Treatment and clinical outcome of needle-track seeding from hepatocellular carcinoma
Article information
Abstract
Background/Aims
Needle-track seeding is a rare but important complication of diagnostic and therapeutic ultrasound (US)-guided procedures in hepatocellular carcinoma (HCC). We examined the frequency of needle-track seeding after US-guided percutaneous ethanol injection (PEI), fine-needle aspiration biopsy (FNAB), and percutaneous transhepatic biliary drainage (PTBD) in order to determine the appropriate treatment for needle-track seeding and its clinical outcome.
Methods
We analyzed the clinical characteristics and treatment outcomes in eight patients who experienced needle-track seeding from HCC after an US-guided procedure (FNAB, PEI, or PTBD) between January 1990 and July 2004.
Results
Seven (0.14%) of 5,092 patients who experienced needle-track seeding (2 after PEI, 4 after FNAB, and 1 after PTBD) during the study period and 1 other patient who experienced needle-track seeding recently were recruited for this study. Two of the eight patients underwent mass excision and the other six patients underwent en-bloc wide excision for the needle-track seeding. Tumors recurred in the needle-tracks in both patients who underwent mass excision but not in the six patients who underwent en-bloc wide excision. Mortality occurred in three patients who experienced the recurrence and progression of intrahepatic HCC.
Conclusions
The incidence of needle-track seeding after US-guided procedures in HCC was 0.14%. En-bloc wide excision seems to be the optimal treatment for minimizing the probability of tumor recurrence due to needle-track seeding.
INTRODUCTION
Hepatocellular carcinoma (HCC) is a common malignancy in Asia, where chronic hepatitis B and C infections are endemic. Furthermore, HCC constitutes more than 5% of all cancers and is the dominant cause of death in patients with compensated cirrhosis,1,2 and its incidence is increasing globally, especially in the West.3
Ultrasound (US)-guided procedures are useful and versatile tools for the diagnosis and treatment of HCC, and have become increasingly popular since the late 1980s.4 US-guided fine-needle aspiration biopsy (FNAB) is a widely accepted and minimally invasive technique for the cytological or histological diagnosis of HCC and is considered a safe and accurate method.4,5 Percutaneous ethanol injection (PEI) is a safe and effective treatment modality in small HCC.6 Percutaneous transhepatic biliary drainage (PTBD) is a useful procedure required in case of the obstructive jaundice due to bile duct invasion by HCC.7 Although many complications have been reported to be associated with these procedures, the majority can be treated conservatively, with the notable exception of needle-track seeding.8 However, needle-track seeding is rare after PEI or FNAB; reported incidences range from 0.65 to 2.2%9,10 and from 1.5 to 5.8%,11 respectively. It has not been previously reported after PTBD (although tumor cell seeding has been reported along a catheter track in a patient with cholangiocarcinoma12). Because of the rare incidence of needle-track seeding in HCC, the treatment options and prognosis of the needle-track seeding have not been properly addressed.
We performed this study to examine the frequency of needle-track seeding after US-guided procedures such as PEI, FNAB, and PTBD in HCC, and to determine the appropriate treatment for the needle-track seeding. In addition, we investigated the clinical courses in patients with the needle-track seeding from HCC.
PATIENTS AND METHODS
Patients
We retrospectively analyzed the computerized medical records of 5,092 patients who underwent PEI (1,549 patients), FNAB (3,391 patients), or PTBD (152 patients) for HCC between January 1990 and July 2004 at Seoul National University Hospital. The study protocol was reviewed and approved by Institutional Review Board of Seoul National University Hospital.
Ultrasound-guided technique
Under US guidance (SSD-680 ultrasound scanner, Aloka, Tokyo, Japan, equipped with 3.5-MHz convex-array transducer), PEI and FNAB were performed using a 20-gauge needle with a closed conical tip, 3 terminal side holes (Gallini, Mirandola, Italy) and a biopsy device (Autovac Gun, Angiomed, Karlsruhe, Germany, equipped with 18 or 21-gauge needles) respectively. PTBD was performed with an 8.5 Fr DM catheter (Cook, Winston-Salem, USA) under USG and fluoroscopic guidance.
