Cause of death and cause-specific mortality for primary liver cancer in South Korea: A nationwide population-based study in hepatitis B virus-endemic area
Article information
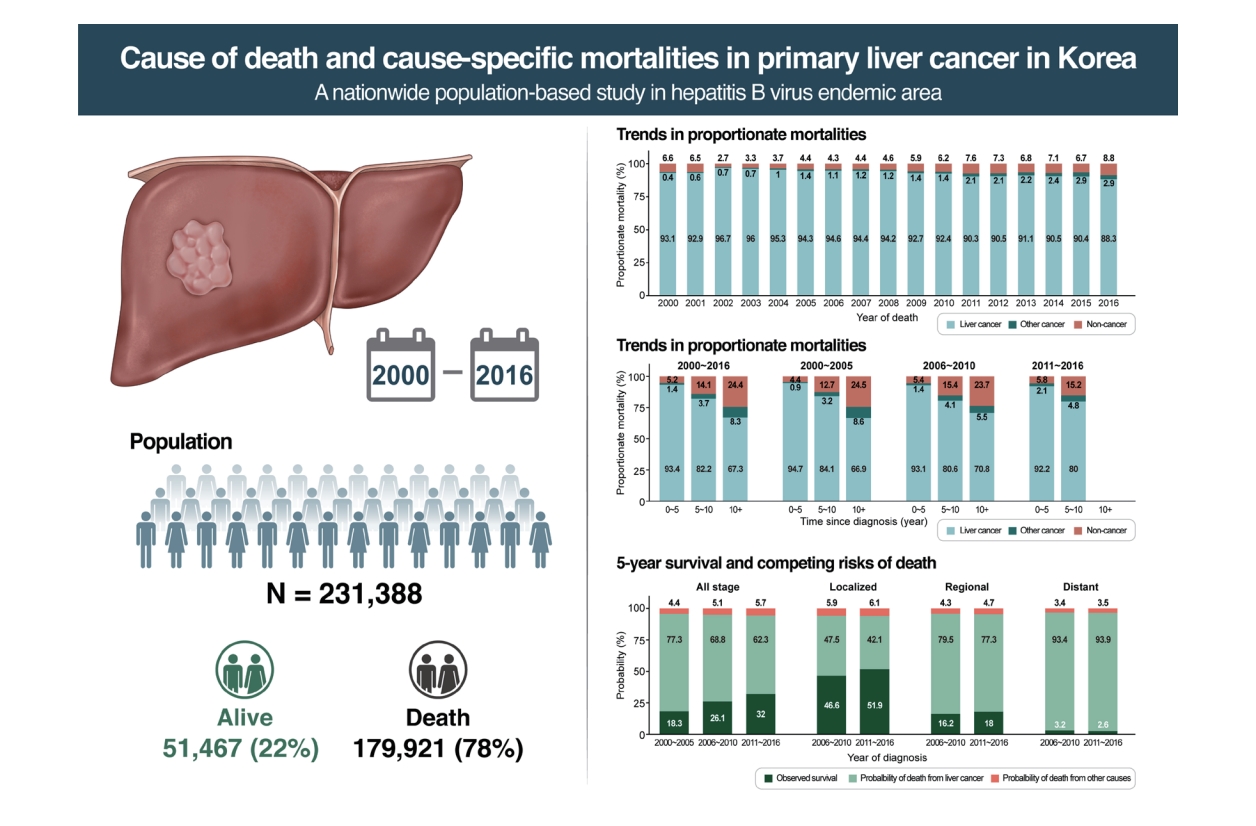
Abstract
Background/Aims
Primary liver cancer is one of the leading causes of cancer mortality worldwide. However, the causes of death have not been studied in detail in patients with liver cancer.
Methods
The causes of death and cause-specific mortality risks in patients with primary liver cancer, diagnosed during 2000–2016, were investigated using the nationwide population-based cancer registry data in South Korea (n=231,388). The cumulative incidence function and Fine-Gray models were used to estimate the cause-specific mortality under the competing risks. Risks of non-cancer deaths relative to the general population were compared by standardized mortality ratios (SMRs).
