Non-alcoholic fatty liver diseases: update on the challenge of diagnosis and treatment
Article information
Abstract
The prevalence of non-alcoholic fatty liver disease (NAFLD) is estimated to be 25-30% of the population, and is the most common cause of elevated liver enzymes in Korea. NAFLD is a “hot potato” for pharmaceutical companies. Many clinical trials are underway to develop a first-in-class drug to treat NAFLD. However, there are several challenging issues regarding the diagnosis of NAFLD. Currently, liver biopsy is the gold standard method for the diagnosis of NAFLD and steatohepatitis. Ideally, globally recognized standards for histological diagnosis and methods to optimize observer agreement on biopsy interpretation should be developed. Liver biopsy is the best method rather than a perfect one. Recently, multi-parametric magnetic resonance imagery can estimate the amount of intrahepatic fat successfully and is widely used in clinical trials. But no diagnostic method can discriminate between steatohepatitis and simple steatosis. The other unresolved issue in regard to NAFLD is the absence of satisfactory treatment options. Vitamin E and obeticholic acid have shown protective effects in randomized controlled trials, but this drug has not been approved for use in Korea. This study will provide a description of diagnostic methods and treatments that are currently recommended for NAFLD.
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is a disease complex that includes simple steatosis (fatty accumulation in the liver), non-alcoholic steatohepatitis (NASH) (inflammatory cell infiltration in the liver), hepatocyte ballooning, and hepatic cirrhosis associated with NAFLD. In Korea the prevalence of fatty liver may be as high as 25-30% [1], 10-15% of whom may have steatohepatitis with inflammation. In clinical practice, NASH, including inflammation and fibrosis, is an important diagnosis, and sometimes leads to hepatic cirrhosis and liver cancer. Currently, NAFLD is the most common chronic liver disease in developed countries.
Unresolved issues relating to NAFLD are the absence of effective diagnostic methods and satisfactory treatments. This study will provide a description of diagnostic methods and treatments that are currently recommended for NAFLD.
DIAGNOSIS OF NAFLD: NON-INVASIVE METHOD I (radiologic method)
1. Ultrasonography
Abdominal ultrasonography (US) is one of the most widely used one of the fatty liver in clinical practice. It is relatively inexpensive and has a sensitivity of 93%, high enough to diagnose a moderately fatty liver with more than 33% fat [2]. However, US shows low specificity and low sensitivity if the liver is composed of less than 30% fat. There also may be a difference in diagnosis due to variations in the interpretations of the readers of the ultrasonograms [2].
2. Computed tomography
Abdominal computed tomography (CT) produces different radiolucency depending on the individual organ examined. The measurement of this radiolucency is called the Hounsfield unit (HU), named after an English electrical engineer who discovered this variation. In general, the calibration of images of body tissues is normalized based on values for air (-1,000 HU), water (0 HU), and bone density (+1,000 HU). Unenhanced abdominal CT uses liver HU and spleen HU to determine the degree of steatosis. The liver, which has a value of 60±10 HU, normally looks brighter than the spleen, blood vessels or biliary tract, while subcutaneous fat represents a value of -90 HU [3]. Increased fat accumulation in the liver may lead to a liver HU that is lower than spleen HU. Generally, liver HU ≤40 HU, or liver minus spleen density difference less than -10 HU, or liver/spleen ratio of ≤0.9, which can lead to the diagnosis of hepatic steatosis [3]. However, there are several disadvantages to this method. Radiation exposure, or HU, can differ depending on the set-up of CT machines by suppliers and installers, and HU can be affected by various conditions, such as accompanying edema or accumulation of copper in liver. CT is not superior to ultrasonography in the assessment of hepatic steatosis, but CT can suggest quantitative and objective values in comparison with ultrasonography.
