Optimal time for repeating the IgM anti-hepatitis A virus antibody test in acute hepatitis A patients with a negative initial test
Article information
Abstract
Background/Aims
The nonspecific clinical presentation of acute hepatitis A (AHA) mandates the detection of anti-hepatitis A virus IgM antibodies (IgM anti-HAV) in the serum for obtaining a definitive diagnosis. However, IgM anti-HAV might not be present during the early phase of the disease. The aim of this study was to determine the optimal time for repeating the IgM anti-HAV test (HAV test) in AHA patients with a negative initial test.
Methods
In total, 261 patients hospitalized with AHA were enrolled for this retrospective study. AHA was diagnosed when the test for IgM anti-HAV was positive and the serum alanine aminotransferase (ALT) level was ≥400 IU/L. Repeat HAV test was conducted after 1-2 weeks if the initial HAV test was negative but AHA was still clinically suspected.
Results
The results of the initial HAV test were negative in 28 (10.7%) patients. The intervals from symptom onset to the initial-HAV-test day and from the peak-ALT day to the initial-HAV-test day were significantly shorter in the negative-initial-HAV-test group, but on multivariate analysis only the latter was significantly associated with negative results for the initial HAV test (β=-0.978; odds ratio [95% confidence interval]=0.376 [0.189-0.747]; P=0.005). The HAV test was positive in all patients when it was performed at least 2 days after the peak-ALT day.
Conclusions
The results of HAV tests were significantly associated with the interval from the peak-ALT day to the HAV-test day. The optimal time for repeating the HAV test in clinically suspicious AHA patients with a negative initial HAV test appears to be at least 2 days after the peak-ALT day.
INTRODUCTION
Acute hepatitis A (AHA) is the most common cause of acute hepatitis in Korea.1,2 It usually results in a self-limited episode of acute hepatitis without chronic infection or complication.3 The overall prognosis of AHA is excellent; about 60% of patients completely recover within 2 months and almost every affected person recovers within 6 months.3
Diagnosis of AHA is usually made by the detection of anti-hepatitis A virus IgM antibodies (IgM anti-HAV) in serum. IgM anti-HAV test (HAV test) have high diagnostic sensitivity and specificity of more than 99%.4 The test result usually becomes positive at the onset of symptoms5 and usually remains positive for approximately 4 months thereafter.6 However, IgM anti-HAV is not detected in some patients with AHA, especially during the early phase of AHA. Previous studies suggested that initial HAV test was negative in 6.4-6.7% of patients with AHA.7,8 Hence, repeating HAV test after 1-2 weeks is usually recommended in clinically suspicious AHA patients with negative initial HAV test. Nevertheless, data to substantiate this recommendation is scarce and studies validating this suggestion are lacking. Therefore, we performed this retrospective study to evaluate the optimal time for repeating HAV test in clinically suspicious AHA patients with negative initial HAV test.
PATIENTS AND METHODS
Patients
We retrospectively reviewed the medical records of all patients with AHA who had been admitted to the Korea University Anam Hospital between January 2001 and December 2009. Patients were hospitalized if they suffered from severe generalized weakness and/or poor oral intake. AHA was diagnosed when the patients were found to be positive for IgM anti-HAV and had a serum alanine aminotransferase (ALT) level of ≥400 IU/L. HAV test was repeated 1-2 weeks after the initial HAV test when the initial test result was negative but AHA was still clinically suspected and no other cause of acute hepatitis could be documented.
Definitions
Day 0, defined as the day of acute hepatitis-associated symptom onset, was determined by thoroughly reviewing the patients' history through medical records. Serum ALT and bilirubin (BIL) levels were repeated in each patient every 2-3 days until peak levels of all parameters were identified in all enrolled patients.
