Massive hepatic necrosis with large regenerative nodules
Article information
INTRODUCTION
Massive hepatic necrosis (MHN) is characterized by extensive panlobular and multilobular hepatocyte necrosis, and is the morphological counterpart of acute fulminant liver failure.1 Histopathologic examination of explanted liver specimens reveals a wide spectrum of morphological changes in the parenchyma, from areas of extensive hepatocyte loss and parenchymal collapse to areas of hepatocytic regeneration with the appearance of regenerating nodules. The latter may be exaggerated to the extent that they are macroscopically identifiable and even simulate neoplastic lesions. In this issue, we will discuss the histopathologic findings of MHN based on a case of a 40-year-old patient.
CASE SUMMARY
A 40-year-old previously healthy female was referred to a tertiary care center for emergency liver transplantation. She had visited a local clinic complaining of fatigue for the past two months and abdominal discomfort for three days. She had no recent history of drug or alcohol ingestion or traveling. Initial AST and ALT levels were 600 IU/L and 700 IU/L, respectively. In spite of conservative treatment, her bilirubin level rose continuously and signs of hepatic encephalopathy developed.
The initial laboratory data were as follows: WBC count 14,510/ul, hemoglobin level 10.6 g/dL, platelet count 74,000/ul, prothrombin time (PT) 44.3 seconds, blood urea nitrogen (BUN) 8.3 mg/dL, creatinine 0.73 mg/dL, total protein 7.2 g/dL, albumin 4.8 g/dL, aspartate aminotransferase (AST) 192 IU/L, alanine aminotransferase (ALT) 133 IU/L, total bilirubin 41.9 mg/dL, direct bilirubin 29.4 mg/dL, and ammonia 172 ug/dL. Serologic markers for HBsAg, IgM anti-HBc, IgM anti-HAV, and anti-HCV were negative. Tumor markers and auto-antibodies were also negative.
Abdominal computed tomography demonstrated a mixture of necrotic or fibrotic areas and areas of normal liver parenchyma, suggestive of fulminant hepatitis. Magnetic resonance image showed a lobulated contour of the liver with uneven arterial and portal supply, consistent with acute hepatitis.
Orthotopic liver transplantation was performed at 2 months after the onset of the abdominal discomfort. The patient is currently being followed up in the outpatient clinic, with improved general conditions and no specific complaints.
PATHOLOGIC FINDINGS
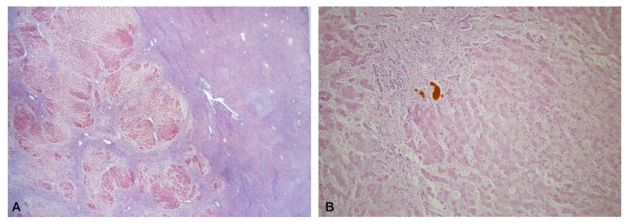
The explanted liver weighted 604 g and measured 22×14×4 cm (Fig. 1). The Glisson's capsule was smooth and the liver was soft on palpation. The posterior surface showed focal pale yellow to green discolorization with areas of bulging. On sections, the parenchyma showed multiple yellow-green variable-sized soft nodules, the largest one measuring 4.5 cm in maximum dimension, separated by more homogeneous reddish-brown areas. On microscopic evaluation, extensive hepatocytic necrosis, lobular collapse, and hemorrhage were seen throughout the liver parenchyma. These features were especially prominent in the perivenular zones, with central venulitis and marked ductular proliferation (Fig. 2A-C). The ductular reaction was positive for EpCAM expression, consistent with proliferation of a hepatic stem/progenitor cell compartment (Fig. 2D). Nodules of regenerating hepatocytes were seen in some areas (Fig. 3A), surrounded by ductular reaction. Ductular cholestasis and macrophage infiltration were also prominent (Fig. 3B). Occasional small regenerating hepatocytes at the edge of the nodules were positive for EpCAM expression (Fig. 3B, inset). The larger nodules were relatively well demarcated from the surrounding parenchyma without definite fibrous capsules (Fig. 4A, B) and were composed of coalescing islands of regenerating hepatocytes. Normal lobular architecture, including portal tract structures, were not seen in the nodules, and hepatocellular atypia was absent.

Gross appearance of massive hepatic necrosis. Two representative sections of the explanted liver show a bulging contour formed by yellow-green soft nodules. The regenerative nodules are surrounded by reddish-brown hemorrhagic parenchyma (black dotted lines).
