INTRODUCTION
Amoebiasis is the second leading cause of death from parasitic disease worldwide.1 Amoebic liver abscess (ALA) is the most common extra-intestinal manifestation of Entamoeba histolytica infestation, and it is associated with significant morbidity and mortality.2 The common complications of ALA include rupture into pleural cavity and peritoneal cavity; rarely, vascular complications are seen in ALA in the form of thrombosis or compression resulting in either hepatic venous outflow obstruction or inferior vena cava (IVC) obstruction. There have been only a few case reports of ALA with IVC obstruction.3-7 We present three cases of ALA where the patients presented with signs of IVC obstruction and radiological confirmation of the IVC obstruction by thrombosis and/or external compression.
CASE REPORT
Case 1
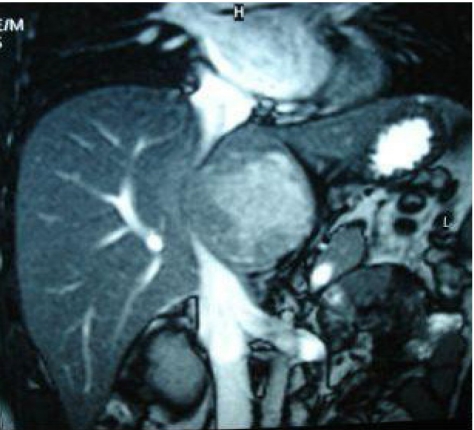
A 24-year old man presented with pain in right upper abdomen with fever for five days. Physical examination revealed high grade fever and tachycardia. There was tenderness and guarding in right hypochondrium. There was bilateral pedal edema. Hematological investigations revealed a hemoglobin (Hb) level of 11.2 g/dL and white blood cell (WBC) count of 18,400/mm3 (normal range, 4,000-11,000/mm3). The biochemical investigations showed a blood urea nitrogen (BUN) of 34 mg/dL (normal range, 15-40 mg/dL), serum creatinine of 1.1 mg/dL (normal range, <1 mg/dL). Liver functions tests showed a total bilirubin of 1.5 mg/dL (normal range, <1 mg/dL), serum alkaline phosphatase (ALP) of 178 IU/L (normal range, 40-280 IU/L), aspartate aminotransferase (AST) 32 IU/L (normal range, <40 IU/L), alanine aminotransferase (ALT) 48 IU/L (normal range, <40 IU/L). Chest X-ray was normal. Ultrasound at admission showed a large (8.6├Ś7.3├Ś6.2 cm), volume 202 mL, heterogeneously hypoechoic lesion with internal echoes in the caudate lobe suggestive of liver abscess. On ultrasonography, the abscess was compressing the intra-hepatic IVC with abnormal color fill (slowed down) and flow pattern. Magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP) was performed which confirmed 6.9├Ś6 cm abscess in the caudate lobe causing eccentric compression over the intrahepatic part of IVC (Fig. 1, Fig. 2). There was a mass effect with compression of the main portal vein and the common hepatic duct just after the ductal confluence, however, the right and left hepatic ducts and intra-hepatic biliary radicals were not dilated. The patient tested positive for amoebic antibody by enzyme-linked immunosorbent assay (ELISA) test. The patient was started on broad spectrum antibiotics and metronidazole for two weeks. After initiating the treatment, there was a gradual amelioration in the fever and abdominal pain. Repeat ultrasound by the end of first week revealed a gradual reduction in the size of the abscess to 50% of its original size and the compression on IVC was also relieved as confirmed by doppler scan. The patient was asymptomatic. Follow-up investigations showed WBC of 8,800/mm3, and liver functions tests showed a total bilirubin of 0.5 mg/dL, serum ALP of 145 IU/L, AST 40 IU/L, ALT 45 IU/L. Patient was followed up for three months and repeat ultrasound done at the end of three months showed no residual abscess and IVC was normal in caliber, color fill and flow pattern.
