| Clin Mol Hepatol > Volume 28(4); 2022 > Article |
|
Dear Editor,
We read with great interest the a recent large-scale cohort study by Jeong et al. [1], which suggested that non-alcoholic fatty liver disease (NAFLD) was associated with a higher risk for incident dementia (adjusted hazard ratio, 1.05; 95% confidence interval [CI], 1.02â1.08; P=0.001), and was in agreement with another previous study [2]. However, we found that other studies have reported results that contradict the findings of the above studies [3-5]. Therefore, we performed a metaanalysis of cohort studies to investigate the association between NAFLD and the risk for dementia. Since the prevalence of NAFLD has increased significantly in recent years [6], it is critical to investigate any potential association with dementia.
Two authors independently searched PubMed and Embase records up to August 2022. âNon-alcoholic Fatty Liver Diseaseâ and âDementiaâ were searched for MeSH terms and free-text searches without language limitations. We included cohort studies reporting the association between NAFLD and dementia incidence, with data provided as hazard ratios and 95% CIs. The Newcastle-Ottawa scale for cohort studies was used to assess the quality of included studies. Two authors independently performed data extraction and quality assessment. Any conflicts were resolved by discussion or by consulting the third author. Of the 1,136 relevant published studies, 1,130 were excluded because they were not original studies (n=643), did not meet the inclusion criteria (n=311), or were duplicates (n=176). Eventually, six cohort studies, including the Jeong et al. [1] study, and other studies [3-5,7,8] were eligible. A total of 2,345,929 patients, with a mean age of 48.2â73.4 years, were included in the meta-analysis.
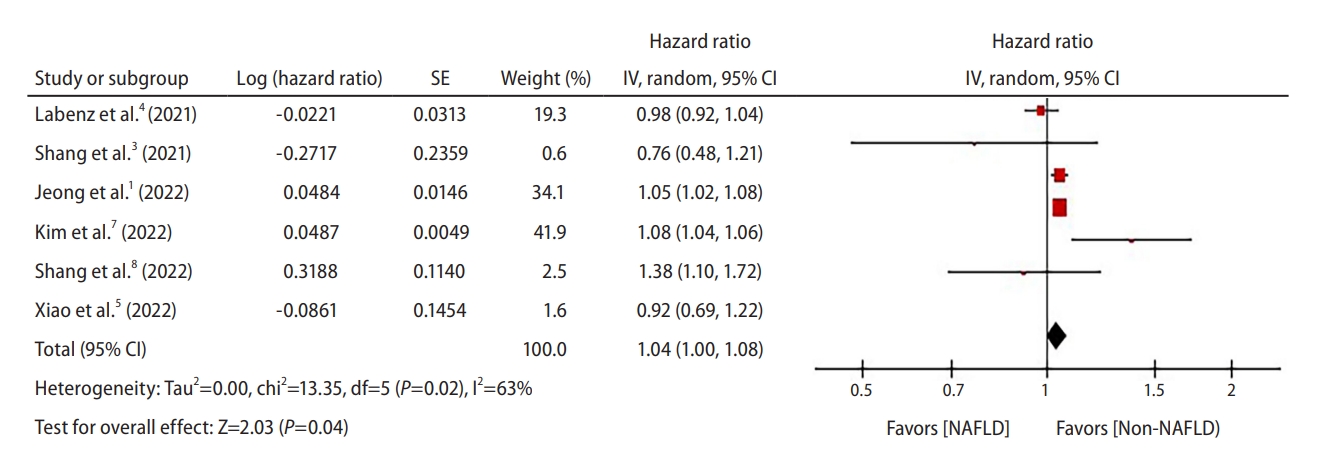
The RevMan 5.4 software (The Cochrane Collaboration, London, UK) was used to perform the meta-analysis and the I2 test was used to test heterogeneity. A random-effect model was used for the analysis. The pooled hazard ratio from six cohorts was 1.04 (95% CI, 1.00â1.08; P=0.04, I2=63%) (Fig. 1). Heterogeneity was high with an I2 of 63%. Sensitivity analyses were performed to assess the robustness of the meta-analysis. Each study was sequentially excluded for sensitivity analysis. The analysis showed that a few large studies affected the significance of the results [1,7]. However, a relationship between NAFLD and dementia was generally demonstrable. Further subgroup analyses are required to explore the causes of heterogeneity.
To the best of our knowledge, this was the first meta-analysis for the association between NAFLD and the risk for dementia. This meta-analysis indicated that NAFLD was a significant risk factor for dementia. However, due to the heterogeneity of statistical analyses, the results must be interpreted cautiously. Further prospective studies are needed to establish the relationship between NAFLD and dementia. Influence of other factors, including age, sex, ethnicity, and diagnosis, also requires further investigation.
FOOTNOTES
REFERENCES
1. Jeong S, Oh YH, Choi S, Chang J, Kim SM, Son JS, et al. Association of non-alcoholic fatty liver disease with incident dementia later in life among elder adults. Clin Mol Hepatol 2022;28:510-521.




2. Wang Y, Li Y, Liu K, Han X, Dong Y, Wang X, et al. Nonalcoholic fatty liver disease, serum cytokines, and dementia among rural-dwelling older adults in China: a population-based study. Eur J Neurol 2022;29:2612-2621.



3. Shang Y, Nasr P, Ekstedt M, Widman L, StĂĽl P, Hultcrantz R, et al. Non-alcoholic fatty liver disease does not increase dementia risk although histology data might improve risk prediction. JHEP Rep 2021;3:100218.



4. Labenz C, Kostev K, Kaps L, Galle PR, Schattenberg JM. Incident dementia in elderly patients with nonalcoholic fatty liver disease in Germany. Dig Dis Sci 2021;66:3179-3185.




5. Xiao T, van Kleef L, Ikram MK, De Knegt R, Ikram MA. Association of nonalcoholic fatty liver disease and fibrosis with incident dementia and cognition: the Rotterdam study. Neurology 2022;99:e565-e573.



6. Park SH, Plank LD, Suk KT, Park YE, Lee J, Choi JH, et al. Trends in the prevalence of chronic liver disease in the Korean adult population, 1998-2017. Clin Mol Hepatol 2020;26:209-215.




- TOOLS
-
METRICS

- ORCID iDs
-
Cheng-Hsien Hung

https://orcid.org/0000-0001-8685-3925 - Related articles
-
Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?2023 October;29(4)
Nonalcoholic fatty liver disease and non-liver comorbidities2023 February;29(Suppl)
Non-alcoholic fatty liver disease: Definition and subtypes2023 February;29(suppl)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



