2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
Article information
Abstract
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide and the fourth most common cancer among men in South Korea, where the prevalence of chronic hepatitis B infection is high in middle and old age. The current practice guidelines will provide useful and sensible advice for the clinical management of patients with HCC. A total of 49 experts in the fields of hepatology, oncology, surgery, radiology, and radiation oncology from the Korean Liver Cancer Association-National Cancer Center Korea Practice Guideline Revision Committee revised the 2018 Korean guidelines and developed new recommendations that integrate the most up-to-date research findings and expert opinions. These guidelines provide useful information and direction for all clinicians, trainees, and researchers in the diagnosis and treatment of HCC.
INTRODUCTION
Intent of revision
The Korean Liver Cancer Study Group (KLCSG)-National Cancer Center (NCC) Korea practice guidelines for the management of hepatocellular carcinoma (HCC) were first announced in 2003 and have been revised three times; first in 2009, second in 2014, and then in 2018. Since then, an abundance of new research findings and therapies for HCC have been presented and published in South Korea and around the globe. As many studies have been conducted, a substantial amount of knowledge have been accumulated on the diagnosis, staging, and treatment of HCC specific to Asia, with the study results showing different clinical behaviors from the West, especially in South Korea; these new research findings have provided clinicians with various action plans and measures related to HCC. Accordingly, in the summer of 2021, the Korean Liver Cancer Association (KLCA, formerly KLCSG)-NCC Korea Practice Guideline Revision Committee (KPGRC) initiated the revision of the guidelines to develop a new recommendation plan that integrates the most up-to-date research findings and expert opinions after the release of the 2018 guidelines.
Target population
The primary targets of these new guidelines are patients with suspicious or newly diagnosed HCC. The key to treatment according to these guidelines is the initial treatment of patients with newly diagnosed HCC; however, for the first time, we extensively reviewed and discussed residual, progressive, or recurrent cancer after initial treatment and provided relevant recommendations since the 2018 guidelines. Moreover, these guidelines can be applied more usefully in actual clinical practice as it described the prevention methods, surveillance tests, a treatment overview, preventive antiviral treatment of underlying chronic hepatitis, management of cancer pain, and an assessment of the tumor response after treatment.
Intended users
These guidelines are intended to provide useful clinical information and direction for all clinicians in charge of the diagnosis and treatment of HCC in South Korea and other countries with similar conditions. They are also intended to provide specific and practical information for medical residents in training, specialists, and their instructors.
Developers and funding source
The KLCA-NCC KPGRC, organized by the consensus of the KLCA and NCC, consists of hepatologists, oncologists, surgeons, radiologists, and radiation oncologists. All required funding was provided by the NCC (#1731510-1). Each member of the KPGRC collected, analyzed relevant evidence, and wrote the manuscript. Conflicts of interests among the members are summarized in Appendix 1.
Literature search for evidence collection
The 2022 KPGRC (Appendix 2) collected and analyzed the Korean and international literature published on HCC since the announcement of the 2018 guidelines through a PubMed search for revision of the guidelines based on the latest updated evidence. Only English and Korean literature were searched, and the keywords included HCC and other keywords specific to related sub-topics. The sub-topics encompassed a wide range of clinically important items, such as epidemiology, prevention, diagnosis, staging, treatment, and response assessment of HCC.
Literature collected for evidence was analyzed through systematic review, and levels of evidence were classified by the revised Grading of Recommendations, Assessment, Development and Evaluation (GRADE) (Table 1) [1-4]. The levels of evidence were categorized based on the possibility of changes in the assessment through further research and were defined as follows: high (A), with lowest possibility; moderate (B), with certain possibility; and low (C), with highest possibility. For example, level A evidence is similar but not identical to that from one or more randomized controlled trials (RCTs). When there is no possibility of a change in the level of evidence since further RCTs are unlikely to be conducted, such evidence could be considered level A. In contrast, RCTs that have a small population of target patients and need further research or have been published only in abstracts were regarded as a lower level evidence. The GRADE system was implemented for classifying the grades of recommendation as strong (1) and weak (2) collectively, considering not only the level of evidence but also the quality, patient benefit-risk, and socioeconomic aspects of each study. Therefore, each recommendation was graded based on the level of evidence (A–C) and grade of recommendation (1 or 2) as follows: A1, A2, B1, B2, C1, or C2 (Table 1). These guidelines avoided giving C2 grades as much as possible. For the first time, the D-grade recommendation was described as the opinions of experts only.
List of clinical questions
The KPGRC selected sub-topics and clinical questions from four departments regarding the revision of the guidelines (Appendix 3), reviewed the evidence of each item, and suggested recommendations through discussion with each subcommittee (Table 2).
Manuscript review
Recommendation drafts were made through several intradepartmental meetings after the initial meeting of the KPGRC and two interdepartmental meetings attended by all members of the committee. The drafts were then thoroughly reviewed through several online discussions and three department head meetings. In addition to the integrity of the contents, methodological validity of the manuscript was also evaluated on the basis of the Appraisal of Guidelines for Research and Evaluation II [5,6]. The complete draft was then reviewed by the advisory board and through a public meeting, and was modified further at the KPGRC department head meeting. The advisory board consisted of nine clinical specialists in liver cancer. The guidelines made through this process were endorsed by the open meeting, board of directors of the KLCA, and the NCC (Appendix 4).
Release of guidelines
The revised guidelines were presented at the 16th conference of the KLCA on June 24, 2022 (Appendix 5). The Korean version is available at the KLCA and NCC websites (http://livercancer.or.kr; http://ncc.re.kr).
Plan for updates
The KLCA and NCC Korea will update part or all of these guidelines when new test methods, drugs, or treatments regarding HCC are developed and new significant research findings are made, and thus, the revision of the guidelines is deemed necessary for promoting the national health of Korea. The schedule for this plan will be posted as needed.
EPIDEMIOLOGY
Metrics of disease burden from liver cancer (mortality vs. incidence, crude rate vs. age-standardized rate)
The disease burden of cancer is commonly described as the incidence or cause-specific mortality. Of these, cause-specific mortality is the most important and standard measure in assessing the disease burden of cancer. Mortality due to a specific disease is useful for determining priorities in public healthcare policies and research. The latest data on disease-specific mortalities are used to determine whether current healthcare policies and research can effectively reduce the burden of a disease and whether new measures must be taken [7,8].