Results
Among 179,921 total deaths, 92.4%, 1.7%, and 6.0% of patients died of primary liver cancer, cancer from other sites, and non-cancer illnesses, respectively. Proportionate mortality from liver cancer remained high. The 5-year competing risks probability of death from liver cancer varied by tumor stage, from 42% to 94%, and it remained high 10 years after the diagnosis (61–95%). Competing mortality from other causes has continuously increased. The most common non-cancer causes of death were underlying liver diseases (SMR, 15.6; 95% confidence interval [CI], 15.1–16.1) and viral hepatitis (SMR, 46.5; 95% CI, 43.9–49.2), which demonstrated higher mortality risks compared to the Korean general population. Higher mortality risks of suicide (SMR, 2.6; 95% CI, 2.4–2.8) was also noted.
Conclusions
Patients with liver cancer are most likely to die from liver cancer and related liver disease, even 10 years after the diagnosis, highlighting a need for specialized long-term follow-up care.
Graphical Abstract
INTRODUCTION
Cancer is the leading cause of death (COD) worldwide; however, cancer survival rates are improving [1,2]. In the meantime, non-cancer deaths and secondary cancer-related deaths have become common in cancer patients [3]. The mortality risks from non-cancer causes are increasing in patients with prostate, bladder, or breast cancers; however, patients with other types of cancer still have a high probability of death from their cancers [3].
Primary liver cancer is the sixth most commonly diagnosed cancer and the fourth leading cause of cancer mortality worldwide [4]. The highest incidence rates of liver cancer have been observed in Eastern Asia, South-Eastern Asia, and Northern Africa [4]. In South Korea, primary liver cancer is the second most common cause of cancer mortality [1]. Each year, approximately 16,000 patients are diagnosed with primary liver cancer, and 11,000 patients die from primary liver cancer [5]. Absolute number of mortalities or crude death rate from primary liver cancer remained stable throughout the last decade [5].
The overall survival rate of primary liver cancer in Korea has improved over the last two decades. Five-year relative survival among patients with primary liver cancer has increased from 13.2% in patients diagnosed during 1996 through 2000 to 34.0% in patients diagnosed between 2011 and 2015. Despite this improvement, the 5-year survival rate in primary liver cancer patients is still low compared to other cancers such as colorectal, stomach, breast, or thyroid [1]. Moreover, the causes of death have often been studied in patients with breast or prostate cancer as cancer survival has improved [6,7]. In contrast, studies on cause-specific mortality of liver cancer are limited. The present study aimed to investigate the causes of death and cause-specific mortality trends in patients with primary liver cancer.
MATERIALS AND METHODS
The study protocol was approved by the Institutional Review Board of the National Cancer Center (NCC2016-0041).
Data and study population
We obtained data from the Korea Central Cancer Registry (KCCR), a population-based cancer registry linked to mortality statistics. This retrospective cohort database includes patients diagnosed with primary liver and intrahepatic bile duct cancer (C22) between January 1, 2000, and December 31, 2016, and followed until December 31, 2017 (n=231,388). The KCCR is the nationally representative database covering more than 98% of cancer patients in South Korea and contains nationwide cancer incidence and survival data from 1999 onward. The registry is linked to the COD statistics provided by Statistics Korea, the national statistics office of South Korea, which provides an opportunity to study cause-specific mortality [1,8]. Statistics Korea annually collects vital status and COD information from death certificates and classifies the causes of death based on the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10), adapted for Korean data, as recommended by the World Health Organization (WHO) [9,10].
We defined liver and intrahepatic bile duct cancer as the International Classification of Diseases for Oncology (ICD-O; 3rd edition) codes (C220, and C221 excluding 9050-9055, 9140, 9590-9992) and further classified hepatocellular carcinoma (HCC; C220) and intrahepatic cholangiocarcinoma (ICCA; C221). The exclusion criteria for this study were as follows: 1) cases with missing COD information or death certificate only cases, 2) cases with multiple primary tumors, 3) cases lost to follow-up, and 4) patients under 20 years of age at diagnosis. Tumor stage information was available as the Surveillance, Epidemiology, and End Results (SEER) summary stage in the registry, defined as follows: 1) a localized tumor is a malignancy limited to the organ of origin, 2) a regional tumor is a tumor beyond the limits of the organ of origin, and 3) a distant tumor is a tumor that has spread to areas of the body distant or remote from the primary tumor.
