1. Xu J, Murphy SL, Kochanek KD, Bastian B, Arias E. Deaths: final data for 2016. Natl Vital Stat Rep 2018;67:1-76.
2. Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet 2014;383:1749-1761.


3. Crager S. Critically ill patients with end-stage liver disease. Emerg Med Clin North Am 2019;37:511-527.


9. Nagamoto Y, Takayama K, Ohashi K, Okamoto R, Sakurai F, Tachibana M, et al. Transplantation of a human iPSC-derived hepatocyte sheet increases survival in mice with acute liver failure. J Hepatol 2016;64:1068-1075.


10. Wang H, Wang D, Yang L, Wang Y, Jia J, Na D, et al. Compact bone-derived mesenchymal stem cells attenuate nonalcoholic steatohepatitis in a mouse model by modulation of CD4 cells differentiation. Int Immunopharmacol 2017;42:67-73.


13. Saad El-Din S, Fouad H, Rashed LA, Mahfouz S, Hussein RE. Impact of mesenchymal stem cells and vitamin D on transforming growth factor beta signaling pathway in hepatocellular carcinoma in rats. Asian Pac J Cancer Prev 2018;19:905-912.


16. Muguruma K. 3D Culture for self-formation of the cerebellum from human pluripotent stem cells through induction of the isthmic organizer. Methods Mol Biol 2017;1597:31-41.


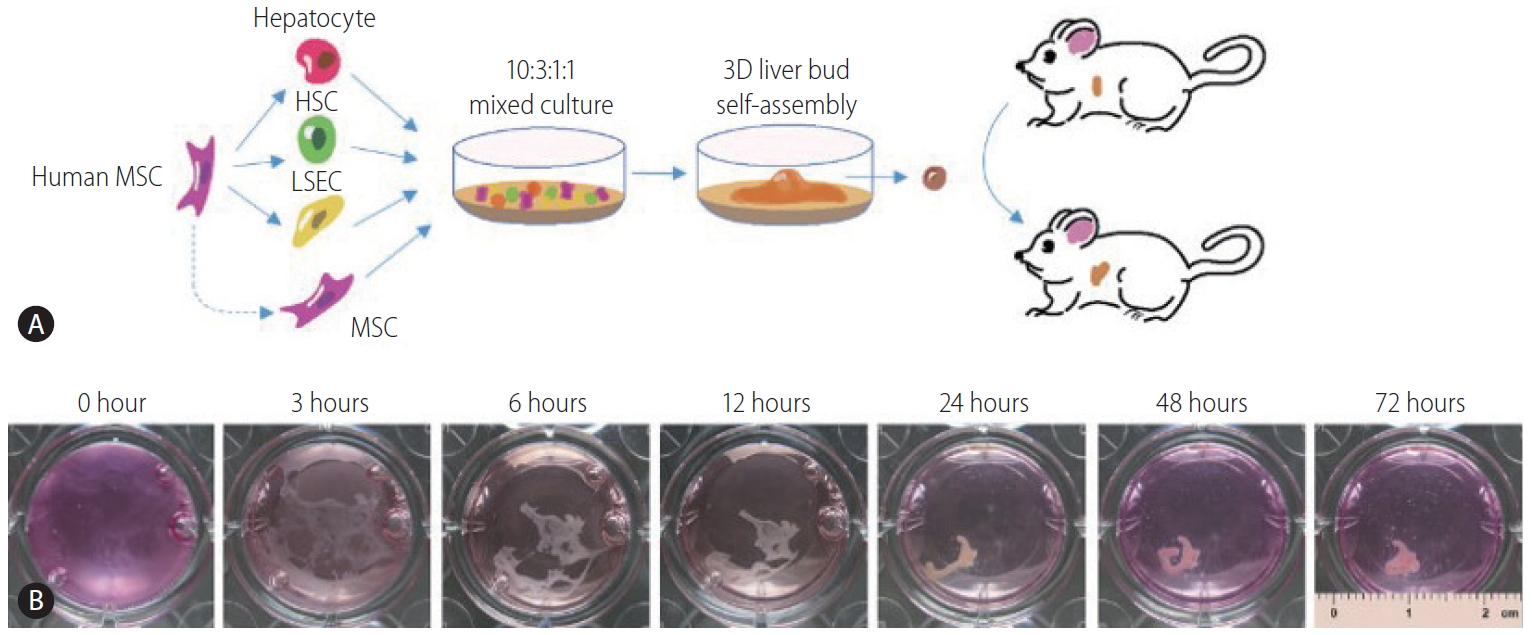
17. Takebe T, Sekine K, Kimura M, Yoshizawa E, Ayano S, Koido M, et al. Massive and reproducible production of liver buds entirely from human pluripotent stem cells. Cell Rep 2017;21:2661-2670.