Mortality and incidence are reported as crude rates and age-standardized rates. Cancer mortality in South Korea is reported with both crude and age-standardized rates (revised by the resident registration data in 2005), and the incidence of cancer is reported with crude rates based on the Korean Central Cancer Registry (KCCR) and age-standardized rates (revised by the resident registration data in 2000). It has been reported that age-standardized rates do not differ significantly according to which population they are adjusted for. However, age-standardized rates must be carefully interpreted, as they sometimes differ from crude rates (Fig. 1), especially more so if the population is rapidly aging, as is the case in South Korea. The United States Centers for Disease Control and Prevention (CDC) recommends choosing between crude rates and age-standardized rates depending on the purpose of use (https://www.cdc.gov/cancer/npcr). It is recommended to use crude rates for estimating the magnitude of resources needed to overcome the social burden of the disease and the disease itself. Age-standardized rates are recommended for determining whether the difference between countries, regions, or time periods are attributable to the age distribution within different population groups.
Given this background, the current guideline considers crude death rate as the most important indicator of the disease burden of liver cancer. This guideline additionally considers crude incidence rate, age-standardized death rate, and age-standardized incidence rate as supplementary indicators.
Liver cancer mortality and economic burden
Malignant neoplasm (cancer) is the main cause of death among South Koreans. According to Statistics Korea (KOSTAT), cancer was the number one cause of death in 2020, with cancer mortality reported as 160.1 persons per 100,000 population. This was 2.5 times higher than that of cardiac diseases, the second most common cause of death, which had a mortality of 63.0 persons per 100,000 population. Liver cancer was the second most common cause of cancer-related death in 2020, with a mortality of 20.6 persons per 100,000 population, following lung cancer with a mortality of 36.4 persons per 100,000 population. However, liver cancer was the number one cause of death among people aged 40–59 years, the most economically productive age group, and the second and fourth highest cause of death among men (30.5 persons per 100,000) and women (10.7 persons per 100,000), respectively (2020 Cause of Death Statistics, Statistics Korea https://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=403046).
In 2015, the yearly economic burden caused by liver cancer in South Korea was 2,266,100,000 USD (approximately 2.7 trillion Korean Won), the highest among all types of cancer. It also showed a steady increase from 2,065,000,000 USD (approximately 2.3 trillion Korean Won) reported in 2000 [9,10]. In other words, liver cancer has the highest disease burden among all types of cancer in South Korea.
Trends in liver cancer mortality and incidence
The yearly crude death rate of liver cancer began to plateau in the last 5 years, after having shown a consistent increase in the previous years. The yearly crude death rate of liver cancer (in unit of deaths per 100,000 population) drastically increased from 16.2 in 1984 to 20.5 in 1999 and 22.5 in 2010, plateaued after 2015, and then settled at 20.6 in 2019 and 2020 (Fig. 1). The yearly absolute number of deaths has also increased over the last two decades; it increased by 19.4% from 9,682 in 1999 to 11.566 in 2014, and then decreased by 8.6% to 10,565 in 2020 (Fig. 2). The yearly crude incidence rate of liver cancer has also increased over the last two decades; it consistently increased from 28.1 in 1999 to its peak at 32.8 in 2010 and 31–32 in 2015, and has been maintained at 30.4 since 2019.
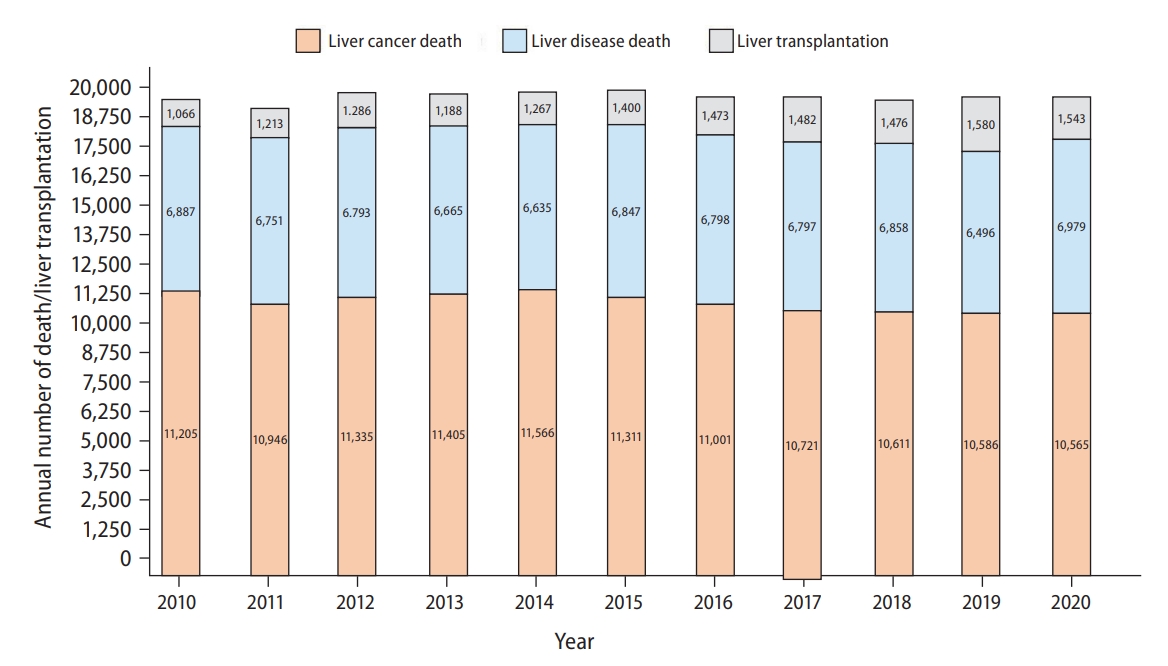
Annual number of liver cancer deaths, liver disease deaths and liver transplantations in South Korea during calendar years 2010 to 2020.