COD classification
We used the ICD-10 codes for underlying COD and classified the COD as follows: liver cancer, other causes including cancer at other sites, and non-cancer (i.e., a death attributed to causes other than cancer). To improve the accuracy of cause-specific survival estimation, we applied the cause-specific death classification algorithm [11] to reclassify the COD in patients with cancer to fit Korean liver cancer patients. This algorithm was developed and validated by the United States National Cancer Center Institute’s SEER program to improve the accuracy of COD information in cancer patients by correcting for possible misclassifications [11,12]. The SEER algorithm attributed non-cancer diseases including diseases of the esophagus, stomach, and duodenum (K20-K31), colitis (K51-K52), vascular disorders of the intestine (K55), paralytic ileus and intestinal obstruction without hernia (K56), diverticular disease of the intestine (K57), diseases of the liver (K70-K76), and other diseases of the digestive system (K92) to the cancer of the liver. In our study, deaths from the diseases of the liver (K70-K76) were classified and evaluated separately. To determine the COD rankings among patients with cancer relative to the general population, we used groupings in a list of 56 causes of death. The list was selected from a set of 80 causes of death recommended by the WHO and is officially used by Statistics Korea to illustrate the COD rankings of the South Korean general population [8,10].
Statistical analysis
Descriptive statistics on demographics, tumor characteristics, and proportion of death according to causes were calculated for liver cancer patients. We estimated the trends in proportionate mortalities over the periods studied and stratified the results by the time since cancer diagnosis. Proportionate mortalities were calculated as the proportions of COD among the total number of death. We estimated standardized mortality ratios (SMRs) and 95% confidence intervals (CIs) to compare the mortality risks of non-cancer diseases in liver cancer patients compared to the general population. The 95% CI for the SMR was calculated using the method described by Kahn and Sempos [13]. We computed the observed survival from all causes of death using the Kaplan-Meier estimator. To estimate the probability of death under the presence of competing risks, we used the cumulative incidence function (CIF) for liver cancer death and death from other causes based on cause-specific hazard function [14]. Survival probability and CIF were stratified by tumor stages (localized, regional, and distant), age (20–39, 40–49, 50–59, 60–69, 70–79, ≥80), and year of a cancer diagnosis (2000–2005, 2006–2010, 2011–2016). CIFs were compared using Gray’s test [15]. The competing risks survival analysis was conducted using Fine-Gray models [16] while adjusting for sex, age, stage at diagnosis, and year of diagnosis. Subdistribution hazards ratios were estimated for liver cancer death under the competing risks of death due to other causes. The statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Characteristics of study population
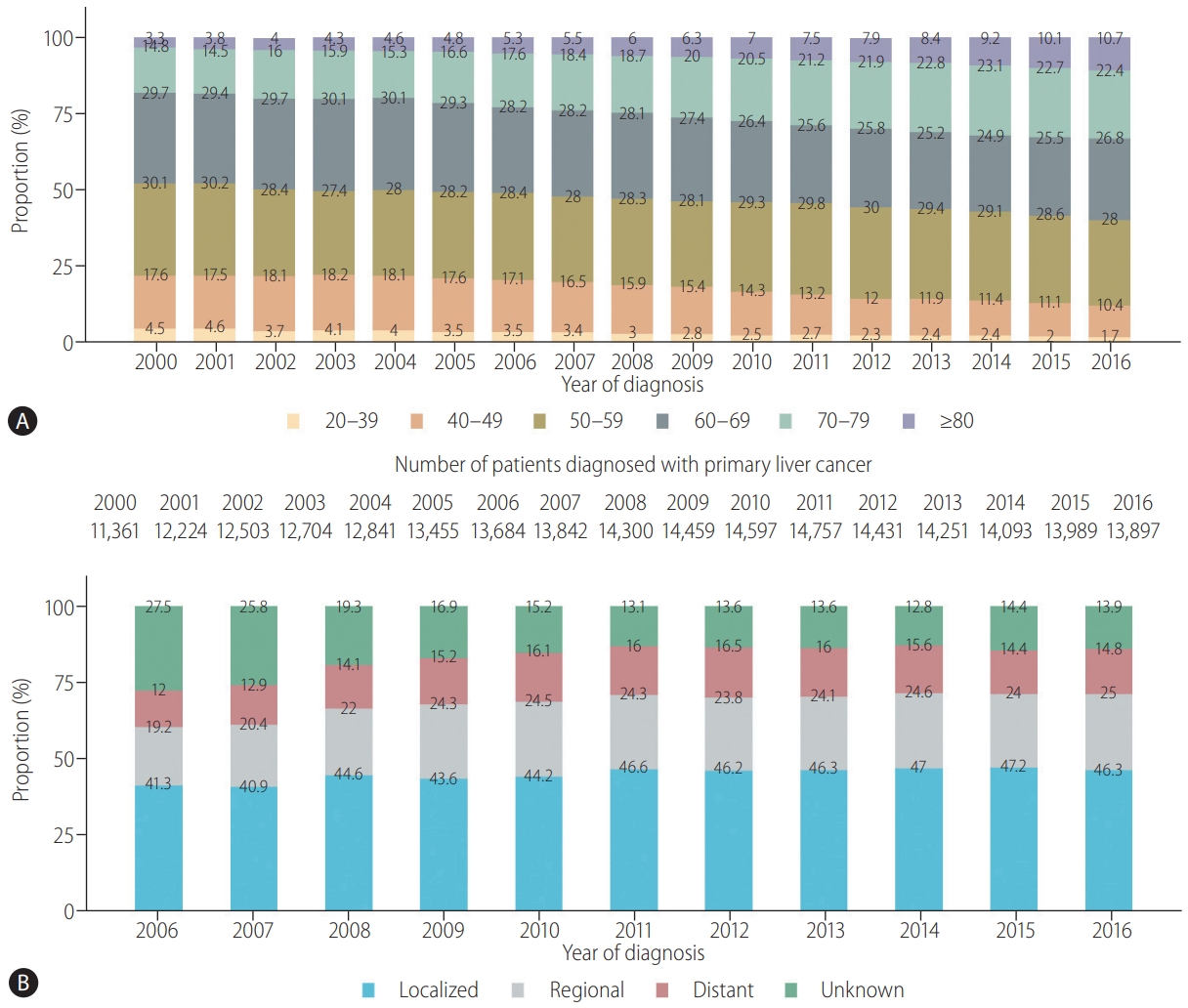
A total of 231,388 patients diagnosed with primary liver cancer between 2000 and 2016 were included in this study (Supplementary Fig. 1). The mean age at diagnosis was 60.9±12.1 years (59.5±11.5 years in males and 65.4±12.5 years in females), and 24.5% were female (Table 1). Of 174,638 male patients, 31.8% and 27.3% were in the 50–59 year and 60–69 year ranges, respectively. Of 56,750 female patients, 28.6% and 27.7% were in the 60–69 year and 70–79 year ranges, respectively. The mean age at death was 63.4±12.3 years (61.7±11.9 years in males and 68.4±12.2 years in females), and it increased from 59.9±12.0 to 66.6±12.4 years from 2000 to 2016 (58.3 to 64.8 years for male patients; 65.2 to 71.8 years for female patients) (Supplementary Table 1). Among our study population, 82.7% of liver cancer patients were diagnosed with HCC (n=191,334), and 17.3% were diagnosed with ICCA (n=40,054). The proportion of ICCA was higher among female patients (27.8%) compared to male patients (13.9%) (Table 1).
The absolute number of patients diagnosed with liver cancer increased from 2000 to 2011 and remained steady (Fig. 1A). However, during the same period, the proportion of elderly patients increased; for example, the proportion of patients aged 70 years or older increased from 18.1% in 2000 to 33.1% in 2016 (Fig. 1A). Among 129,963 patients with available SEER stage information, 30.4%, 15.8%, and 10.1% were localized, regional, and distant stage, respectively (Table 1). The proportion of distant-stage cancers remained primarily unchanged from 2006 to 2016, while the proportion of regional or localized stage cancers increased slightly (Fig. 1B).