Data and image analysis
We retrospectively analyzed the medical records of patients who experienced needle-track seeding and collected the following data: age, gender, hepatitis viral marker, size of implanted nodule and primary HCC at the time of the first US-guided procedure, time interval from the US-guided procedure to the detection of implanted nodule, the extent of implanted nodule, the procedure involved, intrahepatic recurrence, method of nodule excision, degree of histologic differentiation of HCC, time interval from nodule excision to the last follow-up (in case of the recurrence of needle-track seeding, from nodule excision to detection of the recurrence), and survival. Association between these factors and recurrence after surgical excision were analyzed using Fisher's exact test.
The locations of nodules were confirmed and their sizes were measured by physical examination and triple-phase helical computed tomography (CT). Patients underwent en-bloc wide excision or mass excision based on surgeon's judgment. En-bloc wide excision was defined as the resection of implanted nodule with surrounding tissues such as, skin, subcutaneous tissue, muscles, and/or ribs. Mass excision was defined as removal of the implanted nodule only. The diagnosis of needle-track seeding was confirmed with the pathologic proof of metastatic HCC after excision.
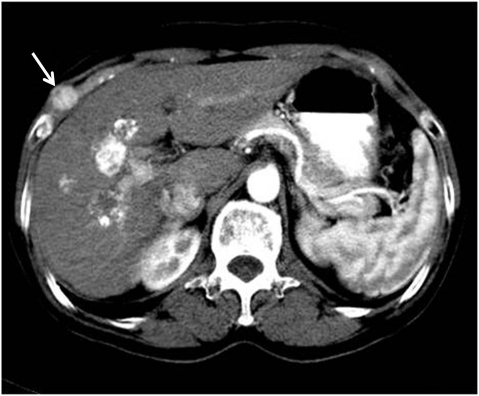
RESULTS
Two (0.13%) of the 1,549 patients who underwent PEI, 4 (0.12%) of the 3,391 who underwent FNAB, and one (0.66%) of the 152 patients who underwent PTBD for HCC experienced needle-track seeding during the study period. In addition, we also recruited one patient with needle-track seeding after PEI transferred from other hospital. Therefore, total 8 patients with needle-track seeding were enrolled (mean age, 48.5 years; range, 32-60 years). Table 1 summarizes the baseline characteristics of the enrolled patients. Seven tumors occurred in the right hepatic lobe and one tumor in the left hepatic lobe. All of 8 patients had well-preserved liver function (Child-Pugh-Turcotte [CPT] score≤6) and no history of variceal bleeding, ascites, or encephalopathy. The size of tumors at the time of PEI, FNAB, or PTBD ranged from 2.5 to 8 cm (mean size, 4.0 cm). Hepatitis B virus surface antigens were detected in 6 patients, but no serologic marker for viral hepatitis was detected in the other two patients. Implanted nodules were detected 7 to 45 months (median; 10.5 months) after the procedures. The size of implanted nodules ranged from 1 to 4 cm (mean; 2.4 cm, maximal diameter) at first excision. The skin was involved in four patients (Fig. 1, 2).

Baseline characteristics, treatments, and outcomes of eight patients with needle-track seeding from hepatocellular carcinoma
Table 1 also summarizes the methods of surgical excision, the pathologic results, and the clinical outcomes in 8 patients with needle-track seeding. Six patients underwent en-bloc wide excision while other two patients underwent mass excision to manage needle-track seeding. Median follow-up after surgical excision was 43.8 monts (range 8-108 months). While no recurrence of needle-track seeding was observed in six patients who underwent en-bloc excision, other two patients who underwent mass excision experienced the recurrence of needle-track seeding after surgery. The implanted nodules at the time of first excision in these two patients who experienced the recurrence after surgery were smaller (1 cm) than those in other six patients who did not experienced the recurrence. One of these two patients had hepatitis B surface antigen and no skin involvement. This patient underwent en-bloc wide excision for the recurred implanted nodule and no intra or extra hepatic recurrence occurred during the study period. The other patient had no serologic markers for viral hepatitis and had skin involvement. The pathologic result of this patient revealed combined hepatocellular-cholangiocarcinoma. This patient did not receive any treatment for recurrence in our institution due to loss of follow-up. Because 8 of 5,092 patients had the pathologic results with combined hepatocellular-cholangiocarcinoma during the study period, the frequency of needle-track seeding in this subgroup with combined hepatocellular-cholangiocarcinoma was 12.5% (one of eight patients).