In contrast to the yearly crude death and incidence rates of liver cancer, which started to plateau recently after having consistently increased in the last two decades, the yearly age-standardized death and incidence rates of liver cancer have decreased. The age-standardized death rate of liver cancer significantly decreased from 24.7 in 1999 to 16.4 in 2014 and 11.5 in 2020. The age-standardized incidence of liver cancer also significantly decreased from 28.9 in 1999 to 19.7 in 2014 and 16.1 in 2019 (Korea Central Cancer Registry. Annual Report of Cancer Statistics in South Korea (2018), Ministry of Health and Welfare, 2021) [11]. The different trends between the crude and age-standardized rates on the yearly death and incidence rates of liver cancer can be attributed to the rapid aging of the Korean population, including the patients with liver cancer. The general elderly population aged ≥65 years increased from 3,394,896 in 2000 (7.2% of the total population) to 8,571,347 in 2021 (16.5% of the total population), contributing to a considerable increase in the mean age of the total population and the proportion of the elderly (2021 Elderly Statistics, Statistics Korea). There was a greater increase in age among liver cancer patients compared to the general population, making it appear as if the age-standardized rates have decreased significantly.
Summary
To summarize, although liver cancer has the second-highest crude death rate across all age groups, it ranks first among the working-age group and causes the highest economic burden among all types of cancer. Although the age-standardized death and incidence rates of liver cancer appear to have decreased, this is not due to an actual decrease in the disease burden of liver cancer but due to the rapid aging of the general population. In addition, the crude death and incidence rates of liver cancer are not decreasing but rather have remained constant in recent years, suggesting that liver cancer requires the most urgent attention among all types of cancer in South Korea.
PREVENTION
Causes and prevention of HCC
HCC occurs almost exclusively in patients with risk factors, such as chronic hepatitis B, chronic hepatitis C, or liver cirrhosis. The most important cause of HCC in South Korea is chronic hepatitis B virus (HBV) infection. According to the results of a random selection registry study of the KLCA and the KCCR, 59.1% of patients diagnosed with HCC between 2012 and 2014 were infected with HBV and 10.7% with hepatitis C virus (HCV). Unknown causes accounted for the remaining 30.3% [12]. It is presumed that liver cirrhosis caused by alcoholic and/or nonalcoholic fatty liver disease would be the main underlying disease for the unknown causes. A cohort study from a single center (2010–2015) reported that 74.0% of patients diagnosed with HCC were with HBV infection [13]. Since about 90% of patients with HCC have cirrhosis or chronic hepatitis B at diagnosis, it is difficult to perform radical treatment, and the risk of recurrence continues even 5 or 10 years after treatment, which worsens the overall prognosis of the patients. According to the National Cancer Registry released by the KCCR in 2017, the 5-year survival rate of patients with HCC was 33.6% and the 10-year survival rate was as low as 20% [14]. These data suggest that preventive measures against HCC are of the utmost importance.
Primary prevention of HCC is to prevent the risk of HCC through measures such as vaccination against HBV and abstinence from alcohol consumption. Secondary prevention is to reduce the risk of developing HCC in patients who already have a risk of HCC, using measures such as antiviral treatment for HBV and HCV to prevent the progression of chronic inflammation and fibrosis of the liver. Tertiary prevention is to prevent the development of new HCC in the remaining liver after curative treatment in patients who have already developed HCC [15].
Primary prevention of HCC
The most important preventive measure for HCC in South Korea is the universal neonatal vaccination against HBV, since most HBV infections are caused by vertical transmission of the virus from mother to child in the neonatal period [16]. Since the majority of HBV infection cases worldwide were reported as mother-to-child transmission during the neonatal period, HBV vaccination should be given as early as possible within 24 hours after birth. The World Health Organization (WHO) recommends HBV vaccination for all newborns regardless of maternal HBV status [17]. In South Korea, the prevalence of chronic hepatitis B infection is about 3–4%, with a high risk of transmission even in adults. Therefore, adults who do not have antibodies to the HBV surface antigen (HBsAg) and have never been exposed to the virus (negative for all HBsAg, HBV surface antibody [anti-HBs], and immunoglobulin (Ig) G HBV core antibody [anti-HBc]) should be vaccinated against HBV [18,19]. In particular, people at high risk of HBV infection (family members of chronic hepatitis B patients, healthcare workers, travelers traveling to areas with high HBV prevalence, persons who inject drugs, and people with multiple sexual partners, etc.) should also be vaccinated against HBV.
No vaccine has yet been developed to prevent HCV infection. Since HCV is transmitted almost entirely through contaminated blood, infection must be prevented by avoiding unsanitary invasive procedures (such as multiple use of acupuncture needles, capping, tattooing, or needle sharing).
Excessive alcohol intake over an extended period of time is an independent cause of liver cirrhosis and HCC, and can further increase the risk of liver cirrhosis and HCC in patients with preexisting chronic liver disease. In South Korea, alcoholic liver cirrhosis is one of the leading causes of HCC, together with chronic hepatitis B and C. Therefore, efforts should be made to lower the risk of developing HCC by limiting excessive alcohol consumption. A systematic review with meta-analysis has shown that continuous consumption of even a relatively low level of alcohol (≥1 drink/day for female, ≥2 drinks/day for male) increases the risk of developing HCC [20].
Metabolic syndrome and fatty liver disease are associated with obesity and diabetes mellitus, and are also known to increase the incidence of HCC [21-23]. Therefore, efforts to reduce obesity and metabolic syndrome are necessary to prevent the development of HCC. Statins for treating hyperlipidemia have been extensively studied for an association with the reduction of HCC risk. Large-scale meta-analyses involving earlier studies have reported that statin use was associated with a reduction in the incidence of HCC by 37% [24]; however, in the RCTs that were included in the meta-analyses, a reduction of HCC incidence was not shown with statin therapy. It is of note that this finding was derived from post-hoc analysis of the RCTs, of which the primary outcome focused on the effect of statins on cardiovascular mortality. Moreover, the study subjects included in the RCTs were at a low risk for developing HCC and not regularly monitored under surveillance program for HCC; therefore, the negative results from RCTs should be interpreted with caution. Recent prospective studies involving large European population-based cohorts revealed that statins had a higher chemopreventive effect on HCC occurrence [25,26]. Studies of Korean public database as well as a hospital-based cohort of Korean patients with chronic hepatitis B also reported that statins were associated with a lower risk for HCC [27,28]. Recent meta-analyses of large-scale cohort studies also showed a significant reduction in the risk of HCC (relative risk [RR], 0.54; hazard ratio [HR], 0.57) with statin use [29,30]. Based on the published data, the potential hepatotoxicity or myopathy of statins was not a cause for concern (less than 3% of all patients taking statins) [29]. However, caution is still required as the long-term safety of statins has not been well-documented in patients with cirrhosis [31]. Another study reported that along with statins, metformin reduced HCC development in type 2 diabetes [32], and this should be further confirmed through additional studies.