3. Multi-parametric magnetic resonance imaging (MRI) of quantitative fat
Hydrogen in fat is different in resonance from hydrogen in water. Magnetic resonance imaging proton density fat fraction (MRI-PDFF) has been widely used to estimate the level of hepatic triglycerides by calculating the fraction of triglycerides versus hydrogen in water. The sensitivity and specificity of MRI-PDFF using a multi-echo technique to estimate intrahepatic fat amount is nearly perfect [4,5]. MRI-PDFF is known as a reference standard in the field of radiology to measure the amount of hepatic fat [6]. Such MRI-based hepatic fat measurement has been used by a number of multinational corporations that produce MRI machines, such as IDEAL IQ® (GE), mDixon Qant® (Philips), and Multiecho VIBE Dixon® (Siemens). Additionally, clinical use has been approved by the Federal Drug Administration (FDA) in the U.S., in which MRI-PDFF can be a substitute for liver biopsy in randomized controlled trials that use hepatic fat change as the primary variable [7,8]. MRI-PDFF values are: 0-6.4% for grade 0 (normal) with less than 5% hepatic fat from tissue biopsy; 6.5-17.5% for grade 1 (mild) with 5-33% hepatic fat; 17.5-22.1% for grade 2 (moderate) with 33-66% hepatic fat; and 22.2% or greater for grade 3 (severe) with more than 66% hepatic fat [9,10]. Nonetheless, it is difficult for primary care and other facilities to use this high-cost equipment universally. But the most important limitation of MRI-PDFF is that it can estimate the intrahepatic fat amount almost perfectly, but cannot detect the difference between NASH and NAFLD.
DIAGNOSIS OF NAFLD : NON-INVASIVE METHOD II (serologic method)
There are three serologic methods used to diagnose NAFLD; the first, a test for predicting hepatic steatosis; the second, a method for determining NASH, and lastly, a test for detecting advanced fibrosis ≥F3.
1. Serologic testing for simple steatosis
The fatty liver index [11] and SteatoTest [12] have been developed to detect simple steatosis, but are not in widespread use due to the availability of advanced imaging tools, such as ultrasonography or MR imaging-PDFF.
2. Serologic testing for NASH
Although radiologic assessment of NASH has improved, no radiologic method can detect a difference between NASH and NAFLD. Many studies on serological surrogate markers are used to distinguish steatohepatitis from the inflammation of simple steatosis, and single serological test methods to predict steatohepatitis have also been studied. Although the recommended surrogate markers TNF-α, IL-6, CRP, Pantraxin, Ferritin, SPEA, and sRAGE predict hepatic inflammation, most of these markers still need extensive external validation (Table 1) [13-19]. The single test most studied so far in regard to the diagnosis of NASH is Cytokeratin-18 (CK-18). The CK-18 fragment, a marker of hepatocyte apoptosis, predicts nonalcoholic steatohepatitis, which is significantly increased compared with normal or simple steatosis. CK-18 showed relatively good results (sensitivity 78%, specificity 87%, areas under the receiver-operating curve (AUROC) 0.82) in some precedent studies, demonstrating the potential for screening nonalcoholic steatohepatitis. However, with CK-18 in clinical application demonstrates a large variation in cut-off values compared to previous studies, and its sensitivity and specificity to predict steatohepatitis was not satisfactory [20]. A meta-analysis using 11 recent studies shows that AUROC for NASH ranged from 0.71-0.93, sensitivity was 66%, and specificity was 82%. Optimal cut-off values may increase sensitivity to 82% and specificity to 98%, but there is a wide variation in cut-off values reported by each researcher (optimal cut off 136 – 338 U/L) [21]. For this reason, the American Association for the Study of Liver Diseases (AASLD) as well as practitioners in Korea have not recommended the use of CK-18 for diagnosis and treatment of NASH.
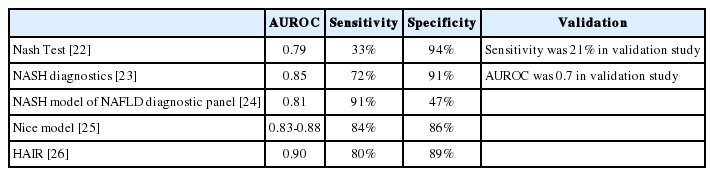
The Nash Test [22], NASH diagnostics [23], NASH model of NAFLD diagnostic panel [24], Nice model [25], and HAIR score [26] have been suggested as biochemical tests to predict NASH, but in most studies , sensitivity was low and AUROC values were unsatisfactory (Table 2). However, the biggest drawback is that most models have not been validated externally, indicating that further studies are needed for confirmation. For instance, HAIR has a relatively high AUROC, sensitivity, and specificity, but also has the limitation of efficacy only in the severely obese patient, with no external validation for other NASH patients [26].