Method of surgical excision, that is, en-bloc wide excision versus mass excision, was found to be significantly (P=0.036) associated with recurrence. On the other hand, Other factors such as age, gender, the presence of viral markers, the size of implanted nodule and primary HCC, the extent of implanted nodule, US-guided procedure used, time interval from the US-guided procedure to the detection of implanted nodule and intrahepatic recurrence were not found to be significantly associated with the recurrence of needle-track seeding. Degree of differentiation of the primary tumor could only be analyzed for seven of the eight patients, due to a lack of information on one, but was not found to be significantly associated with recurrence.
During the study period, mortalities occurred in three patients (Table 1). These three patients received en-bloc wide excision for needle-track seeding and did not experience the recurrence after surgical resection. However, intrahepatic HCC recurred and progressed in these three patients during the study period. The patients died due to HCC progression and hepatic failure. Among two patients who experienced the recurrence of needle-track seeding after mass excision, one patient did not experienced further recurrence of needle-track seeding after repeated surgical treatment (en-bloc wide excision) and was alive by the end of the current study. Clinical outcome of the other patient who had combined hepatocellular-cholangiocarcinoma could not be evaluated due to follow-up loss.
DISCUSSION
In the current study, the incidence of needle-track seeding from HCC after a US-guided procedure (FNAB, PEI and PTBD) was 0.14% (7 of 5,092 patients) and the incidence of implanted nodule recurrence after surgical excision was 25% (2 of 8 patients). Two patients who had undergone only mass excision instead of en-bloc wide excision experienced the recurrence of needle-track seeding after surgical excision. One of these underwent en-bloc wide excision for the recurred implanted nodule and experienced no further recurrence of needle-track seeding during the study period.
Biliary peritonitis, intra-and extrahepatic tumor seeding, and intrahepatic hematoma are the most serious complications of PEI, FNAB, and PTBD in HCC.13-17 Complications after FNAB and PEI are rare, with reported incidences of 2.4% and 0.05-0.18% and mortality rates of 0.1% and 0.006-0.031%, respectively.14,16,18-20 However, the overall complication rate after PTBD is higher with an incidence of 3.4-5%.21 In the current study, two (0.13%) of the 1,549 patients who underwent PEI, four (0.12%) of the 3,391 patients who underwent FNAB, and one (0.66%) of the 152 patients who underwent PTBD for HCC experienced needle-track seeding. Silva et al in a systematic review and meta-analysis of eight observational studies found that the incidence of needle-track seeding after FNAB varied widely from 0-5.8%.11 As compared with previous reports, rates of needle-track seeding after PEI and FNAB were slightly lower in the current study. The number of patients in the current study was much larger than the previous observational studies, which would contribute to lower incidence in the current study due to the abundant experience.
The mechanism of needle-track seeding from HCC is probably complex and several causes have been discussed.22 In animal models, Ryd et al found that FNAB can implant 103-105 cells along a single needle-track.23 Tumor size and degree of histologic differentiation, number of needle passes, the difference in the number of needle passes and the obtained specimens, the thickness of liver parenchyma along needle-tracks, and needle type have all been considered factors of needle-track seeding after FNAB in HCC.24-29 Kim et al reported that the number of needle passes seemed to affect the frequency of needle-track seeding and suggested that the life expectancies of patients influence the frequency of needle-track seeding more significantly than the size or degree of differentiation of HCC.26 In addition, many cases of needle-track seeding after PEI have been reported.9 Di Stasi et al reported that tumoral seeding after PEI occurs for deeply located and small HCCs, but found no relation between seeding risk and HCC cytology.9
No report has been issued on the recurrence of needle-track seeding and the factors associated to the recurrence in HCC. In the current study, the recurrence rate of needle-track seeding was 25% among our eight patients at a median follow-up of 43.8 months. And we found that only the method of excision for implanted nodules was significantly associated with recurrence while other factors were not; no patients who had undergone en-bloc wide excision experienced the recurrence of needle-track seeding. Furthermore, our findings show that PTBD, like PEI and FNAB, can cause needle-track seeding.