Aspirin and other antiplatelet agents have also been suggested to reduce the risk of developing HCC in large prospective population-based observational studies [33,34]. A Swedish study of nationwide patient registries observing 50,275 patients with HBV or HCV for 7.9 years reported that treatment with low-dose aspirin (<160 mg/day) was associated with a significantly reduced risk of HCC (adjusted HR [aHR], 0.69; 95% confidence interval [CI], 0.62–0.76) [35]. In the study, it was noted that the preventive effects of aspirin on HCC incidence appeared to be treatment duration-dependent. A retrospective cohort study involving Korean patients with chronic hepatitis B on antiviral therapy showed similar results regarding the beneficial effects of aspirin on HCC [36]. Recent meta-analyses of population-based cohorts or at-risk patients with chronic liver disease revealed that aspirin was associated with a significantly decreased risk of HCC development (HR, 0.51–0.59; RR, 0.73) [37-39]. However, aspirin use was reported to slightly increase the risk (RR, 1.15–1.32) of gastrointestinal bleeding as a major adverse event [37,38]; therefore, the potential benefits from aspirin must be weighed against the potential for bleeding in patients with chronic liver disease. Particularly, the benefits from aspirin use regarding lowering HCC risk were reportedly lacking (aHR, 1.00; 95% CI, 0.85–1.18) in patients with HBV-related cirrhosis in a recent analysis of Korean population-based administrative database [40]. Thus, the use of aspirin or anti-platelet agents for the prevention of HCC is not uniformly recommended in routine practice for managing patients with cirrhosis. The optimal dose and duration of aspirin effective for preventing HCC occurrence are yet to be determined, and the chemopreventive effect of other nonsteroidal anti-inflammatory drugs (NSAIDs), excluding aspirin, on HCC also remains uncertain.
Coffee is the only food or drink that has shown evidence for reducing the risk of HCC occurrence. In recent meta-analyses and large-scale cohort studies, coffee consumption significantly reduced the risk of HCC, regardless of the consumption amount, as well as the severity and cause of underlying liver disease [41-44]. In most studies, the reported amount of coffee consumed per day was more than 2–3 cups or more, or was not clearly described.
Secondary prevention of HCC
Continued high-level viremia in patients with chronic hepatitis B or C is an independent risk factor for the development of HCC. Therefore, the inhibition of HBV or HCV proliferation by antiviral therapy is expected to reduce the incidence of HCC. Regarding the antiviral therapy of chronic hepatitis B and chronic hepatitis C, we recommend following the clinical practice guidelines of the Korean Association for the Study of Liver (KASL) [45,46].
Oral antiviral agents, such as tenofovir and entecavir, are preferred as the first-line treatment for chronic HBV infection. There is no RCT to determine whether interferon therapy reduces the incidence of HCC in chronic hepatitis B patients. Lamivudine, the first oral antiviral agent for patients with chronic hepatitis B, has shown to reduce the incidence of HCC in patients with advanced hepatic fibrosis in a RCT (32 months of follow-up: lamivudine vs. control, 3.9% vs 7.4%; P=0.047) [47]. Large-scale observational studies have consistently shown that long-term therapy with entecavir and tenofovir, potent antiviral agents that have a strong inhibitory effect on HBV proliferation, significantly reduces the incidence of HCC compared with the untreated control group [48-50].
Recently, a number of active studies have been performed to compare the difference in HCC prevention between antiviral drugs for chronic hepatitis B, particularly in South Korea. The first study analyzed the National Health Insurance Service database of 24,156 patients and in-hospital cohort of 2,701 Korean patients with chronic hepatitis B and showed that tenofovir significantly decreased the risk of HCC occurrence by 32% compared to entecavir [51]. However, other two large cohort studies, involving 2,897 and 3,022 Korean patients, revealed no difference in the incidence of HCC between groups on tenofovir and entecavir therapy [52,53]. Another Korean study including the largest cohort of 55,473 patients with chronic hepatitis B showed no difference in the occurrence of HCC in the entire cohort, but a lower incidence of HCC among patients on tenofovir than those on entecavir in the subgroup analysis of patients enrolled between 2012 and 2014 [54]. According to reports from Asian as well as Western countries, there have been huge controversies regarding the chemopreventive effects between tenofovir and entecavir on the development of HCC, mostly showing the superior preventive effects with tenofovir than with entecavir, or no difference between the two drugs. The results of a systematic literature review or meta-analysis also showed conflicting results. In a meta-analysis of 14 relevant studies, there was no difference between the two drugs in the overall HCC risk (RR, 1.28; 95% CI, 0.99–1.66), and the analysis of seven studies that adjusted for clinical variables reported a reduction in HCC risk among patients treated with tenofovir compared to those treated with entecavir (95% CI, 1.01–1.60, P=0.04) [55]. In another meta-analysis including a total of 119,053 patients from 31 studies, no difference in the occurrence of HCC was observed between patients treated with tenofovir and entecavir, in both the propensity score-matching analysis (5-year HCC incidence of 3.44% for entecavir vs. 3.39% for tenofovir) and the analysis after adjustment for clinical variables (aHR, 0.88; 95% CI, 0.73−1.07) [56]. On the other hand, several retrospective studies that evaluated the chemopreventive effects of tenofovir tenofovir alafenamide (TAF), which improved the side effects of tenofovir disoproxil fumarate (TDF), were also conducted and showed no difference in the incidence of HCC between patients on TAF and TDF, or TAF and entecavir [57,58].