18. Takebe T, Enomura M, Yoshizawa E, Kimura M, Koike H, Ueno Y, et al. Vascularized and complex organ buds from diverse tissues via mesenchymal cell-driven condensation. Cell Stem Cell 2015;16:556-565.


20. Xie PY, Hu XJ, Guo RM, Meng XC, Pang PF, Zhou ZY, et al. Generation of functional hepatocyte-like cells from human bone marrow mesenchymal stem cells by overexpression of transcription factor HNF4α and FOXA2. Hepatobiliary Pancreat Dis Int 2019;18:546-556.


25. Fukuda T, Takayama K, Hirata M, Liu YJ, Yanagihara K, Suga M, et al. Isolation and expansion of human pluripotent stem cell-derived hepatic progenitor cells by growth factor defined serum-free culture conditions. Exp Cell Res 2017;352:333-345.


27. Mazza G, Al-Akkad W, Rombouts K. Engineering in vitro models of hepatofibrogenesis. Adv Drug Del Rev 2017;121:147-157.

29. Saito Y, Morine Y, Shimada M. Mechanism of impairment on liver regeneration in elderly patients: role of hepatic stellate cell function. Hepatol Res 2017;47:505-513.


30. Geerts A. On the origin of stellate cells: mesodermal, endodermal or neuro-ectodermal? J Hepatol 2004;40:331-334.


31. Baba S, Fujii H, Hirose T, Yasuchika K, Azuma H, Hoppo T, et al. Commitment of bone marrow cells to hepatic stellate cells in mouse. J Hepatol 2004;40:255-260.


33. Tan KS, Kulkeaw K, Nakanishi Y, Sugiyama D. Expression of cytokine and extracellular matrix mRNAs in fetal hepatic stellate cells. Genes Cells 2017;22:836-844.


34. Kordes C, Sawitza I, Götze S, Schumacher E, Häussinger D. Beyond fibrosis: stellate cells as liver stem cells. Z Gastroenterol 2015;53:1425-1431.


35. Coll M, Perea L, Boon R, Leite SB, Vallverdú J, Mannaerts I, et al. Generation of hepatic stellate cells from human pluripotent stem cells enables invitro modeling of liver fibrosis. Cell Stem Cell 2018;23:101-113 e7.


36. Xu M, Wang X, Zou Y, Zhong Y. Key role of liver sinusoidal endothelial cells in liver fibrosis. Biosci Trends 2017;11:163-168.


37. Poisson J, Lemoinne S, Boulanger C, Durand F, Moreau R, Valla D, et al. Liver sinusoidal endothelial cells: physiology and role in liver diseases. J Hepatol 2016;66:212-227.


40. Du C, Narayanan K, Leong MF, Wan AC. Induced pluripotent stem cell-derived hepatocytes and endothelial cells in multi-component hydrogel fibers for liver tissue engineering. Biomaterials 2014;35:6006-6014.


43. Rubio-Tomás T, Aguilar-Bravo B, Sancho-Bru P. Genetic lineage tracing of biliary epithelial cells. Methods Mol Biol 2019;1905:45-57.


45. Raynaud P, Carpentier R, Antoniou A, Lemaigre FP. Biliary differentiation and bile duct morphogenesis in development and disease. Int J Biochem Cell Biol 2011;43:245-256.


49. Li P, He K, Li J, Liu Z, Gong J. The role of Kupffer cells in hepatic diseases. Mol Immunol 2017;85:222-229.


51. Chhabra A, Chen IP, Batra D. Human dendritic cell-derived induced pluripotent stem cell lines are not immunogenic. J Immunol 2017;198:1875-1886.


