actively circulating blood within the dilated sinusoid. In contrast, when there was old and stagnated blood within the spaces in conjunction with hepatocyte degeneration or atrophy, dynamic studies tended to show persistently low or slow centripetal enhancement of the lesion on portal or delayed phase images, similar as in our case. In such circumstances, the lesion should be differentiated from atypical hypovascular malignant hepatic tumors such as cholangiocarcinoma, epithelioid hemangioendothelioma, or metastasis especially in patients with underlying malignancy. In addition to the absence of suggestive findings of such tumors (e.g. accompanying bile duct dilatation, multinodular coalescent appearance, capsular retraction, and peripheral ring-like enhancement during the arterial phase), an ill-defined, irregular, non-tumefactive margin and the lack of mass effect can be differential points suggestive of peliosis hepatis. Moreover, the late iso-attenuating enhancement in our case, representing the venous pooling at the dilated sinusoids, may be another clue for the diagnosis of peliosis hepatis.5 However, this finding should be cautiously differentiated from the slow progressive enhancement in the sclerotic stroma of hypovascular malignant tumors. Similar enhancement patterns can be also appreciated in some benign hepatic lesions with abundant sclerosis such as sclerosing hemangioma and organizing abscess, and these entities should be also included in the differential diagnosis.
The definitive diagnosis of peliosis hepatis is established by histopathology. Therefore, a percutaneous needle biopsy can be used to confirm the diagnosis, if peliosis hepatis is suspected on the imaging studies. As peliosis hepatis may present with a broad spectrum of potentially misleading findings on imaging studies, a high level of suspicion is a prerequisite for the diagnosis. Peliosis hepatis should be suspected when an incidental focal liver lesion shows no specific findings that clearly favor the diagnosis of the common hepatic tumors and tumor-like lesions. Non-tumefactive margin, the lack of mass effect, and late iso-attenuating enhancement during the venous or delayed phase on dynamic post-contrast study may further raise the suspicion. Establishing the diagnosis with biopsy, then the management and monitoring of the lesion can be tailored based on the location and extent of the lesion, the damage to liver function, and the presence or absence of complications.
SUMMARY
Although peliosis hepatis is a rare entity, it is increasingly found as a focal liver lesion in the routine practice with the popular use of modern cross-sectional imaging studies. As peliosis hepatis may present with a broad spectrum of potentially misleading findings on imaging studies, a high level of suspicion is a prerequisite for the diagnosis. Peliosis hepatis should be suspected when the imaging findings of an incidental focal liver lesion do not favor the diagnosis of the common hepatic tumors and tumor-like lesions. Non-tumefactive margin, the lack of mass effect, and late iso-attenuating enhancement on dynamic post-contrast study may further raise the suspicion.
Notes
Conflicts of Interest: The authors have no conflicts to disclose.
Abbreviations
CT
computed tomography
AFP
α-fetoprotein
CEA
carcinoembryonic antigen
CA
carbohydrate antigen
MRI
magnetic resonance imaging