Based on the aforementioned studies, it commonly appears that the preventive effects on HCC was more apparent for an antiviral drug with a shorter observation period, and thus, the follow-up duration may function as a determinant of preventive effects of antiviral drugs [59]. In general, in-hospital cohort studies report no difference between drugs, whereas studies of administrative, public database suggest a superiority of tenofovir to entecavir in lowering the risk of HCC occurrence [56]. These database studies have an advantage of including a large sample size, but also have some disadvantages, such as potential unbalanced distribution of HCC risk factors between drugs and different periods of ETV and TDF adminstration [60]. For these reasons, patients with favorable prognosis are more likely to be included in the tenofovir group than in the entecavir group. There could be additional confounders that are unable to be corrected for by any sophisticated statistical methods [60]. Therefore, the overall reliability of the comparative studies appears low, since each study is quite heterogeneous in terms of patient characteristics, severity of liver disease, study period, the time of drug availability, imbalance in the number of patients between drugs, and the analytical methods used [55]. The aforementioned studies on the chemopreventive effect of anti-HBV drugs represent mostly short observation period of less than 5 years. In theory, given the expected tumor doubling time during the development of HCC, it takes an average of 9–10 years for a single malignant transformed cell to grow to a clinically detectable size (~1 cm) [61]. Therefore, well-designed, large-scale randomized studies with longer follow-up duration are needed to determine the true difference in the prevention of HCC between antiviral drugs. Most importantly, before discussing the differential efficacy between drugs, it has to be emphasized that the risk of HCC does not completely disappear despite long-term antiviral treatment [62,63]. It is because, apart from inflammation caused by viral hepatitis, various other non-viral factors, such as underlying liver disease, demographic characteristics such as age and sex, alcohol, as well as metabolic diseases, can also contribute to hepatocarcinogenesis. In conclusion, secondary prevention of HCC through antiviral therapy in chronic hepatitis B is not complete [64].
The primary aim of chronic hepatitis C treatment is to achieve a sustained virologic response (SVR) that is defined as undetectable HCV RNA using polymerase chain reaction (PCR) at 12 or 24 weeks after the end of treatment. The HCV recurrence rate after an SVR is only about 1% in the long term, so it is regarded as a virological cure. The achievement of an SVR can prevent progression to cirrhosis and the development of HCC. However, patients with preexisting hepatic fibrosis should undergo regular surveillance for HCC, since there is a continuing risk of developing HCC even after achieving an SVR [50].
Interferon therapy has been consistently reported to reduce the incidence of HCC in chronic hepatitis C patients compared with untreated controls. In a meta-analysis of 20 studies (4,700 patients), the HCC risk was significantly reduced in the interferon treatment group (RR, 0.43; 95% CI, 0.33–0.56) and to a greater extent in patients with an SVR (RR, 0.35; 95% CI, 0.26–0.46) compared to the control group [65]. Another meta-analysis of 30 studies (approximately 25,000 patients) reported a 76% reduction in the incidence of HCC in patients with an SVR compared with those without an SVR [66]. These results were consistent regardless of the degree of hepatic fibrosis or the presence of cirrhosis. Direct-acting antivirals (DAAs) against HCV have recently been introduced successively, leading to an SVR achievement rate as high as 98–100%. A prospective cohort study recruiting 9,895 French patients with chronic HCV infection showed that exposure to DAA was associated with a significantly reduced risk for HCC (HR, 0.66; 95% CI, 0.46–0.93) [67]. Other two large-scale independent studies revealed consistent results from DAA treatment: in a study involving a prospective cohort of 2,249 Italian cirrhotic patients, the absence of an SVR (HR, 3.40; 95% CI, 1.89–6.12) was independently associated with an increased risk for HCC [68]; another cohort study that prospectively recruited 1,760 patients with chronic hepatitis C in Latin America showed that attaining an SVR (HR, 0.2; 95% CI, 0.1–0.8) significantly reduced the risk of de novo occurrence of HCC [69]. In a meta-analysis comparing the risk of HCC between DAA treatment and interferon therapy, the incidence and recurrence rates of HCC were not different between the two treatments after adjusting the follow-up period and patient age [70]. In summary, acquisition of SVR, whether treated with interferon or DAA, leads to a reduced risk of HCC by 70–75% [70,71]. Therefore, achieving SVR is an important immediate therapeutic goal to reduce the risk of HCC.
Tertiary prevention of HCC
HCC is associated with a high rate of recurrence even after curative treatment. In fact, the 5-year recurrence rate is as high as 50–70%; therefore, tertiary prevention is very important. Recurrence within 2 years after curative treatment is highly likely to be metastasis of the primary tumor, and adjuvant cytotoxic chemotherapy has previously been attempted without proving reduction in recurrence or prolongation of survival [50].
There has been a paucity of well-designed RCTs that determined whether antiviral treatment could reduce the incidence of HCC after hepatic resection in patients with chronic HBV or HCV infection. However, many observational studies have reported that oral antiviral therapy after curative treatment of HBV-associated HCC can significantly reduce recurrence of HCC by up to 50% (HR, 0.48; 95% CI, 0.32–0.70) [72]. A meta-analysis that compared HCC recurrence between antiviral-treated and untreated patients after curative treatments (i.e., hepatic resection, radiofrequency ablation [RFA], and percutaneous ethanol injection [PEI]) showed that antiviral treatment for HBV significantly reduced the recurrence of HCC (odds ratio [OR], 0.59; 95% CI, 0.35–0.97), liver-related mortality (OR, 0.13; 95% CI, 0.02–0.69), and overall mortality (OR, 0.27; 95% CI, 0.14–0.50) [73,74]. In a meta-analysis of studies investigating post-operative recurrence of HBV-related HCC, antiviral treatment led to a significant reduction in the overall mortality (HR, 0.69; 95% CI, 0.52–0.92) and recurrence (HR, 0.58; 95% CI, 0.49–0.70) in patients with high-level viremia (HBV DNA ≤20,000 IU/mL), but this effect was not observed in patients with low-level viremia (HBV DNA <20,000 IU/mL) [75]. There have also been some studies that focused on the differential post-operative recurrence between antiviral drugs. However, it remains inconclusive whether one drug is more effective than the other in reducing the recurrence of HCC, due to an ongoing controversy over the results observed between antiviral drugs [76-78]. Rather than comparing the preventive effects between individual antiviral drugs, it is more important to consider various factors beside the viral factor such as tumor factors (tumor size and number, vascular invasion, degree of tumor differentiation), techniques and types of curative treatment, and underlying liver disease which play important roles in the recurrence of HCC after treatment.