Nevertheless, despite the risks of needle-track seeding, PEI, FNAB and PTBD are useful tools for diagnosing and treating HCC, because it appears that needle-track seeding does not exacerbate the disease course. Several studies have reported that the prognosis of needle-track seeding from HCC after PEI or FNAB is favorable and similar to that of patients who do not develop seeding, although these studies concerned clinical follow-ups on small numbers of patients.9,20,30 Despite the fact that only eight patients were included in the current study, it is the largest study conducted to date on the prognosis of needle-track seeding. In the current study, needle-track seeding, when it was treated by en-bloc side excision, did not seem to affect the long-term clinical outcome. We believe that needle-track seeding from HCC does not modify clinical course, because tumor involvement in needle-tracks appears to be limited to subcutaneous tissues at puncture sites.31 Accordingly, we believe that aggressive local ablative treatment, such as, en-bloc wide excision, can effectively remove needle-track seeding. Furthermore, the prognosis of HCC is usually not dependent on the severity of metastatic lesions, but rather on hepatic functional reserve and on the characteristics of intrahepatic lesions.32
Based on the rationale that HCC infiltrates surrounding tissues and that several needle passes are conducted, we recommend that en-bloc wide excision of implanted nodules, including surrounding tissues, should be used to treat needle-track seeding from HCC rather than mass excision. However, Takahashi et al in a report of the recurrence of needle-track seeding after wide excision suggested that needle-tract seeding is not a local, limited disease.33 Nevertheless, their patient was treated by wide excision and radiotherapy and remained alive without evidence of recurrence, which reinforces the point that aggressive local treatment is well worth considering.
The current study has some limitations that should be mentioned. First, the number of patients enrolled and the follow-up period were not enough to determine the effects of the surgical method used to treat needle-track seeding on clinical outcome. Second, one of the two patients who experienced the recurrence of needle-track seeding after surgical excision had combined hepatocellular-cholangiocarcinoma and long-term clinical outcome of this patient could not be evaluated because of loss of follow-up. Combined hepatocellular-cholangiocarcinoma is known to have a poorer prognosis than the ordinary HCC.34 In the current study, the frequency of needle-track seeding in patients with combined hepatocellular-cholangiocarcinoma was 12.5%, which is much larger than that in patients with ordinary HCC. Nevertheless, we believe that en-bloc wide excision might be also useful for the treatment of needle-track seeding in this subgroup. Further studies in this subgroup will be needed to clarify this issue.
Recently, the long term survivals of HCC patients are increasing due, in no small part, to the introductions of curative local ablation and liver transplantation. The current study shows that needle-track seeding can be curatively treated by en-bloc excision without recurrence, and that therefore, it should not be considered to be similar to systemic metastasis. Therefore our findings indicate that needle-track seeding, if it is treated by en-bloc wide excision, should not be considered as contraindication for liver transplantation.
Taken together, needle-track seeding after PEI or FNAB by HCC is a rare but important complication, and it can also occur after PTBD for biliary obstruction by HCC. However, the result of follow-up indicates that the prognosis of needle-track seeding, when it is treated by en-bloc wide excision, is favorable. Our results suggest that implanted nodules should be treated by en-bloc wide excision in cases with needle-track seeding from HCC after an US-guided procedure, especially in patients awaiting liver transplantation.
Acknowledgements
This project was supported by grant No 04-2010-1110 from the SNUH Research Fund.
Abbreviations
CPT score
Child-Pugh-Turcotte score
CT
computed tomography
FNAB
fine-needle aspiration biopsy
HCC
hepatocellular carcinoma
PEI
percutaneous ethanol injection
PTBD
percutaneous transhepatic biliary drainage
US
ultrasound