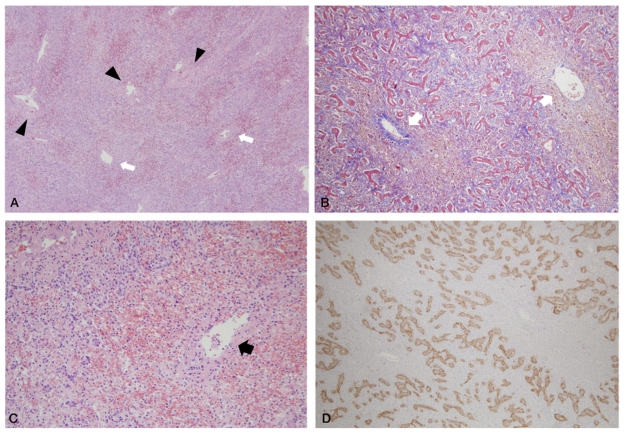
Histologic features of areas of extensive hepatocyte necrosis (A. H-E, ×40, B. Masson's trichrome, ×100, C. H-E, ×200). Complete loss of hepatocytes is seen, with preservation of the basic lobular architecture (black arrowheads: portal tracts, white arrows: central veins) and hemorrhage in the collapsed areas. Prominent ductular reaction is present, and the ductular reaction is positive for EpCAM expression by immunohistochemistry (D. EpCAM, ×100).
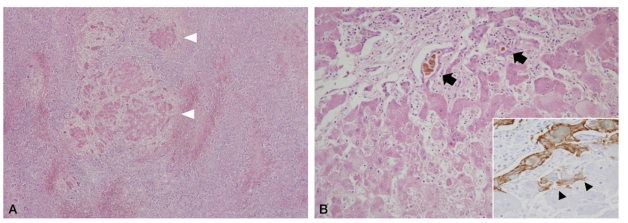
Small islands of regenerating hepatocytes are seen (white arrowheads) in the background of diffuse liver cell necrosis (A. H-E, ×40). Higher power magnification shows regenerating hepatocytes with hepatocellular cholestasis, Kupffer cell hyperplasia and ductular cholestasis (black arrows). Occasional small regenerating hepatocytes are positive for EpCAM (B. H-E, ×200, inset: EpCAM, ×400).
DISCUSSION
The etiologies of acute fulminant liver failure include acute viral hepatitis, drugs or toxins, autoimmune hepatitis, metabolic diseases, vascular diseases, and malignancies. Acute viral hepatitis is the most common and important cause of acute fulminant liver failure worldwide.1 Its prognosis varies according to the underlying etiology; for example, patients with acute hepatitis A have a more favorable outcome compared to those with acute hepatitis B, autoimmune hepatitis or Wilson's disease.2
The morphological features of MHN depend on the length of time elapsed between the insult and time at histologic examination, the etiology of the MHN, and whether the injury is solitary, repeated, or continuous.1 In general, the reticulin framework remains largely intact, and the dropout of the hepatocytes results in the shrinkage of the parenchymal mass. The liver subsequently shrinks and softens, and the capsule becomes wrinkled.3 Microscopically, the characteristic features of MHN include extensive hepatocyte loss, ductular reaction around portal tracts, inflammatory cell infiltration, and collapse of the reticulin framework. Hemorrhage in the collapsed zones may be prominent. Inflammatory cell infiltration is variable in degree, and the main infiltrating cells are macrophages, which are frequently ceroid-laden. Venulitis of central veins can be seen. The ductular reaction is believed to represent the proliferation of a hepatic stem/progenitor cell compartment and is most prominent in the periportal zone.4 The ductular cells are bipotential cells that can differentiate into both hepatocytic and cholangiocytic lineages, and have been demonstrated to be an important source of hepatocyte regeneration, both in acute liver injury (e.g. MHN) and in chronic liver diseases (e.g. cirrhosis). In less severe forms of MHN, there may be residual patches of hepatic parenchyma, which have been not affected by the noxious process.
With recovery, scattered hepatocyte islands appear in the collapsed areas and form regenerative nodules which lack a true lobular architecture. These are newly formed hepatocytes that eventually will form a normal lobular pattern.5 Macroscopically identifiable regenerative nodules may subsequently appear, characterized by tan to yellow-green nodules of regenerating parenchyma which are surrounded by more hemorrhagic or necrotic areas.3 Owing to the considerable chronological and spatial heterogeneity in the degree of parenchymal damage or regeneration in MHN, the diagnosis of MHN may be hindered on needle biopsy specimens. The diagnosis may be even further complicated by the appearance of large regenerative nodules during the healing process of MHN. These nodules are -it should be noted- different from the large regenerative nodules of cirrhotic livers which are larger than the surrounding regenerative nodules but have the same histological characteristics of regenerative nodules. They should also be differentiated from other benign and malignant hepatic nodules, including focal nodular hyperplasia, hepatocellular adenomas, and well-differentiated hepatocellular carcinomas. The absence of hepatocellular atypia, the architectural features, careful examination of the surrounding hepatic parenchyma, and thorough clinico-radiological correlations are important aids to the differential diagnosis.