In a meta-analysis of interferon therapy after curative treatment for HCV-associated HCC that observed 665 patients for 2 to 7 years, the achievement of an SVR was associated with a 74% reduction in the HCC recurrence rate and a 60% reduction in the mortality rate [79]. In another meta-analysis, HCC recurrence was significantly lower in the interferon-treated group than in the non-treated group after hepatic resection (ORs of 0.52, 0.23, 0.41, 0.37 at 1, 2, 3, and 5 years, respectively) [74]. Earlier reports of cases series suggested that HCC recurrence occurred earlier and more commonly after DAA treatment [80,81]. Regarding such phenomenon, it has been hypothesized that rapid reduction in the HCV viral load with DAAs may cause a decrease in immune surveillance against intrahepatic microscopic tumor clones, leading to an enhanced early recurrence [82,83]. However, recent analyses yielded contradictory results. In a large-scale prospective cohort study of the French Agency for AIDS and Viral hepatitis Research, the recurrence rate after the curative treatment of HCC was not significantly different between the DAA-treated group and the no-treatment group; nevertheless, there was a significantly higher HCC recurrence rate in the no-treatment group in the presence of compensated cirrhosis [84]. In addition, among liver transplant recipients, there was no difference in the incidence of HCC between the DAA-treated and non-treated groups. In a prospective cohort study conducted in Italy, DAA was not associated with HCC recurrence after curative treatment; however, the acquisition of SVR resulted in a significant reduction of HCC recurrence (HR, 0.25; 95% CI, 0.11–0.57) [85]. A series of systematic review and meta-analysis investigating the relationship between DAA treatment and HCC recurrence also showed that DAA treatment did not increase HCC recurrence, but rather appeared to decrease the recurrence of HCC when an SVR was achieved [70,83,86]. Nevertheless, there is considerable heterogeneity among studies in terms of patient characteristics, the timing of DAA administration, duration of follow-up, and the interval or method of surveillance for HCC. Therefore, it is still difficult to conclude whether DAA increases or decreases recurrence after curative treatment of HCC, which remains an open question to be answered in future studies.
There have been some studies that explored the potential effects of NSAIDs, including aspirin, on recurrence in patients with HCC undergoing hepatic resection. The two meta-analyses suggested that only the non-aspirin NSAIDs were associated with significant risk reduction in the recurrence of HCC, unlike aspirin which showed unclear preventive effects against post-treatment recurrence [38,87]. However, these results should be interpreted with caution since the studies represented only a small sample size and conflicting results, together with significant heterogeneity in methodology. It was also reported that the use of these drugs was associated with a non-negligible risk of hemorrhagic complications in patients with HCC. Therefore, the administration of NSAIDs, including aspirin, or antiplatelet agents for the purpose of preventing recurrence should be decided carefully. On the other hand, several retrospective cohort studies have suggested a preventive effect of statin on recurrence after curative treatment of HCC [88,89]. In agreement with the results, two Korean studies involving transplant recipients also showed that statin use was associated with a significant risk reduction of HCC recurrence after liver transplantation (LT) [90,91]. Large-scale prospective studies are needed to confirm the preventive roles of these medications on recurrence after curative treatment of HCC.
[Recommendations]
1. All newborns (A1) and seronegative (negative for all of HBsAg, anti-HBs, and anti-HBc) children and adults should be vaccinated against HBV (B1) to prevent HCC.
2. General HCC preventive measures include the following: prevention of HBV/HCV transmission (A1); avoidance of alcohol abuse; and control of metabolic disorders, such as obesity and diabetes (C1).
3. Antiviral therapy as a secondary prevention of HCC should follow the KASL guidelines for the management of chronic hepatitis B or C (A1).
4. The risk of HCC can be reduced if HBV replication is persistently suppressed in patients with chronic hepatitis B (A1), and if an SVR is achieved by interferon therapy (A2) or DAA therapy (B1) in patients with chronic hepatitis C.
5. Among patients with chronic liver disease, the risk of developing HCC is lower in patients receiving statin therapy for the management of dyslipidemia compared to those undergoing no treatment (B1).
6. Among patients with chronic liver disease, the risk of developing HCC is lower in patients receiving aspirin therapy for the purpose of preventing cardiovascular complications or managing pain and inflammation compared to those undergoing no treatment. However, the administration of aspirin for patients with liver cirrhosis should be considered with caution as the risk of gastrointestinal bleeding may increase (B2).
7. Coffee consumption in patients with chronic liver disease can lower the risk of HCC (B1).
8. After curative treatment of HBV-associated HCC, antiviral therapy should be considered to reduce the risk of HCC recurrence in patients with detectable serum HBV DNA (B1).
9. After curative treatment of HCV-associated HCC, the association of DAA therapy with the risk or prevention of HCC recurrence remains unclear (C1).
SURVEILLANCE
The major purpose of intensive surveillance for cancer is to reduce disease-related mortality. There are two RCTs on the efficacy of surveillance programs in reducing HCC-related mortality among individuals at risk of HCC. In a Chinese study of 5,581 chronic hepatitis B patients recruited in the early 1990s, surveillance for HCC using only 6-monthly alpha-fetoprotein (AFP) assays resulted in an earlier diagnosis of HCC; however, the gain in lead time did not result in a significant reduction in overall mortality due to ineffective treatments for HCC [92]. In contrast, a large-scale randomized trial involving 18,816 Chinese patients with chronic hepatitis B demonstrated that, despite poor study adherence (58.2%), a strategy of surveillance with ultrasonography (US) and AFP measurement every 6 months significantly reduced HCC-related mortality by 37% compared to no surveillance. In addition, the surveillance strategy was associated with a higher rate of detection of small HCC and surgically amenable HCC, as well as better overall survival (OS) after the diagnosis of HCC [93]. Several non-randomized cohort studies and meta-analyses have also found that surveillance has led to the detection of more early stage HCCs, provided a higher rate of curative treatments, and a significantly better OS than that found in the control group, indicating the compelling justification for HCC surveillance in at-risk patients [94-98]. In a meta-analysis of 32 HCC surveillance studies with a total of 13,367 cirrhotic patients, the sensitivity for detecting all stages of HCC was 84% (47% in early stage) with US alone, whereas combining serum AFP and US increased the RR of HCC detection at all stages and early stage to 0.88 and 0.81, respectively [99]. US and serum AFP measurement was reported to be cost-effective as an HCC surveillance tool. In a study using Markov model of 1 million cirrhotic patients, three groups of US alone, US and serum AFP measurement and no surveillance were compared. With the assumption of HCC incidence ≥0.4%/year, adherence to surveillance test >19.5%, and willingness-to-pay threshold of 100,000 USD, performing the combination of US and serum AFP measurement every 6 months was the most cost-effective [100].