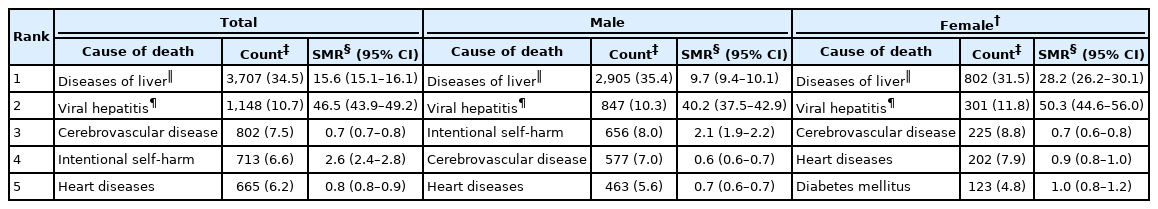
Causes of death and SMR
Of the 231,388 liver patients diagnosed between 2000 and 2016, 78% (n=179,921) died. Among these decedents, 92.4%, 1.7%, and 6.0% died of primary liver cancer, cancer of other sites, and non-cancer, respectively (Table 1). The most common non-cancer causes of death were diseases of the liver (34.5%) and viral hepatitis (10.7%), followed by cerebrovascular disease (7.5%) and intentional self-harm (6.6%) (Table 2). Liver disease and viral hepatitis were common non-cancer causes of death in all age groups. In contrast, intentional self-harm (suicide) was a common non-cancer COD in the younger age (20–59 years old) group, while cardiovascular disease-related death was common in the elderly (60 years old or older) (Supplementary Table 2).
Non-cancer mortality risks compared to the Korean general population matched by age, gender, and calendar year are shown in Table 2. Compared to the Korean general population, mortality risks due to liver diseases and viral hepatitis were significantly higher in patients with liver cancer; for example, the mortality risk was 15.6 times (95% CI, 15.1–16.1) higher in patients with diseases of the liver and 46.5 times higher (95% CI, 43.9–49.2) in viral hepatitis patients. The SMRs were higher in female patients (viral hepatitis: 50.3 in females vs. 40.2 in males; diseases of the liver: 28.2 in females vs. 9.7 in males). Meanwhile, mortality risks due to suicide were 2.6 times higher (95% CI, 2.4–2.8) in liver cancer patients compared to the Korean general population (Table 2).
Trends in cause-specific proportionate mortalities
The absolute number of deaths of patients with liver cancer increased from 2000 to 2012 (Fig. 2A). Proportionate mortality from the diagnosed liver cancer was approximately 90% (mean, 92.8%; range, 88.3–96.7%), and it remained high over the decades. In contrast, the proportion of mortality from causes other than liver cancer increased slightly from 3.4% in 2002 to 11.7% in 2016 (Fig. 2A). This trend was not changed when viral hepatitis and liver disease were recorded as liver cancer death (Supplementary Fig. 2). This observation was noted consistently in all age groups (Supplementary Fig. 3). The proportionate mortality of liver cancer decreased for both tumor types but remained high, at over 89% (Supplementary Fig. 4).

Trends in proportionate mortalities in liver cancer patients, 2000–2016. (A) By the year of death. (B) By time since diagnosis. Percentages are rounded to one decimal place.
During the first 5 years after the diagnosis, 93.4% of patients died from liver cancer; however, the proportion decreased to 67.3% for patients 10 or more years post-diagnosis (Fig. 2B). Non-cancer deaths increased from 5.2% to 24.4% over the corresponding time. Cerebrovascular disease (7.1%) and intentional self-intentional harm (6.9%) were the most common causes among non-cancer deaths during the first 5 years after the diagnosis, apart from liver diseases (37.2%) and viral hepatitis (11.3%) (Supplementary Table 3). At 10 or more years after a cancer diagnosis, cardiovascular disease (10.9%) was the second most common non-cancer COD following liver diseases (19.3%) (Supplementary Table 3).