The course of AHA was classified into 3 periods as follows (Fig. 1):9
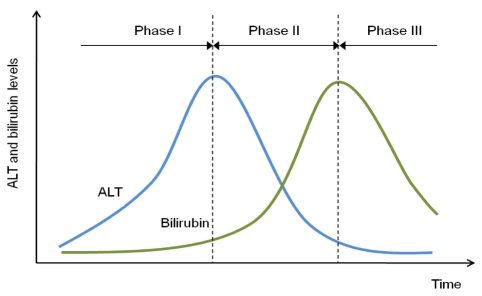
Definition of the phase of AHA. Phase I is the period from the AHA-associated symptom-onset day to the peak-ALT day. Phase II is the period from the peak-ALT day to the peak-bilirubin day. Phase III is the period after the peak-bilirubin day. ALT, alanine aminotransferase.
Phase I was defined as the period from day 0 to the day when serum ALT levels peak (peak-ALT day). The serum levels of both ALT and BIL usually increase during this period.
Phase II was defined as the period from the peak-ALT day to the day when serum BIL levels peak (peak-BIL day). The serum ALT levels decrease but serum BIL levels continue to increase during this period.
Phase III was defined as the period after the peak-BIL day. The serum levels of both ALT and BIL decreased during this period, but have not recovered to below the upper limit of normal.
In patients who were admitted during the phase II, the admission day was assumed as the peak-ALT day, and in those who were admitted during the phase III, the admission day was assumed as both peak-ALT day and the peak-BIL day.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 13.0; SPSS Inc., Chicago, IL, USA). Data are represented as mean±standard deviation (SD), or percentage values. Mann-Whitney U-test and the chi-square test were used to compare continuous and categorical variables, respectively.
To identify the significantly associated factors with the result of the initial HAV test, univariate analysis for age, sex, HBs (hepatitis B surface) antigen, duration of hospitalization, durations to the first HAV-test day from the day 0 to the first HAV-test day, peak-ALT and BIL days, the course of AHA at the first HAV-test day, ALT and BIL levels on the first HAV-test day, and peak-ALT and BIL levels were performed. Then, multivariate logistic regression analysis was performed using variables with P<0.1. P<0.05 was considered statistically significant.
RESULTS
Baseline characteristics
A total of 261 patients with AHA were hospitalized during the study period. The mean age was 31.2±7.0 years and 158 patients (60.5%) were men (Table 1). Patients were hospitalized 5.3±2.6 days after day 0. Baseline serum ALT and BIL levels were 2962.4±1961.3 IU/L and 4.5±3.2 mg/dL, respectively. When the patients were classified at baseline according to the course of AHA, 61 (23.4%) patients belonged to phase I, 126 (48.3%) to the phase II, and 74 (28.4%) to phase III. Peak serum ALT and BIL levels were 3442.2±2033.8 IU/L and 7.3±4.3 mg/dL, respectively.
The initial HAV test during hospitalization was performed 6.3±2.9 days after day 0. The test was done during phase I in 41 (15.7%) patients, phase II in 125 (47.9%) patients, and phase III in 95 (36.4%) patients (Fig. 2). Serum ALT and BIL levels at the time of first HAV test were 2985.4±1944.5 IU/L and 4.5±3.2 mg/dL, respectively. The result of initial HAV test was positive in 233 (89.3%) patients, thus being diagnosed as AHA, while it was negative in 28 (10.7%) patients.
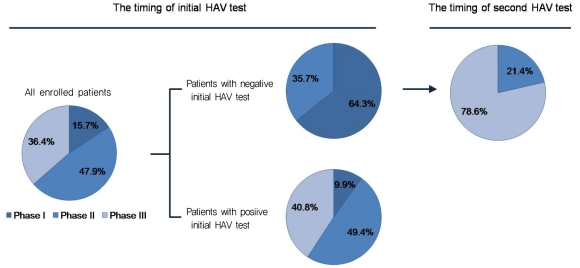
Timing of the initial HAV test. At the time of the initial HAV test, about half of the patients were in phase II, and none of the patients with negative initial HAV test were in phase III. The HAV test was repeated 6.5±2.3 days (mean±SD) after the first test in these 28 patients, at which time 6 (21.4%) patients were in phase II and 22 (78.6%) were in phase III. HAV, hepatitis A virus.