Case 2
A 21-year old male presented with upper abdominal pain for 15 days accompanied by a gradually increasing abdominal girth and swelling of the feet with low grade fever for one week. On examination, he was normo-tensive and showed pitting pedal edema. There was a tender hepatomegaly extending three fingers below the costal margin in the mid-clavicular line. Shifting dullness was positive. Hematological investigations revealed Hb level of 9 g/dL and WBC of 7,500/mm3. The biochemical investigations showed a raised BUN of 65 mg/dL and serum creatinine of 1.5 mg/dL. Urine analysis revealed slight proteinuria. Liver functions tests showed a total bilirubin of 0.6 mg/dL, serum ALP of 247 IU/L, AST 40 IU/L and ALT 80 IU/L. Ultrasonography of the abdomen showed an abscess in the right lobe of liver on its postero-superior surface measuring 1.4├Ś1├Ś1 cm with internal echoes and moderate ascites. Color doppler scan was done which showed patent hepatic veins with normal hepatofugal flow. Hepatic IVC was seen displaced and compressed by the large abscess cavity but the flow was normal. Infra-hepatic IVC was dilated to 1.7 cm. The Doppler findings were suggestive of IVC obstruction due to the liver abscess with proximal dilatation. A contrast enhanced CT scan confirmed the findings of thrombus in the IVC (Fig. 3). The patient tested positive for amoebic antibody by indirect haemagglutination test. The patient was started on intravenous metronidazole and broad spectrum antibiotics. The liver abscess was aspirated twice under ultrasonic guidance within a period of two days yielding 500 mL and 360 mL of pus. The pus was thick, creamy and brownish in color and did not grow any organisms on culture. The ascites and pedal edema disappeared rapidly after the treatment. Doppler scan repeated four days later showed a decrease in the infra-hepatic IVC dilatation. Hepatic portion of the IVC was normal in caliber and fully patent in subsequent color doppler examination performed twelve days after the aspiration of pus. The biochemical renal parameters improved and two weeks after aspiration of the liver abscess, the BUN was 32 mg/dL and serum creatinine was 1.1 mg/dL. Patient was followed up for three months, and repeat ultrasonography done was essentially normal.
Case 3
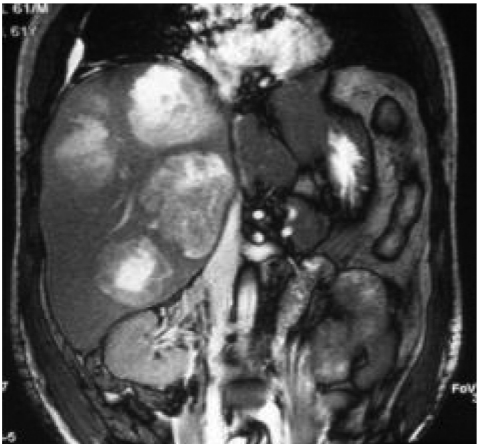
A 61-year old man presented with high grade fever for eight days, vomiting for five days associated with right upper abdomen pain, yellowish discoloration of eyes for three days, and swelling of the feet for three days. He was icteric with a pulse rate of 96/min and blood pressure of 126/80 mmHg. There was bilateral pedal edema. On abdominal examination, tender hepatomegaly was present three finger breadth below the costal margin. Ultrasonography revealed multiple abscesses in the liver, the largest one 8├Ś7.2├Ś6.8 cm in the right lobe with mild pleural effusion. Hematological investigations revealed a Hb of 9.4 gm/dL and WBC 29,900/mm3 with predominantly polymorphic leukocytosis. The biochemical investigations showed a raised BUN of 59 mg/dL, serum creatinine of 1.2 mg/dL. Liver function tests showed total bilirubin of 4.9 mg/dL, direct bilirubin of 3.8 mg/dL, ALP of 1,055 IU/ L, AST of 99 IU/L and ALT of 108 IU/L. The patient tested positive for amoebic antibody by ELISA test. MRI with MRCP revealed four abscesses, two in the right lobe, one in the left lobe and one in the caudate lobe (Fig. 4). The largest one was 7.5├Ś7.2├Ś7 cm in size, in the right lobe. The abscess in the caudate lobe was compressing the porta hepatis and IVC (Fig. 5). The flow in IVC was found to be slowed down on color doppler. Catheter drainage was done from the largest abscess and the patient was started on intravenous metronidazole and broad spectrum antibiotics. Total 580 mL of pus was drained before the catheter was removed. After five days of admission the pedal edema reduced markedly and after ten days it subsided completely. Liver function tests returned to normal range with total bilirubin 1.1 mg/dL, direct bilirubin 0.3 mg/dL, ALP 22 IU/L, AST 42 IU/L and ALT 20 IU/L. The patient was discharged in good condition and followed up for three months and repeat ultrasound done at the end of three months showed no residual abscess and IVC was normal in caliber, color fill and flow pattern.
