INTRODUCTION
Hepatic amyloidosis is a rare disease that presents as an infiltrative disease involving liver. Amyloidosis is a systemic disease characterized by the extracellular deposition of amyloid protein in many organs.1-4 Progressive organ involvement leads to organ malfunction and death usually resulting from renal and/or cardiac involvement. Liver and spleen are major sites of involvement.1-3 The wide range of presenting symptoms encountered makes rapid clinical diagnosis difficult. None of the present imaging techniques is capable of specifically demonstrating the presence of amyloid. Even when suspected clinically and radiologically, the diagnosis of amyloidosis depends on a tissue biopsy to confirm the presence of amyloid deposits.5
To provide more detailed understanding of hepatic amyloidosis, here a case of amyloidosis involving liver is presented with radiological imaging findings including computed tomography (CT).
CASE
A 45-year-old female was admitted with the complaint of generalized edema. She got about 6 kg of weight gain during recent one week. She had dizziness, dyspnea, anorexia, nausea and epigastric discomfort. She presented physical examination findings including neck vein engorgement, abdominal distension, hepatomegaly and pitting edema. She had history of syncope about one month ago, but brain magnetic resonance imaging (MRI) showed no abnormal finding. The laboratory findings showed leukocyte count of 11,500/mm3, hemoglobin level of 9.1 g/dL and platelet count of 284,000/mm3. Biochemical tests showed that the serum level of alanine aminotransferase was 30 IU/L, aspartate aminotransferase was 55 IU/L, and alkaline phosphatase elevated up to 398 IU/L. Serum albumin was 3.7 g/dL, total bilirubin was 1.2 mg/dL, and creatinine was 2.3 mg/dL. Alpha fetoprotein was less than 1 ng/mL. The results for hepatitis B surface antigen and anti-HBs were negative. Urine analysis showed albumin positive, and otherwise negative.
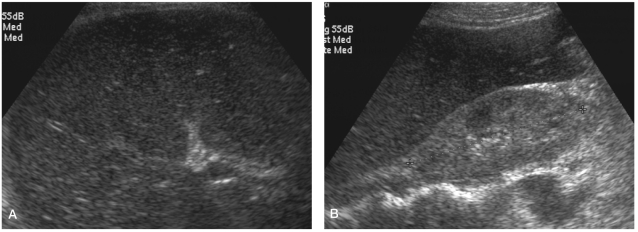
Renal disease was suspected and abdominal ultrasonography was done. Liver showed diffuse coarse echo and hypoechoic pattern with hepatomegaly (Fig. 1A). Both kidneys showed also diffuse increased cortical echo suggesting renal parenchymal disease (Fig. 1B).
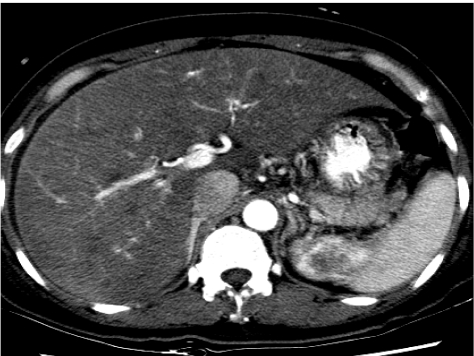
Dynamic contrast enhanced CT was taken because of abnormal liver echo and size. On arterial phase, there was no enhancing lesion in liver (Fig. 2). On portal phase, size of liver increased, and especially left lobe showed bulging contoured enlargement and ill-defined hypoattenuation (Fig. 3A, 3B). There were multiple ill-defined hypoattenuatted areas in right lobe. Spleen showed normal enhancement, but size increased. Both kidneys also showed multiple irregular decreased attenuation lesions (Fig. 3C). Because liver showed decreased echo on ultrasonography, it was assumed that it was not fatty infiltration. These CT findings suggested diffuse infiltrative disease, so liver biopsy was done. Percutaneous fine-needle-aspiration biopsy was performed under ultrasound guidance, and a histological examination of the biopsy specimen showed amorphous material stained by Congo red stain. The deposit demonstrated characteristic positive birefringence with polarized light. Biopsy results led to a final diagnosis of extensive amyloidosis.
Additional examinations were done to evaluate the extent of amyloidosis involvement. 2D Doppler echocardiography showed enlarged both atrium and thickened left ventricle wall with normal vetnrcular contractility, which suggested infiltrative disease such as amyloidosis. Bone marrow aspiration and colonic mucosa biopsy showed also amyloidosis. Urine Immunoelectrophoresis showed abnormal zone of restriction in kappa light chain, suggesting Bence-Jones protein, free kappa type.
She was diagnosed as systemic amyloidosis, and chemotherapy was done. However, hepatic failure with hepatic encephalopathy was aggravated and she got discharged in a moribund state.
DISCUSSION
Amyloid is defined as a substance which: (1) stains positively with Congo red, (2) exhibits apple green birefringence by polarization microscopy, (3) shows aggregations of approximately 10 nm wide fibrils on electron microscopy, (4) exhibits a ╬▓-pleated sheet configuration, and (5) shows resistance to proteases other than pronase.5 Progressive deposition of amyloid compresses and replaces normal tissue, and this leads to organ dysfunction and a wide variety of clinical syndromes, some of which have severe pathophysiological consequences.