Cause-specific mortality under the competing risks
The 5-year observed survival rates from all causes of death in liver cancer patients improved from 18.3% in 2000–2005 to 32% in 2011–2016. The survival improvement was notable for patients diagnosed with localized SEER stage (from 46.6% in 2006–2010 to 51.9 % in 2011–2016), while during the same time, survival remained steady for patients diagnosed with the distant stage cancer (3.2% to 2.6%; Fig. 3A). The probability of death due to liver cancer and other causes under the competing risks of death are also shown in Figure 3 and Supplementary Figure 5. The probability of dying from liver cancer decreased significantly for the early stage (P<0.0001) and over the periods of diagnosis (P<0.0001) (Supplementary Fig. 5). The probability of dying from liver cancer in 5 years decreased from 77.3% in patients who were diagnosed in 2000–2005 to 62.3% in patients diagnosed in 2011–2016 (Fig. 3A). For patients diagnosed with localized SEER stage, the probability of death from liver cancer decreased from 47.5% in patients who were diagnosed in 2006–2010 to 42.1% in patients diagnosed in 2011–2016. For patients with regional SEER stage, the probability of death from liver cancer showed a slight decrease from 79.5% to 77.3%; however, for patients with distant SEER stage, the probability of dying from liver cancer in 5 years exceeded 93% and remained stable in the corresponding periods (Fig. 3A). According to the stage at diagnosis, the 5-year probability of death from other competing causes varied from 3.4% to 6.1%; approximately 6% for patients diagnosed with localized stage and less than 4% for patients diagnosed with advanced-stage (Fig. 3A). Meanwhile, the competing risks probabilities of dying from liver cancer and other causes were significantly higher in older patients (Fig. 3B, P<0.0001).

Survival and cause-specific competing risks probability of death, 2000–2016. (A) Five-year all-cause survival and cause-specific competing risks probability of death by tumor stage and year of diagnosis. (B) Competing risks probability of death from liver cancer and other-causes by age at diagnosis. Tumor stage information was available from 2006. The probability of death was estimated by the cumulative incidence function. Percentages are rounded to one decimal place.
The prognosis of patients with HCC was better than that of ICCA patients in the early tumor stage. For instance, the observed 5-year survival was 49.3% for patients diagnosed with localized HCC, compared to 20.6% for patients diagnosed with localized ICCA in 2011–2016 (Supplementary Fig. 6). The 5-year probability of dying from liver cancer was 59.3% among HCC patients, which was lower than the 83.6% among ICCA patients, in 2011–2016 (Supplementary Fig. 6).
The results of multivariable competing risks analysis showed that males with older age and an advanced stage at diagnosis had significantly higher mortality risks under the competing risks (Table 3). For example, patients aged 70–79 years and 80 years or older had 1.48 (95% CI, 1.42–1.55) and 2.27 (95% CI, 2.16–2.39) times higher risk (hazard) of dying from liver cancer death, respectively, compared to patients aged 20–39 years. Patients diagnosed with ICCA had a 1.20 (95% CI, 1.17–1.22) times higher risk of dying compared to HCC patients, and patients diagnosed with distant stage had a 4.45 (95% CI, 4.36–4.54) times higher risk of dying from liver cancer than those diagnosed with localized tumors. Meanwhile, recently diagnosed patients demonstrated decreased mortality risks (hazard ratio, 0.80; 95% CI, 0.79–0.81).
DISCUSSION
The present study demonstrates trends in the COD and cause-specific mortalities in liver cancer patients. The absolute number of deaths among patients with liver cancer increased over time, and liver cancer itself was the most common COD. The proportion of deaths due to liver cancer slightly decreased; however, it remained high at 88% in 2016. The risk of liver cancer death remained high, even 10 or more years after a cancer diagnosis, in liver cancer patients. Liver and viral hepatitis diseases were the most common causes of non-liver cancer deaths. Deaths from cardiovascular and cerebrovascular diseases also became frequent in 10 or more years after a cancer diagnosis.