DISCUSSION
Amoebiasis occurs in 10% of the world's population and is most common in tropical and subtropical regions.1 Humans are the principal hosts and reservoir and get infected by ingestion of contaminated food and water containing amoebic cysts.2 ALA develops in less than 1% of patients infested with E. histolytica, but this still represents a large number of patients.2 The disease should be suspected in anyone with an appropriate exposure history (residency or travel in an endemic area) and fever, right upper quadrant pain, and substantial hepatic tenderness.
The diagnosis of ALA relies on identification of space occupying lesion of the liver and positive amoebic serology.1 Amoebic serology is highly sensitive (>94%) and highly specific (>95%) for the diagnosis of amoebic liver abscess.8 Antibodies develop in 90 to 100% of patients with ALA and become detectable at seven to ten days after the onset of symptoms. Indirect hemagglutination and enzyme-linked immunosorbent assay are widely used because of their high sensitivity.2 Computed tomography is an ideal tool to detect liver abscesses, particularly smaller lesions and its associated complications. Its sensitivity for detecting liver abscess is as high as 97%.9
The rate of various complications described in an ALA was reported to be 10.3%.10 Complications associated with liver abscess include rupture into pleural, pericardial & peritoneal cavity, vascular thrombosis, and rupture into the bile ducts.11 Early diagnosis and prompt treatment are essential to reduce the morbidity and mortality associated with a liver abscess. The mortality rate being low when the abscess is limited to liver but it increases as the abscess gets complicated. Therefore, the early detection of complications associated with hepatic abscess is important. Vascular complications of hepatic abscess, such as thrombosis of the portal vein, occlusion of hepatic vein, or inferior vena cava obstruction, are rare and they have been previously described mostly in autopsy studies.12 This was a large study by Krishnan et al12 where retrospective analysis of 95 autopsies on ALA was done and IVC thrombosis was seen in 8% of the cases in combination with hepatic vein in all but one. One of the cases showed rupture of the abscess into IVC. Apart from this study, there have been very few case reports in which IVC obstruction has been described in patients with ALA.3-7 Huddle3 reported a case of 26 year old man with ALA where it was complicated with extrinsic compression of the IVC by an abscess in the caudate lobe of the liver at the level where it passes through the liver. There was no evidence of IVC thrombosis. Hodkinson et al4 reported another case of 50 year old man with ALA where the patient developed IVC obstruction due to a thrombus which extended up to the right atrium. Another case was reported by Sharma and Sarin5 where a 30 year old man presented with ALA with signs of hepatic venous outflow obstruction, later found to be due to compression of the IVC by a large and tense abscess in the caudate lobe of the liver. Sodhi et al6 reported a case where amoebic liver abscess in a 57 year old man was complicated by hepatic vein and IVC thrombosis. Schmid et al7 reported another case of a 19 year old man with ALA where the patient had signs if IVC obstruction due to external compression of the IVC and not due to thrombosis. In another study by Yang et al,11 a retrospective analysis of 81 patients with pyogenic liver abscess, three patients had vascular complications. Of these three patients, two had portal vein thrombosis only and one had extrinsic compression of the IVC associated with portal vein thrombosis. There were only three cases of our report described where the ALA has led to extrinsic compression of the IVC in absence of any thrombosis so far. This complication can be managed effectively by catheter drainage or percutaneous needle aspiration combined with antibiotics. In all the three cases of ALA with IVC compression mentioned above, percutaneous needle aspiration of the abscess was required to relieve the compression and all the patients were discharged in good condition. In our cases, two patients required percutaneous drainage and in one patient, IVC compression was relieved with antibiotics alone. The management of ALA with IVC thrombosis again mainly includes antibiotics and drainage of the abscess, but in few cases, anticoagulation therapy has also been added to achieve complete resolution.
We report three cases of ALA causing IVC obstruction which completely resolved by the percutaneous drainage and appropriate antibiotic therapy.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