3. Advanced fibrosis ≥F3
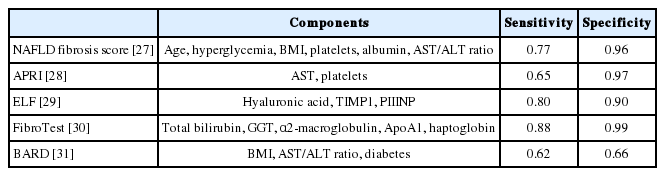
NAFLD fibrosis score [27], APRI (AST-to-platelet ratio index) [28], ELF (enhanced liver fibrosis panel) [29], FibroTest [30] and BARD [31] have been studied to predict advanced fibrosis ≥F3 (Table 3) in NAFLD patients. ELF (Hyaluronic acid, TIMP1, PIIINP) and FibroTest (α2-macroglobulin, ApoA1, haptoglobin) use direct markers from collagen synthesis and degradation, while the NAFLD fibrosis score and APRI exploit biochemical test components, such as age, glucose, body mass index, platelets and albumin, which are commonly used in clinical practice.
The NAFLD Fibrosis score has been studied extensively studied worldwide. It is composed of six markers (age, hyperglycemia, BMI, platelet, albumin, and AST/ALT ratio), which are clinically or biochemically measured easily. The NAFLD fibrosis score typically uses low and high cut-off values. When a low cut-off value (-1.455) was used, a negative predictive value (NPV) for predicting without advanced fibrosis (< F3) was 93%, and when a high cut-off value (0.676) was used, the positive predictive value (PPV) for predicting advanced fibrosis (≥ F3) was 90% [27]. Since then, the NAFLD fibrosis score has been validated externally in Western countries, demonstrating relatively reliable predictability compared to other models for prediction of fibrosis. However, the results of studies on external validation using the NAFLD fibrosis score conducted in Eastern countries showed somewhat different results. One study conducted on 162 NAFLD patients in Hong Kong indicated NPVs of low cut-off value were very high at 91%, while PPVs of high cut-off value were 0% [32]. In a Hong Kong cohort of obese subjects (average BMI 28.5) , only 18 patients (11%) had advanced fibrosis ≥F3 [32]. In a Japanese multicenter study conducted on 588 subjects showed the NPV of low cut-off was 98%, while the PPV of high cut-off was 43% [33]. Advanced fibrosis ≥F3 was detected in 27.8% of these subjects [33]. In a study on external validation of the NAFLD fibrosis score using a Korean cohort, AUROC to predict advanced fibrosis was high at 0.964. The NPV of low cut-off was 100%, while the PPV of high cut-off was 33.3% [34]. Therefore, the use of PPV with a high cut-off in Asian countries in patients with low advanced fibrosis needs further study.