Liver cancer remains the predominant COD, even though the probability of death from liver cancer has declined over time. The proportionate mortality from other causes of death, including cancer of other sites and non-cancer causes, gradually increased from 3.3% in 2002 to 11.7% in 2016 for patients with liver cancer. Even when liver diseases and viral hepatitis are regarded as liver cancer death, the yearly trend of proportionate mortality demonstrated the increasing tendency of the proportions of death from other non-cancer causes and other causes (Supplementary Fig. 2). However, the degree of increase was small compared to all cancer patients for whom the proportion of other causes of death increased from 5.0% in 2000 to 22.6% in 2016 [17]. These findings imply that the cure rate of liver cancer might still be low compared to other types of cancer. A previous study reported that more than 85% of deaths from diagnosed cancer occurred in patients with stomach, colorectal, lung, or liver cancers within 5 years after the cancer diagnosis [17]. The proportions of diagnosed cancer-related deaths gradually decreased to less than 50% in patients with stomach, colorectal, or lung cancers. In contrast, the proportion of liver cancer death was still high, even 10 years after the diagnosis, in patients with liver cancer. Our results were consistent with the previous findings that the 10-year post-diagnosis proportionate cancer mortality remained high in liver cancer patients, at approximately 67–70%, throughout recent decades. Our study further extends the previous study [17] by evaluating detailed COD exclusively for liver cancer patients and estimating the cause-specific competing risk mortalities. The higher recurrence rate of liver cancer than other types of cancer, such as stomach or colorectal cancers, could contribute to the high proportionate mortality from liver cancer [18]. This finding may warrant periodic follow-up examination after 5 years from the initial cancer diagnosis in patients with liver cancer [19].
Unlike other cancer types, such as stomach, colorectal, or lung cancers, the most common causes of non-cancer deaths for patients with liver cancer was liver disease and viral hepatitis. This finding also supports that most patients with liver cancer have underlying chronic liver disease. In South Korea, which is a hepatitis B virus-endemic area, hepatitis virus B and C account for approximately 70% and 10%, respectively, of HCC [5,20-23]. Antiviral therapy for HBV decreases the risk of decompensation, thereby increasing the life expectancy of patients with HBV-related HCC [24]. Although previous studies have reported that the widespread use of antiviral therapy has contributed to the survival improvement of HBV-related HCC, viral hepatitis is still considered a major cause of non-cancer deaths [24,25].
Other than liver and viral hepatitis, intentional self-harm was the most common cause of non-cancer death among patients aged 20–59 years. The present study demonstrated that suicide ranked high in non-cancer death of young patients with liver cancer, particularly within 5 years after the liver cancer diagnosis, even though older age at diagnosis has previously been reported to be associated with higher suicide rates [26,27]. Previous studies reported a higher risk of suicide among patients with cancer and necessitated psychosocial intervention and prevention strategies [26,27]. Taken together, these findings suggest a need to pay attention to emotional and psychological support for patients with cancer, particularly in the early years of liver cancer diagnosis. Cerebrovascular disease and cardiovascular disease rank high in liver cancer patients aged 60 years or older, as in patients with other types of cancer [17]. Nevertheless, proportions of death from heart disease or cerebrovascular disease are relatively small, and the mortality risks are lower compared to those of the Korean general population with low SMRs (heart diseases: SMR, 0.8; 95% CI, 0.8–0.9; cerebrovascular diseases: SMR, 0.7; 95% CI, 0.7–0.8). This result is compatible with previous studies which reported that Korean cancer patients showed low SMRs (<1.0) for heart and cerebrovascular diseases [17]. Interestingly, cancer patients in the Western countries had high SMRs for cardiovascular disease and cerebrovascular disease, probably reflecting the different disease risks and prevalence between countries [3,28]. Nevertheless, the trend in South Korea would also change, expecting higher risks, as proportions of patients with nonalcoholic fatty liver disease increase [29,30].
A major strength of our study was that it was a large population-based study investigating the cause-specific mortality trends and competing causes of death in liver cancer patients. The comprehensive patterns in the causes of death and trends in competing mortality risks, including the competing risks modeling approach, in patients with liver cancer have not been investigated in depth, to the best of our knowledge. However, the present study also had several limitations. First, we could not incorporate detailed individual-level etiological and prognostic factors in the analyses. The available information was limited since the cancer registry data does not include information regarding the cause of cancer, liver function, hepatitis virus infection status, antiviral treatment received, performance status, recurrence of cancer, or response to cancer treatment. A comprehensive multivariate study incorporating the risk factors for liver cancer mortality and the associated individual patient level competing risks analysis should be performed in the future. Second, misclassification of the COD based on death certificates might exist, which could have led to underestimating deaths from non-cancer death. It is challenging to distinguish liver cancer-related death from death due to underlying liver disease in real-world practice. Many of the patients with liver cancer have underlying chronic liver disease. It might have been challenging to assign a COD as progressive liver disease (diseases of liver or viral hepatitis) or progressive liver cancer, since the two are closely associated with each other. Also, the COD might have been assumed to be liver cancer once the patients were diagnosed with liver cancer. The KCCR registry data does not include detailed information on each patient’s death. Therefore, we used the information on the COD from the death certificate obtained from Statistics Korea, where the official COD statistics is reported annually in South Korea [10]. In Korea, physicians certify the COD and issue the death certificate, and Statistics Korea has been making ongoing efforts to improve accuracy in collecting data related to the COD. We further applied the SEER cause-specific death classification algorithm to enhance the accuracy of COD classifications in cancer patients.