In these 28 patients, the second HAV test was done 6.5±2.3 days after the first HAV test. The interval from the peak-ALT day to the second test was 5.0±3.2 days (range, 1-16 days), while the interval from the peak-BIL day to the second test was 1.1±3.9 days (range, -9~13 days). The second HAV test was done during phase II in 6 (21.4%) patients and during phase III in 22 (78.6%) patients (Fig. 2).
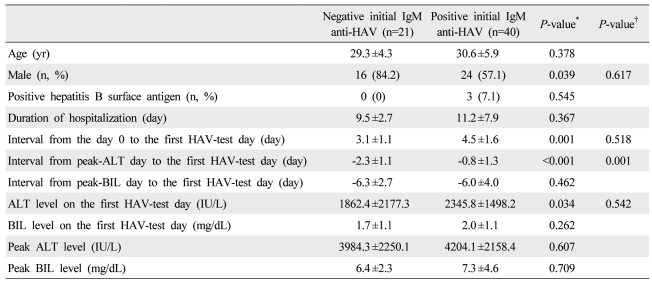
Comparison between patients with negative initial IgM anti-HAV and with positive initial IgM anti-HAV
The proportion of men was greater in the negative initial IgM anti-HAV group than the positive initial IgM anti-HAV group, while the age did not differ between the two groups (Table 2). Interval from day 0 to the first HAV-test day (3.9±2.2 days vs. 6.6±2.9 days, P<0.001) and that from peak-ALT day to the first HAV-test day (-1.5±1.5 days vs. 0.7±1.6 days, P<0.001) were significantly shorter in the negative initial HAV test group. In all patients with negative initial HAV test, the test was done during phase I or II. On the contrary, in patients with positive initial HAV-test, the test was usually done during phase II or III (P<0.001).
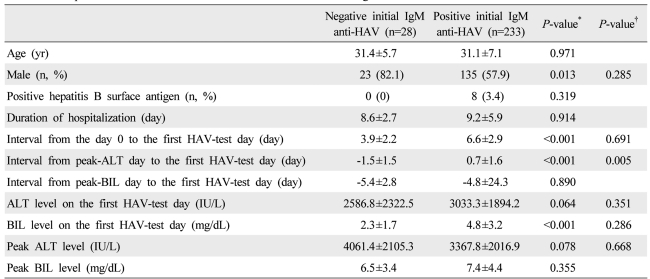
Comparison of clinical and biochemical characteristics according to the results of the first HAV test
Serum ALT levels at the time of the initial HAV test showed a tendency to be lower in patients with negative initial HAV test (2586.8±2322.5 IU/L vs. 3033.3±1894.2 IU/L, P=0.064), while peak-ALT levels showed a tendency to be higher in these patients (4016.4±2105.3 IU/L vs. 3367.8±2016.9 IU/L, P=0.078). Serum BIL level at the time of the initial HAV tests was significantly lower in the negative initial HAV test group than the positive initial HAV test group (2.3±1.7 mg/dL vs. 4.8±3.2 mg/dL, P<0.001), while peak-BIL level did not differ between the 2 groups (6.5±3.4 mg/dL vs. 7.4±4.4 mg/dL, P=0.355). On multivariate logistic regression analysis, only the duration from the peak-ALT day to the initial HAV-test day were significantly associated with negative results for the initial HAV test (β, -0.978; odds ratio [95% confidence interval], 0.376 [0.189-0.747]; P=0.005). The proportion of patients with negative initial HAV test decreased when the initial HAV test time approached the peak-ALT day (likelihood ratio, 53.8; P<0.001 on linear-by-linear association) (Fig. 3). HAV test was positive in all patients when it was performed at least 2 days after the peak-ALT day.