DIAGNOSIS OF NAFLD: AN INVASIVE METHODS (liver biopsy)
Currently, liver biopsy is the gold standard for diagnosis of NAFLD. However, this method still has several unresolved issues. Occasionally, advanced NASH-associated cirrhosis may not demonstrate fat in the liver, and is called “burned-out cirrhosis.” This condition can’t be easily distinguished from cryptogenic cirrhosis. Perisinusoidal fibrosis, ballooning hepatocytes, and Mallory-Denk bodies found in non-alcoholic patients may be a clue for NASH-associated cirrhosis, but it is difficult to distinguish from “burned-out” cirrhosis unless confirmed by biopsy. Also, liver biopsy utilizes only a small section of the liver (1/50,000th), and different positions may lead to different results. In regard to steatosis, the extent of fat accumulation varies depending upon in which segment it is located, as the amount of hepatic fat is significantly higher in the right lobe than the left [35]. There are significant differences in the amount of intrahepatic fat between the various lobes and segments [35]. In addition, needle biopsy and surgical biopsy can result in different findings for the same organ, as anesthesia during a surgical biopsy may cause minor or “surgical” hepatitis [36]. In many cases, liver tissue can be obtained from the surface of the liver rather than its central core. Surface tissue often presents an expanded portal vein and exaggerated fibrosis. Also, observer-to-observer agreement may be low in the interpretation the liver biopsy. Finally, though several diagnostic criteria for NASH are recommended, there are no unified standards at the present time. Currently, three standards are being used for histological diagnosis of NASH in clinical practice, the Brunt system, NASH CRN, and the SAF/FLIP algorithm. The Brunt system is the prototype of histological diagnostic criteria for nonalcoholic fatty liver diseases [37]. This system divides steatosis, hepatocyte ballooning degeneration, lobular and portal vein inflammation into three types; mild, moderate and severe and classifies liver fibrosis into 4 stages [37]. It stresses hepatocyte ballooning, fatty accumulation in the liver, and inflammatory cell infiltration, especially on damage in zone 3. However, this system has not been corroborated extensively by other researchers. NAS is recommended by the non-alcoholic steatohepatitis Clinical Research Network (CRN), and its clinical usefulness has been validated by a number of researchers [38]. NAS was not designed to diagnose NASH. but it was designed to assess treatment efficacy in a clinical study on fatty liver diseases. The NAS system contains components that determine fibrosis, but the NAS score itself does not include a determination of fibrosis. For this reason, there are cases with advanced hepatic fibrosis and low NAS scores or the exact opposite. Twenty-eight percent of obvious NASH patients scored less than 5 points in the study, while 7% of obvious non-NASH patients scored more than 5 points [39]. Recently, the European Fatty Liver Inhibition of Progression (FLIP) group has recommended the SAF score [40,41]. SAF, a scoring system for Steatosis, Activity (inflammation), and Fibrosis, puts weight on hepatic fibrosis and hepatocyte ballooning to diagnose NASH, unlike the NAS score. SAF also has the advantage of less difference in interpretation by multiple observers. Worldwide consensus on diagnostic criteria and severity in NASH should be developed.
In spite of the issues listed above, liver biopsy is still the gold standard in practice and clinical trial. Globally unified standards for histological diagnosis, methods to enhance agreement in interpretation, and standardization of biopsy sites and methods still require resolution.
TREATMENT UPDATE ON NAFLD
1. Lifestyle modification
The treatment of NAFLD is based on weight loss achieved by lifestyle modification. A minimum of 5% weight loss decreases hepatic fat, and a 7-10% weight loss is required to improve hepatic inflammation [42,43]. However, it is difficult for diet and exercise regimens to achieve and maintain a 10% weight loss. In a recent study conducted in Cuba, a low calorie diet and modification of habits achieved a 30% weight loss in subjects for one year [44]. However, only 19% of the subjects achieved improvement in hepatic fibrosis. Instead, 16% of them had advanced hepatic fibrosis. Though modification of habit and diet is the foundation for the treatment of nonalcoholic fatty liver disease, there still exists a lack of randomized controlled trials on diet, modification of habit, and weight loss on the improvement of NASH and hepatic fibrosis. In the past, aerobic exercise was considered a better way to reduce hepatic fat than weight training, but recent studies show that a combination of aerobic exercise and weight training is more effective than an aerobic exercise alone.
2. Pharmacotherapy
In some randomized controlled trials, the effect of vitamin E and obeticholic acid on nonalcoholic fatty liver diseases has been proven [45,46], but these drugs have not been approved in most countries. The following drugs are used off-label for NAFLD in Korea.