In summary, our results showed that patients with liver cancer were most likely to die from liver cancer itself, even 10 years after the cancer diagnosis. The proportion of mortality from causes other than liver cancer tended to increase slightly; however, the magnitude of the increase was small. The most common non-cancer causes of death were liver diseases and viral hepatitis. These findings highlight the need for specialized, continued long-term follow-up care for patients with liver cancer.
Notes
Authors’ contributions
Conception and study design: BHK, HC; Investigation and data curation: DL, KWJ, YJW, HC; Methodology and formal analysis: BHK, DL, HC; Interpretation of results: BHK, DL, HC; Writing – original draft: BHK, HC; Writing-review and editing: DL, KWJ, YJW. All authors reviewed and approved the final draft.
Conflicts of Interest
BHK has served in an advisory role for Eisai and Roche; received honoraria from Abbvie; and participated in research sponsored by Ono-BMS and Hanmi. The other authors have no conflicts to disclose.
Acknowledgements
This study was supported by the National Cancer Center, Korea (grant number: NCC-1710300-3, NCC-2110450, and NCC2010162). The funding source had no role in the study design, data curation, or the analysis and interpretation of data.
The authors thank the staff of the Korea Central Cancer Registry and Statistics Korea.
Data that support this study’s findings can be requested from the Korea Central Cancer Registry (https://ncc.re.kr/main.ncc?uri=manage02_4) and Statistics Korea (https://mdis.kostat.go.kr/index.do). The data are not publicly available due to privacy or ethical restrictions.
SUPPLEMENTAL MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website (http://www.e-cmh.org).
Patient selection. KCCR, Korea central cancer registry; DCO, death certificate only.
Trends in proportionate mortality, 2000–2016. Percentages are rounded to one decimal place.
Trends in proportionate mortality by age group, 2000–2016. Percentages are rounded to one decimal place.
Trends in proportionate mortalities in liver cancer patients with hepatocellular carcinoma and intrahepatic cholangiocarcinoma, 2000–2016. (A) Hepatocellular carcinoma. (B) Intrahepatic cholangiocarcinoma. –, less than 10 cases. Percentages are rounded to one decimal place.
Competing risks probabilities of death from liver cancer and other causes by tumor stage and period of diagnosis. (A) By tumor stage, 2006–2016. (B) By period of diagnosis, 2000–2016. Tumor stage information was available from 2006. The probability of death was estimated by the cumulative incidence function.
Five-year survival and cause-specific competing risks probability of death of patients with hepatocellular carcinoma and intrahepatic cholangiocarcinoma, 2000–2016. (A) Hepatocellular carcinoma. (B) Intrahepatic cholangiocarcinoma. Tumor stage information was available from 2006. The probability of death was estimated by the cumulative incidence function. Percentages are rounded to one decimal place.
Mean and standard deviation of age at death by sex, year of death, and cause of death
Distribution of non-cancer cause of death by age group
Distribution of non-cancer cause of death in liver cancer patients by time since cancer diagnosis
Abbreviations
CIF
cumulative incidence function
CIs
confidence intervals
COD
cause of death
HCC
hepatocellular carcinoma
ICCA
intrahepatic cholangiocarcinoma
ICD-10
International Statistical Classification of Diseases and Related Health Problems
ICD-O
International Classification of Diseases for Oncology
KCCR
Korea central cancer registry
SEER
Surveillance
SMRs
standardized mortality ratios
WHO
World Health Organization
References
Article information Continued
Notes
Study Highlights
The present nationwide study reported that liver cancer and related liver diseases remain the most prevalent causes of death among liver cancer patients, despite the progress in liver cancer control. Long-term follow-up care is necessary, considering the high risk of liver cancer death even 10 years after the diagnosis.