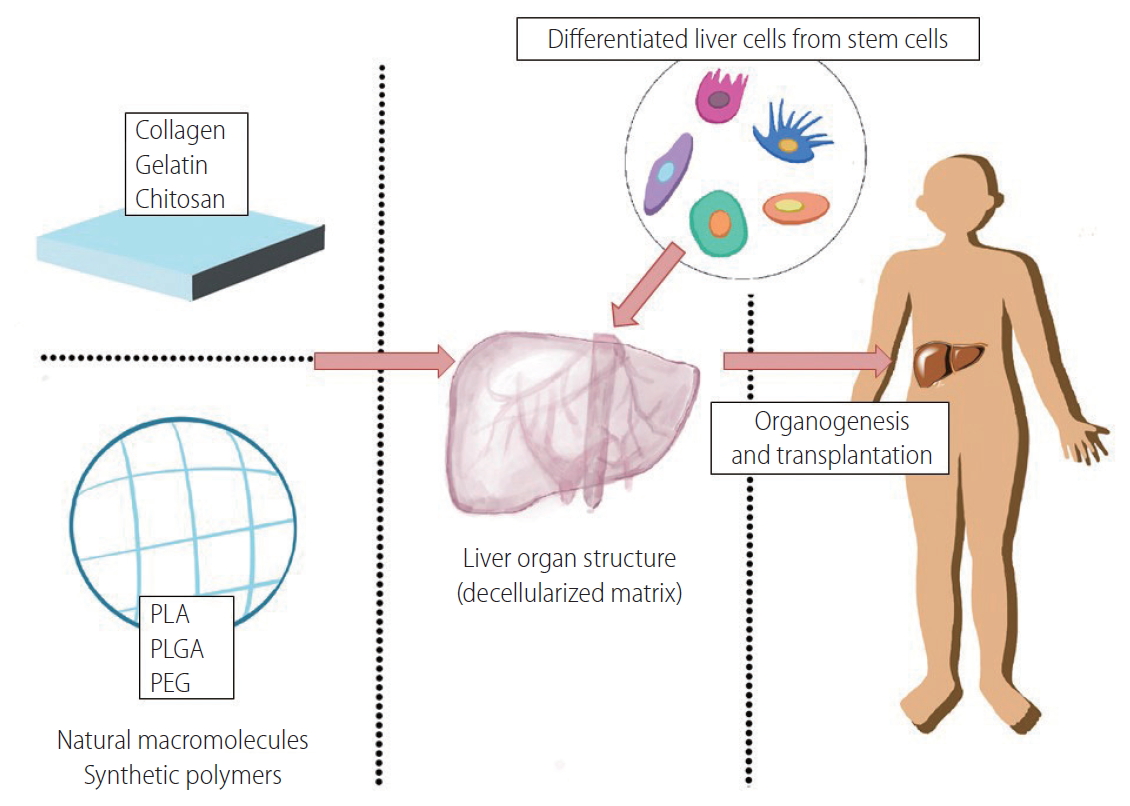
53. Baptista PM, Siddiqui MM, Lozier G, Rodriguez SR, Atala A, Soker S. The use of whole organ decellularization for the generation of a vascularized liver organoid. Hepatology 2011;53:604-617.


54. Waring P, Mullbacher A. Cell death induced by the Fas/Fas ligand pathway and its role in pathology. Immunol Cell Biol 1999;77:312-317.


55. Tasnim F, Xing J, Huang X, Mo S, Wei X, Tan MH, et al. Generation of mature kupffer cells from human induced pluripotent stem cells. Biomaterials 2019;192:377-391.


57. Zhang J, Zhao X, Liang L, Li J, Demirci U, Wang S. A decade of progress in liver regenerative medicine. Biomaterials 2018;157:161-176.


58. He L, Tian L, Sun Y, Zhang Y, Xue W, So KF, et al. Nano-engineered environment for nerve regeneration: scaffolds, functional molecules and stem cells. Curr Stem Cell Res Ther 2016;11:605-617.


61. Yang W, Xia R, Zhang Y, Zhang H, Bai L. Decellularized liver scaffold for liver regeneration. Methods Mol Biol 2017;1577:11-23.

63. Lin P, Chan WC, Badylak SF, Bhatia SN. Assessing porcine liver-derived biomatrix for hepatic tissue engineering. Tissue Eng 2004;10:1046-1053.


65. Park KM, Hussein KH, Hong SH, Ahn C, Yang SR, Park SM, et al. Decellularized liver extracellular matrix as promising tools for transplantable bioengineered liver promotes hepatic lineage commitments of induced pluripotent stem cells. Tissue Engineering Part A 2016;22:449-460.


66. Coronado RE, Somaraki-Cormier M, Ong JL, Halff GA. Hepatocyte-like cells derived from human amniotic epithelial, bone marrow, and adipose stromal cells display enhanced functionality when cultured on decellularized liver substrate. Stem Cell Res 2019;38:101471.