FXR agonist (Obeticholic acid, Intercept, Phase IIb): Farnesoid X Receptor (FXR) agonist (obeticholic acid) has significantly decreased hepatic inflammation in large scale clinical trial in patients with NASH [46]. However, at the same time obeticholic acid has significantly increased blood triglyceride and LDL-cholesterol levels and decreased HDL-cholesterol concentration. Given that many NASH patients die due to cardiovascular diseases, an increased blood cholesterol level due to the use of obeticholic acid is problematic [47]. Recently, intestine-specific FXR agonist has been investigated. This new FXR agonist has reduced inflammatory cell infiltration around fat cells and improved insulin resistance, with a decline in hepatic fat and inflammation in preclinical studies. In addition, the intestine-specific FXR agonist did not increase cholesterol and triglyceride concentration [48]. Further studies on human subjects are warranted.
NOX-1/4 Inhibitor (GKT137831, Genkyotex): GKT137831 is a first-in-class drug targeting NADPH oxidase (NOX) 1 and 4. GKT137831 was designed as an anti-diabetic drug. The NOX1/4 inhibitor failed to reduce albuminuria in patients with diabetic nephropathy, but it showed an excellent safety profile. GKT137831 extended its therapeutic targets, including atherosclerosis, idiopathic pulmonary fibrosis, liver fibrosis, and models of angiogenesis. NOX embedded in inflammatory and hepatic stellate cells plays a crucial role in the outbreak of hepatic inflammation and fibrosis. The overexpression of NOX 1 and 4 in tissue from patients with liver cirrhosis and NASH confirms the accuracy of the preclinical models. The NOX1/4 inhibitor has had a favorable effect on the inhibition of hepatic inflammation and fibrosis in animal testing [49]. Another interesting finding in preclinical data is that the NOX1/4 inhibitor decreases hepatocyte apoptosis.
Galectin-3 inhibitor (GR-MD-02, Galectin Therapeutics, Phase II): Galectin-3, a kind of carbohydrate-binding protein, is bound to the galactose residues of large proteins such as glycoprotein. Galectin-3 normally expresses in immune cells at a very low concentration and increases inflammation [50]. Galectin-3 antagonist has demonstrated an outstanding result in animal study. Galectin-3 knock-out mice have had lesser hepatic fibrosis. GR-MD-02 (Galectin Therapeutics, Inc, Norcross, GA, USA) has no obviously identified mechanism, but acts as an antagonist on galectin. In a phase I study on 31 subjects with biopsy-proven NASH with advanced fibrosis (Brunt stage 3), a high dose of GR-MD-02 (8mg/kg) administered for 6 weeks was relatively safe and lowered FibroTest® and α2-macroglobulin levels. At this time, GR-MD-02 is undergoing Phase II clinical trials for safety and efficacy (ClinicalTrial.gov NCT02462967).
CCR2 and CCR5 inhibitor (Cenicriviroc, Tobira, Phase IIb): C-C chemokine receptor (CCR) is expressed in diverse immune cells, including monocytes, macrophagocytes, and hepatic Kupffer cells. Cenicriviroc® was developed as anti-viral agent in HIV-1 patients. It has shown effective antiviral activity and safety in recent phase IIb clinical trials in patient with AIDS. Cenicriviroc® also activated hepatic stellate cells and hepatic fibrosis [51]. Cenicriviroc® has induced histological improvement in both models of diet-inducing steatosis and hepatic fibrosis in animals. Currently, clinical studies on NASH patients with CENTAUR using Cenicriviroc® are in progress [51], awaiting the results of Cenicriviroc® safety and efficacy (ClinicalTrial.gov NCT02217475).
Pan-caspase inhibitor (Emricasan, Conatus Pharmaceuticals, Inc., Phase IIa): This anti-apoptotic drug has already received attention as a potential target for NASH, because hepatocyte apoptosis is the most important step in developing NASH. For this reason, hepatocyte ballooning, which is surrogate marker of hepatocyte apoptosis, is important in the diagnosis of liver pathology. Emricasan® suppressed liver injury and fibrosis by inhibiting hepatocytes apoptosis [52]. In a phase II clinical study on 38 NASH patients, Emricasan® lowered serum aminotransferase activity and cleaved CK-8 serum concentration [53]. Emricasan® has been studied across a broad range of liver disease etiologies and stages of progression, and has demonstrated meaningful reductions in hepatic venous pressure gradient (HVPG) in cirrhotic patients. ENCORE trials designed to evaluate fibrosis and inflammation in patients with NASH fibrosis showed improvement in HVPG in NASH cirrhosis in November of 2015. Recently the U.S. FDA has granted Fast Track designation to the company’s Emricasan® development program for the treatment of cirrhosis caused by nonalcoholic steatohepatitis.