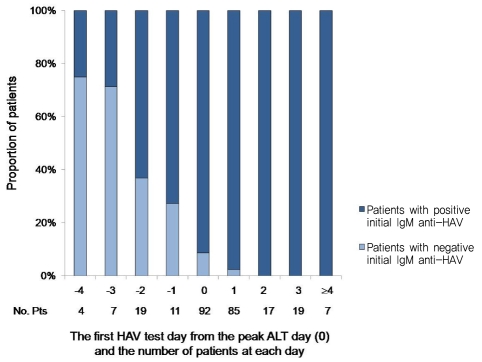
Proportions of patients with negative initial HAV tests at each day from the peak-ALT day (defined as day 0). The proportion of patients with a negative initial HAV test decreased as the initial HAV test time approached the peak-ALT day, and the test for IgM anti-HAV was positive in all patients at 2 days after the peak-ALT day.
Subgroup analysis in patients hospitalized during the phase I of acute hepatitis A
The positivity of HAV tests were significantly related with the interval from the peak-ALT day to the HAV-test day. However, the peak-ALT day could not be said to have represented their true peak day or their true peak levels in patients admitted during the phase II or III. Therefore, we performed a subgroup analysis with patients who were hospitalized during the phase I.
Consistent with the results of analysis with all enrolled patients, proportions of men and patients who had their initial HAV tests during the phase I were more frequent in the negative initial HAV test group than in the positive initial HAV test group. In addition, intervals from day 0 to the initial HAV-test day (3.1±1.1 days vs. 4.5±1.6 days, P=0.001) and from peak-ALT day to the initial HAV-test day (-2.3±1.1 days vs. -0.8±1.3 days, P<0.001) were significantly shorter in patients with negative initial HAV test than those with positive initial HAV test. Serum ALT levels at the time of the initial HAV test were significantly lower in patients with negative initial HAV test (1862.4±2177.3 IU/L vs. 2345.8±1498.2 IU/L, P=0.034). However, peak ALT (3984.3±2250.1 IU/L vs. 4204.1±2158.4 IU/L, P=0.607) and BIL levels (6.4±2.3 mg/dL vs. 7.3±4.6 mg/dL, P=0.709) did not differ between 2 groups. On multivariate logistic regression analysis, only the interval from the peak-ALT day to the initial HAV-test day was significantly associated with the negative results for the initial HAV tests (β, -0.984; odds ratio [95% confidence interval], 0.374 [0.209-0.669]; P=0.001) (Table 3).
DISCUSSION
Our results suggest that up to 10% of patients with symptomatic AHA cannot be diagnosed if we rely solely on the result of initial HAV test. HAV RNA assay could be an option for diagnosing AHA in patients whose HAV test is negative. HAV RNA has been detected in the serum, stool, and liver tissue using molecular hybridization assay or reverse transcription-PCR assay.10,11 However, the use of HAV RNA assay is still limited to research laboratories.3 Therefore, repeating HAV test after a certain period of time in clinically suspicious but negative initial HAV test patients seems to be more practical to make the diagnosis of AHA for the time being. Although repeating HAV test after 1 to 2 weeks is generally recommended for those with initially negative result, not much is known about the appropriate time interval fit for reevaluation and studies are lacking to support this recommendation. The results of our study show that in most of the patients with negative initial HAV test, the test was performed before the peak-ALT day. However, when the initial or follow-up HAV test was performed at least 2 days after the peak ALT level, it was positive in all patients. In addition, on multivariate analysis, the only significant parameter associated with the result of the initial HAV test was the duration from peak-ALT day to the initial test day. Therefore, it could be suggested that the optimal time for repeating HAV test in clinically suspicious AHA patients with negative initial HAV test would be at least 2 days after peak-ALT day.
Although previous studies have not classified and analyzed their data according to the clinical course of AHA as we have done in our study, the fact that higher proportion of patients presented with fever and abdominal pain7 or lower ALT level and that the interval from symptom onset to hospital admission was shorter12 in patients with negative initial HAV test suggest that, consistent with our data, initial tests had been performed during the phase I in the majority of study subjects.