Amyloidosis is usually seen in a systemic form, but 10-20% of cases can be localized.4 Men are affected more than women, and the mean age of presentation is 55-60 years. Some causes of secondary amyloidosis are multiple myeloma (10-15%), rheumatoid arthritis (20-25%), tuberculosis (50%), or familial Mediterranean fever (26-40%).4 Approximately one-third of patients with primary amyloidosis develop congestive heart failure. It is the leading cause of death in patients with primary and myeloma-related amyloidosis.
In case of hepatic amyloidosis, amyloid is deposited in the parenchyma, along the sinusoids within the space of Disse, or in blood vessel walls. Hepatocytes are severely compressed by extensive accumulation of amyloid and they may atrophy or nearly disappear. In advanced cases with massive infiltration, the liver is enlarged with rubbery elastic consistency, and it may show 'lardaceous liver' appearance on cut surface.1
Although hepatic involvement is very common in patients with amyloidosis, the clinical manifestations of hepatic involvement are usually mild. Symptomatic involvement, including rupture, portal hypertension or hepatic failure, is rare. Hepatomegaly and a borderline abnormal liver function test are the most frequent findings in patients with hepatic amyloidosis.3,5 However, serious symptoms such as hepatic failure and portal hypertension may develop. Spontaneous rupture and massive hemorrhage may occur; therefore, needle biopsy should be performed carefully. In one report 77% of the patient had an associated nephrotic syndrome, congestive heart failure, peripheral neuropathy, or orthostatic hypotension. Other signs of hepatic amyloidosis included proteinuria (88%), elevated serum alkaline phospatase (86%), abnormal serum protein electrophoresis (monoclonal protein or hypogammaglobulinemia, 64%), hyposplenism on the peripheral blood smear (62%), defined by the presence of Howell-Jolly bodies; and hepatomegaly (81%) disproportional to the liver enzyme abnormalities. Liver function tests were not sensitive or specific. Normal levels of aspartate aminotransferase, and bilirubin were seen in 32%. The median survival of the entire group was nine months.2,3
Radiological findings of hepatic involvement are nonspecific, Amorphous or irregular calcifications were occasionally identified within the amyloid deposit. Definitive diagnosis requires biopsy confirmation, as CT findings are nonspecific.5,6 The ultrasonographic findings of primary hepatic amyloidosis have not been well described. In one reported case, heterogeneous echogenicity was seen in the liver as in the present case.
The frequent findings of conventional precontrast and contrast-enhanced CT are an enlarged liver with heterogeneous decreased attenuation.1,6 Calcification may be seen rarely in the hepatic parenchyma. The hepatic parenchyma infiltrated more highly by amyloid may appear as focal hypoattenuating areas on contrast-enhanced CT scans. This finding probably resulted from impairment of blood flow due to vascular involvement and diffuse parenchymal infiltration of amyloid.1 Delayed phase CT scans showed delayed enhancement with the presence of some focal hypoattenuating areas in the liver. The delayed enhancement was probably due to delayed passage of contrast medium in the involved parenchyma, and the hepatic parenchyma with prominent infiltration might appear as the focal hypoattenuating areas. Kim et al5 suggested that hepatic amyloidosis have characteristic features of hepatic contour; and asymmetric and triangular hepatomegaly with the apex at the falciform ligament. This finding was believed to be the result of mild atrophic change of the lateral border of both hepatic lobes, in spite of hepatic enlargement reported in other infiltrative diseases.
MR imaging has been used for the evaluation of primary hepatic amyloidosis. One report showed that, although T2 value of the hepatic parenchyma was not changed, T1 value was increased and it could beused to monitoring of chemotherapy.1 However, the reason for high signal intensity on T1 is not known.
One report showed that the deposition of amyloid in the spleen was identified in about 83% of patients at the time of autopsy.1 Amyloid tends to infiltrate in the red pulp or blood vessel walls. The spleen may swell and harden by massive infiltration, and 'bacon spleen' appearance may be seen on cut surface in advanced cases. Splenic involvement is usually asymptomatic. Hyposplenism may occur and potentially increase the risk of serious infection. Spontaneous splenic rupture is a known consequence of splenic amyloidosis. CT findings of primary splenic amyloidosis include splenomegaly, calcification and poor contrast enhancement of the splenic parenchyma on conventional contrast-enhanced CT scans. Mild delayed enhancement was noted in the spleen on delayed phase CT scans.1,4 In the spleen, arterial phase CT showed the lack of parenchymal enhancement, and T2-weighted MR imaging showed decreased signal intensity.2
SUMMARY
Amyloidosis can demonstrate a wide spectrum of disease in nearly every organ and tissue type. Hepatic involvement shows 1) hepatomegaly, 2) inhomogeneous areas of decreased attenuation on CT, with focal or diffuse involvement, 3) delayed enhancement with intravenously administered contrast material, or rarely 4) hepatic rupture or marked hepatic calcification.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