Unlike other malignancies, HCC has well-established risk factors that allow the identification of an at-risk patient group. Since approximately 90% of HCC cases are associated with a well-known risk factor, most of the international guidelines have been adapted to perform HCC surveillance in the population at risk of HCC development [95]. Patients with cirrhosis derived from any etiology are regarded as the most important targets to undergo a surveillance program, since more than 80% of patients diagnosed with HCC have underlying cirrhosis. Viral hepatitis is also one of the most important causal risk factors for HCC. Chronic HBV infection is responsible for around 70% of all patients diagnosed with HCC in East Asia, including Korea, whereas chronic HCV infection accounts for around 30% of HCC patients in Western countries, with most of the HCV-associated HCC patients having either cirrhosis or advanced fibrosis at diagnosis. However, one Korean study on patients who underwent hepatic resection shown that 32.5% of HCV-related HCCs were not associated with underlying cirrhosis, indicating a lower rate of HCV-related HCC accompanying cirrhosis than that reported in Western countries [101]. In addition, the risk of HCC also increases with the patient’s age, excessive alcohol drinking, male sex, and diabetes mellitus, and risk is higher among Asian HBV carriers with high viral activity and family history of the disease, and chronic hepatitis B patients with cirrhosis or advanced fibrosis [102,103]. Based on a cost-effectiveness study, it is generally accepted that an annual incidence of HCC surpassing 1.5% would warrant a surveillance scheme of HCC in cirrhotic patients [104]. However, patients with chronic HBV infection can develop HCC in the absence of underlying cirrhosis. Therefore, expert opinion indicates that HCC surveillance for chronic HBV carriers is deemed to be cost-effective if the annual incidence exceeds 0.2% [105]. Given this definition, patients with liver cirrhosis of all etiologies, chronic HBV infection, or chronic HCV infection with cirrhosis or advanced fibrosis are the major target population for surveillance as a high risk group for HCC. From a pooled analysis of previously published studies on the natural history of various liver diseases, patients with liver cirrhosis are at the highest risk of developing HCC, irrespective of etiology. Patients with chronic HBV infection and those with HCV-related cirrhosis or advanced fibrosis are also at a high risk of HCC, of which annual incidences exceed 0.2% and 1.5%, respectively [95,105].
In particular, HCV-infected patients with cirrhosis or advanced liver fibrosis (≥F3) need to receive HCC surveillance even after they achieve SVR by DAA treatment. Transient elastography is known to well predict the risk of HCC development in treatment-naïve HCV-infected patients. However, data are scarce regarding the performance of transient elastography in predicting the risk of HCC in HCV patients who achieved SVR after antiviral therapy. In addition, since patients who achieved SVR may still develop HCC, if cirrhosis or advanced fibrosis had not been ruled out by biopsy, patients should be in the HCC surveillance program [81,106-108].
According to the increasing availability of non-invasive biomarkers or imaging which assess liver fibrosis, it has been suggested that patients with NAFLD who were found to have cirrhosis or advanced fibrosis by these tests should receive HCC surveillance. For example, if FIB-4, which is a non-invasive liver fibrosis marker using age, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and platelet count, is more than 2.67, there is a high probability of cirrhosis or bridging fibrosis. Thus, in this case, a patient with NAFLD needs to receive HCC surveillance [109].
In general, US with or without AFP is widely used as a tool for HCC surveillance in high-risk patients. However, globally there are some regional discrepancies regarding the recommended surveillance methods. Among tumor markers relevant to HCC, information on surveillance are mostly limited to AFP, and therefore almost all studies focusing on the effectiveness of a surveillance program have implemented only AFP as a tumor marker for HCC. The sensitivity of detecting an early stage HCC in high-risk patients is reportedly approximately 60% when performing surveillance using US with or without serum AFP measurement [110-112]. The sensitivity and specificity of US as a surveillance tool for HCC in patients with chronic HBV infection were reported to be 65–80% and over 90%, respectively, with a higher sensitivity compared to serum markers such as AFP [98,113]. While AFP measurement and US are imperfect tools, they appear to be mutually complementary [103]. In a meta-analysis of 16 relevant studies, the combined use of US and AFP measurement yielded a higher sensitivity for HCC detection compared to US alone (0.79 [95% CI, 0.57–0.91] vs. 0.69 [95% CI, 0.46–0.85]), although it was not statistically significant [98]. In another meta-analysis of 13 selected studies, the pooled sensitivity for detecting early-stage HCC increased from 63% with US alone to 70% with US combined with AFP measurement [94]. A pooled analysis of seven studies on patients with cirrhosis showed that US with and without AFP measurement detected early-stage HCC with 63% sensitivity (95% CI, 48–75%) and 45% sensitivity (95% CI, 30–62%), respectively, indicating a higher sensitivity by US combined with AFP measurement than by US only [99]. The performance of surveillance varies depending on the cut-off levels of biomarkers and the prevalence of HCC among the general population in the region. In the United States and Europe, where the prevalence of HCC is relatively low, only the US examination is often recommended as a surveillance method. On the other hand, in South Korea and Japan, where the HCC prevalence is high, it is recommended to perform US with serum AFP measurement for HCC surveillance in the high-risk population [114-116].
The interval of cancer surveillance should be determined based on tumor doubling time, time to stage migration to enable curative treatments at diagnosis, cost-effectiveness, and its impact on patient survival. Although the optimal surveillance intervals for patients at risk of HCC are yet to be clearly determined, the intervals of HCC surveillance recommended by most of the regional guidelines range from 3 to 12 months [105,114-117]. An Italian study that compared 6- vs. 12-month surveillance failed to increase the detection rate of a single nodular tumor with 6-month surveillance compared to 12-month surveillance [118]. A RCT that evaluated more intense surveillance of 3- vs. 6-month intervals also provided similar results in detecting small HCCs [119]. In contrast, another Italian study on the performance of semiannual surveillance showed that it increased the detection rate of early-stage HCC and patient survival compared to an annual program [97]. Another randomized trial evaluating US as a surveillance tool in Taiwanese patients with viral hepatitis demonstrated that a 4-month interval scheme performed better in detecting very early stage HCC compared to a 12-month interval, although it did not provide a survival benefit [120]. Moreover, the pooled sensitivity of detecting HCC increased from 50% with the annual scheme to 70% with the semiannual surveillance [94]. In a cost-effective study, a semiannual US surveillance program in cirrhotic patients also resulted in improved clinical outcomes at a reasonable cost [121]. The mean tumor doubling time of small HCCs (<5 cm) is estimated to be around 4–7 months, ranging between 136 and 204 days [122,123], and semiannual surveillance was the interval employed in the only RCT that showed a survival benefit with an HCC surveillance scheme [93]. Thus, taken together, a 6-month interval for an HCC surveillance program would be considered a preferable and reasonable strategy.