When we look at Table 2, patients with negative initial IgM anti-HAV show lower ALT and BIL level than those with positive initial anti-HAV at the time of first HAV test, but the peak ALT and BIL level are higher in the former patients. Therefore, we are apt to think that these patients would go through a more aggressive clinical course. However, since most of the patients with positive initial HAV test have been admitted during the phase II or III, their true peak ALT or BIL level cannot be said to have been rightly assessed. To clarify whether there is any relationship between the result of initial HAV test and the clinical course, we performed a subgroup analysis only with those admitted during the phase I whose true peak ALT and BIL level could be obtained. The result of this subgroup analysis showed that the peak ALT and BIL level did not differ between the negative initial HAV test group and the positive initial HAV test group.
A previous study suggested that the negative results in the initial HAV tests are associated with the short interval from symptom onset to hospital admission, high body mass index, and low initial ALT level on the multivariate analysis.12 Consistently, both the duration from day 0 to the initial HAV-test day and the duration from peak-ALT day to the initial HAV-test day were associated with the results of the initial HAV-test day on univariate analysis in our study. However, only the duration from peak-ALT day to the initial HAV-test day was associated with the results of the initial tests on multivariate analysis. These results suggest that the appearance of IgM anti-HAV is associated with the course of immune response to HAV. In addition, since perception of AHA symptoms is very subjective, the day when patients first feel the symptoms may vary greatly from person to person during the course of the disease process. Furthermore, the fact that the data on first symptom presentation can only be obtained through history taking, which in turn depends entirely on the recollection by the patients, renders the information on first symptom presentation date not so reliable. This could explain why the result on initial HAV test shows closer and better association with the duration from peak-ALT day to the initial HAV-test day, which is objective, than the duration from symptom onset to the initial HAV-test day.
Shin et al8 suggested high initial cutoff index of HAV test (≥0.5), low serum BIL level (<1.4 mg/dL), and low platelet count (<165×103/µL) as predictive factors for positive result on HAV retesting. However, when we applied these suggested predictive factors to our patients, seven patients among 28 patients (25%) with negative initial HAV test did not meet any one of them.
The result of our study shows that initial HAV tests were negative in 10.7% of patients with AHA, which is relatively higher than that of the previous studies (6.4-6.7%).7,12 Because these previous studies have not separately demonstrated the data of their patients according to the phase of AHA, it is difficult to clearly state the reason for this discrepancy on initial HAV test negativity. However, there is a possibility that higher proportion of patients could have been hospitalized during the phase I in our study. Because symptoms during the prodromal period, including fever, chill, nausea, and abdominal pain, are too nonspecific, it is not easy for the patient to consider themselves to have AHA during this period. Therefore, most of the patients with AHA make hospital visits during the icteric period because of jaundice. In Korea, the prevalence of symptomatic AHA has increased since the AHA outbreak in 200813 and ever since, more people have become more aware of AHA and visit the hospital to be assessed for this condition if they have fever of chilling sensation. Consistent with this trend, the proportion of patients who visited the hospital during the prodromal period has risen and this might have led to these discrepancies in our study compared to the previous studies.
In conclusion, the result of HAV test was significantly associated with the duration from peak-ALT day to the test day. The optimal time for repeating HAV test in clinically suspicious patients with negative initial test seems to be at least 2 days after peak-ALT day.
Acknowledgements
This study was supported by a grant from Ministry for Health and Welfare, Republic of Korea (A050021).
Notes
The authors declare no conflicts of interest.
Abbreviations
AHA
acute hepatitis A
ALT
alanine aminotransferase
BIL
bilirubin
HAV test
IgM anti-HAV test
IgM anti-HAV
anti-hepatitis A virus IgM antibodies
peak-ALT day
the day when serum ALT levels peak
peak-BIL day
the day when serum BIL levels peak