PPAR-α/δ agonist (GFT505, Genfit, Phase IIb): This agent was developed as a PPAR-α/δ agonist, and is already known for mitigation of hepatic fat and relief of inflammation. Very little is known of the role of PPAR-δ, but it has the effect of improving the function of mitochondria, fat burning, and insulin resistance. In a large-scale randomized controlled trial on 274 NASH patients, GFT505 did not significantly decrease hepatic inflammation [54]. However, when administered to a subgroup with the NAS score≥4 before treatment, GFT505 induced significant improvement in hepatic inflammation. Further studies on target groups and timing of optimal clinical application of GFT505 are in progress.
SCD-1 inhibitor (Aramchol, Galmed, Phase IIb): Stearoyl-CoA desaturase-1 (SCD-1), an enzyme essential to neutral lipid synthesis, has a strong effect on controlling neutral lipid biosynthesis. In a study conducted for 3 months on 60 patients with NASH confirmed by liver biopsy, Aramchol® showed a significant decrease in hepatic fat of roughly 12.6% [6]. However, only 6 (10%) of the above subjects were NASH patients, and the anti-fibrotic effect was not evaluated. Currently, a phase IIb clinical study of 240 NASH patients treated with Aramchol® is in progress, and is attempting to determine the level of hepatic fibrosis and hepatic inflammation in a non-invasive way (ClincialTrails.gov NCT02279524).
Apoptosis signal-regulating kinase 1 inhibitor (GS-4997, Gilead, Phase II): Apoptosis signal-regulating kinase 1 (ASK1) is activated by various stimuli, including hyperglycemia, TGF-β, and oxidative stimulus in the body. Activated ASK1 induces apoptosis and fibrosis through p38 and JNK1. In the animal NASH model, the ASK1 antagonist induced a decrease in hepatic fat and fibrosis. It also induced improvement in insulin resistance and metabolic index by prompting weight loss [55]. Presently, a phase II clinical study on the ASK1 antagonist (GS-4997) is in progress testing NASH patients with moderate steatosis and advanced fibrosis (ClinicalTrial.gov NCT02466516).
Lysyk oxidase-like 2 inhibitor (Simtuzumab, Gilead, Phase IIb): This drug strengthens collagen binding in the extracellular matrix to restrain decomposition. In the hepatic cirrhosis model, more LOXL2 appeared. In the animal model, the LOXL2 monoclonal antibody restrained hepatic fibrosis [56]. A phase IIb study on the inhibition of hepatic fibrosis and cirrhosis in nonalcoholic fatty liver disease treated with Simtuzumab (Gilead Sciences, Foster City, USA) is in progress. This study, targeting 222 NASH patients, follows patients for 6 years to assess the incidence of hepatic cirrhosis (ClincialTrial.gov NCT01672866). At the same time, a phase IIb clinical study on the safety and efficacy of simtuzumab for steatosis associated hepatic cirrhosis patients is in progress (ClincalTrial. gov NCT01672879). This study will target patients with compensated liver cirrhosis, assess the incidence of associated complications of hepatic cirrhosis. Simtuzumab will be studied with a reduced amount of HVPG after treatment for a maximum of 6 years with subsequent HVPG measurement. The study is expected to be completed in 2024.
Notes
Conflicts of Interest: The authors have no conflicts to disclose.
Abbreviations
AUROC
areas under the receiver-operating curve
CK-18
cytokeratin-18
CT
computed tomography
HU
Hounsfield unit
FXR
farnesoid X receptor
MRS
magnetic resonance spectroscopy
NAFLD
non-alcoholic fatty liver disease
NASH
non-alcoholic steatohepatitis
NFS
NAFLD Fibrosis Score
NPV
negative predictive value
PDFF
proton density fat fraction
PPV
positive predictive value
SAF
scoring system for steatosis, activity, and fibrosis