67. Xiang JX, Zheng XL, Gao R, Wu WQ, Zhu XL, Li JH, et al. Liver regeneration using decellularized splenic scaffold: a novel approach in tissue engineering. Hepatobiliary Pancreat Dis Int 2015;14:502-508.


68. Liu P, Tian B, Yang L, Zheng X, Zhang X, Li J, et al. Hemocompatibility improvement of decellularized spleen matrix for constructing transplantable bioartificial liver. Biomed Mater 2019;14:025003.


69. Taylor DA, Sampaio LC, Ferdous Z, Gobin AS, Taite LJ. Decellularized matrices in regenerative medicine. Acta Biomater 2018;74:74-89.


70. Watari R, Kakiki M, Oshikata A, Takezawa T, Yamasaki C, Ishida Y, et al. A long-term culture system based on a collagen vitrigel membrane chamber that supports liver-specific functions of hepatocytes isolated from mice with humanized livers. J Toxicol Sci 2018;43:521-529.


71. Khodabandeh Z, Vojdani Z, Talaei-Khozani T, Jaberipour M, Hosseini A, Bahmanpour S. Comparison of the expression of hepatic genes by human Wharton’s jelly mesenchymal stem cells cultured in 2D and 3D collagen culture systems. Iran J Med Sci 2016;41:28-36.


76. Ghaderi Gandomani M, Sahebghadam Lotfi A, Kordi Tamandani D, Arjmand S, Alizadeh S. The enhancement of differentiating adipose derived mesenchymal stem cells toward hepatocyte like cells using gelatin cryogel scaffold. Biochem Biophys Res Commun 2017;491:1000-1006.


77. Mohammadpour A, Arjmand S, Lotfi AS, Tavana H, Kabir-Salmani M. Promoting hepatogenic differentiation of human mesenchymal stem cells using a novel laminin-containing gelatin cryogel scaffold. Biochem Biophys Res Commun 2018;507:15-21.


78. German CL, Madihally SV. Type of endothelial cells affects HepaRG cell acetaminophen metabolism in both 2D and 3D porous scaffold cultures. J Appl Toxicol 2019;39:461-472.


79. Yan Y, Wang X, Pan Y, Liu H, Cheng J, Xiong Z, et al. Fabrication of viable tissue-engineered constructs with 3D cell-assembly technique. Biomaterials 2005;26:5864-5871.


81. Feng ZQ, Chu X, Huang NP, Wang T, Wang Y, Shi X, et al. The effect of nanofibrous galactosylated chitosan scaffolds on the formation of rat primary hepatocyte aggregates and the maintenance of liver function. Biomaterials 2009;30:2753-2763.


82. Rajendran D, Hussain A, Yip D, Parekh A, Cho CH. Long-term liver-specific functions of hepatocytes in electrospun chitosan nanofiber scaffolds coated with fibronectin. J Biomed Mater Res A 2017;105:2119-2128.


83. Fan L, Zou S, Ge H, Xiao Y, Wen H, Feng H, et al. Preparation and characterization of hydroxypropyl chitosan modified with collagen peptide. Int J Biol Macromol 2016;93(Pt A):636-643.


84. Li L, Zhang Y, Pan X. Preparation and characterization of alginatechitosan microcapsule for hepatocyte culture. Methods Mol Biol 2017;1479:199-206.


85. Fan J, Yang J. Preparation and characterization of a chitosan/galactosylated hyaluronic acid/heparin scaffold for hepatic tissue engineering. J Biomater Sci Polym Ed 2017;28:569-581.


87. Tran NM, Dufresne M, Duverlie G, Castelain S, Défarge C, Paullier P, et al. An appropriate selection of a 3D alginate culture model for hepatic Huh-7 cell line encapsulation intended for viral studies. Tissue Eng Part A 2013;19:103-113.


89. Lau TT, Ho LW, Wang DA. Hepatogenesis of murine induced pluripotent stem cells in 3D micro-cavitary hydrogel system for liver regeneration. Biomaterials 2013;34:6659-6669.


90. Shteyer E, Ben Ya’acov A, Zolotaryova L, Sinai A, Lichtenstein Y, Pappo O, et al. Reduced liver cell death using an alginate scaffold bandage: a novel approach for liver reconstruction after extended partial hepatectomy. Acta Biomater 2014;10:3209-3216.


91. Varaa N, Azandeh S, Khorsandi L, Bijan Nejad D, Bayati V, Bahreini A. Ameliorating effect of encapsulated hepatocyte-like cells derived from umbilical cord in high mannuronic alginate scaffolds on acute liver failure in rats. Iran J Basic Med Sci 2018;21:928-935.


92. Shao H, Li T, Zhu R, Xu X, Yu J, Chen S, et al. Carbon nanotube multilayered nanocomposites as multifunctional substrates for actuating neuronal differentiation and functions of neural stem cells. Biomaterials 2018;175:93-109.


93. Abbasian M, Massoumi B, Mohammad-Rezaei R, Samadian H, Jaymand M. Scaffolding polymeric biomaterials: are naturally occurring biological macromolecules more appropriate for tissue engineering? Int J Biol Macromol 2019;134:673-694.


94. Oana C, Adriana T, Mircea C, Dragos S, Monica H. Natural macromolecules with protective and antitumor activity. Anticancer Agents Med Chem 2018;18:675-683.


96. Hanada S, Kayano H, Jiang J, Kojima N, Miyajima A, Sakoda A, et al. Enhanced in vitro maturation of subcultivated fetal human hepatocytes in three dimensional culture using poly-L-lactic acid scaffolds in the presence of oncostatin M. Int J Artif Organs 2003;26:943-951.


97. Jiang J, Kojima N, Guo L, Naruse K, Makuuchi M, Miyajima A, et al. Efficacy of engineered liver tissue based on poly-L-lactic acid scaffolds and fetal mouse liver cells cultured with oncostatin M, nicotinamide, and dimethyl sulfoxide. Tissue Eng 2004;10:1577-1586.


99. Mobarra N, Soleimani M, Pakzad R, Enderami SE, Pasalar P. Three-dimensional nanofiberous PLLA/PCL scaffold improved biochemical and molecular markers hiPS cell-derived insulin-producing islet-like cells. Artif Cells Nanomed Biotechnol 2018;46(sup3):S685-S692.


100. Mobarra N, Soleimani M, Ghayour-Mobarhan M, Safarpour S, Ferns GA, Pakzad R, et al. Hybrid poly‐l‐lactic acid/poly(ε‐caprolactone) nanofibrous scaffold can improve biochemical and molecular markers of human induced pluripotent stem cell‐derived hepatocyte‐ like cells. J Cell Physiol 2019;234:11247-11255.


101. Ranucci CS, Moghe PV. Polymer substrate topography actively regulates the multicellular organization and liver-specific functions of cultured hepatocytes. Tissue Eng 1999;5:407-420.


102. Kasuya J, Sudo R, Tamogami R, Masuda G, Mitaka T, Ikeda M, et al. Reconstruction of 3D stacked hepatocyte tissues using degradable, microporous poly(d,l-lactide-co-glycolide) membranes. Biomaterials 2012;33:2693-2700.


103. Liu T, Zhang S, Chen X, Li G, Wang Y. Hepatic differentiation of mouse embryonic stem cells in three-dimensional polymer scaffolds. Tissue Eng Part A 2010;16:1115-1122.


104. Zhang K, Zheng H, Liang S, Gao C. Aligned PLLA nanofibrous scaffolds coated with graphene oxide for promoting neural cell growth. Acta Biomater 2016;37:131-142.


105. Zhang K, Huang D, Yan Z, Wang C. Heparin/collagen encapsulating nerve growth factor multilayers coated aligned PLLA nanofibrous scaffolds for nerve tissue engineering. J Biomed Mater Res A 2017;105:1900-1910.


106. Kojima N, Matsuo T, Sakai Y. Rapid hepatic cell attachment onto biodegradable polymer surfaces without toxicity using an avidinbiotin binding system. Biomaterials 2006;27:4904-4910.


108. Bierwolf J, Lutgehetmann M, Feng K, Erbes J, Deichmann S, Toronyi E, et al. Primary rat hepatocyte culture on 3D nanofibrous polymer scaffolds for toxicology and pharmaceutical research. Biotechnol Bioeng 2015;108:141-150.

109. Hay DC, Zhao D, Fletcher J, Hewitt ZA, McLean D, Urruticoechea-Uriguen A, et al. Efficient differentiation of hepatocytes from human embryonic stem cells exhibiting markers recapitulating liver development in vivo. Stem Cells 2008;26:894-902.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print