Given that the incidence of HCC varies according to the cause of underlying liver disease and the degree of cirrhosis even in the high-risk group, some groups may be at a higher risk of HCC than others. Under circumstances in which HCC is highly suspected, contrast-enhanced US (CEUS), liver dynamic computed tomography (CT), or contrast-enhanced magnetic resonance imaging (MRI) can be performed as an alternative to US when an US examination fails to detect nodules or is incomplete due to poor visualization. With the advantage of being able to assess the blood supply and vascular invasion of tumors, CEUS has been found to be more cost-effective in surveillance for HCC than US alone [124].
A recent randomized trial that compared biannual US with yearly contrast CT has shown the former to be marginally more sensitive and less expensive for the detection of early HCC in patients with compensated cirrhosis. Recently, MRI with liver-specific contrast in a surveillance setting of cirrhotic patients has resulted in a higher detection rate of HCC and lower false-positive findings compared to US [125]. Due to the incomplete performance of US as a surveillance tool, the need for an alternative imaging test which can avoid radiation exposure and contrast agent is increasing. An abbreviated MRI with or without contrast agent reduced the scanning time and images acquired, and it is gaining attention as an alternative tool to US in HCC surveillance. In three prospective studies and 12 retrospective studies, 917 patients developed HCC among 2,807 patients who received surveillance with abbreviated MRI or US. In a meta-analysis of these 15 studies, the sensitivity and specificity of non-contrast abbreviated MRI were similar to those of contrast-enhanced abbreviated MRI (86% vs. 94%; 87% vs. 94%, respectively). Also, the sensitivity of abbreviated MRI was higher compared to US (82% vs. 53%) [126]. However, the information on the alternative surveillance imaging strategies is very limited and should be interpreted carefully. Study results regarding the diagnostic performance of CT or MRI for HCC cannot be directly extrapolated to the setting of cancer surveillance. Regarding abbreviated MRI, most studies were retrospective and non-randomized. Particularly, the safety of MRI contrast has not been guaranteed in a surveillance setting, which might be another limitation of contrast-enhanced MRI as a surveillance tool. In addition, the risks, accessibility, and cost-effectiveness of these alternative imaging methods should be meticulously evaluated. Therefore, further studies on the accuracy, costs, and potential harms regarding these new radiological modalities are needed before the wide implementation of the alternative imaging surveillance strategies.
[Recommendations]
1. Surveillance for HCC should be performed in high-risk groups; patients with chronic hepatitis B (A1), chronic hepatitis C (B1), and liver cirrhosis (A1).
2. Surveillance test for HCC should be performed with liver US plus serum AFP measurement every 6 months (A1).
3. When liver US cannot be performed adequately, dynamic contrast-enhanced CT or dynamic contrast-enhanced MRI can be performed as an alternative (C1)
DIAGNOSIS
HCC can be diagnosed either pathologically by biopsy or clinically by the use of non-invasive imaging in high-risk groups (chronic hepatitis B, chronic hepatitis C, or cirrhosis) [127-133]. If a new liver nodule ≥1 cm in size is detected by surveillance test in high-risk patients, a first-line imaging study, such as dynamic contrast-enhanced CT or dynamic contrast-enhanced MRI with extracellular contrast agents or hepatocyte-specific contrast agents like gadoxetic acid (gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid; Gd-EOB-DTPA), should be performed for the imaging diagnosis of HCC (Fig. 3). Since imaging-based diagnosis of HCC relies on the dynamic contrast enhancement characteristics on multiphasic CT or MRI, single phase CT or MRI may not be used as a diagnostic tool. The etiology of cirrhosis does not influence the imaging diagnosis of HCC but it should be applied with caution in patients with cirrhosis due to vascular disorders, such as Budd-Chiari syndrome, or due to Fontan-associated liver disease, as such conditions are often accompanied with benign hyperplastic nodules that can mimic HCC on imaging [134,135].

Diagnostic algorithm. HCC, hepatocellular carcinoma; CHB, chronic hepatitis B; CHC, chronic hepatitis C; CT, computed tomography. *The radiological hallmarks for diagnosing “definite” HCC on multiphasic contrast-enhanced CT or magnetic resonance imaging (MRI) are arterial phase hyperenhancement (APHE) with washout appearance in the portal venous, delayed, or hepatobiliary phases. These criteria should be applied only to a lesion that does not show either marked T2 hyperintensity or targetoid appearances on diffusion-weighted images or contrast-enhanced images. For a second-line imaging modality, the radiologic hallmarks of contrast-enhanced ultrasonography (blood-pool contrast agent or Kupffer cell-specific contrast agent) for a “definite” diagnosis of HCC are APHE with mild and late (≥60 seconds) washout. These criteria should be applied only to a lesion that does not show either rim or peripheral globular enhancement in the arterial phase. †For the diagnosis of “probable” HCC, ancillary imaging features are applied as follows: there are two categories of ancillary imaging features, including imaging features favoring malignancy in general (mild-to-moderate T2 hyperintensity, restricted diffusion, threshold growth) and those favoring HCC in particular (enhancing or non-enhancing capsule, mosaic architecture, nodule-in-nodule appearance, fat or blood products in the mass). For nodules without APHE, “probable” HCC can be assigned only when the lesion fulfills at least one item from each of the two categories of ancillary imaging features. For nodules with APHE but without washout appearance, “probable” HCC can be assigned when the lesion fulfills at least one of the aforementioned ancillary imaging features.
A recent meta-analysis regarding the imaging diagnosis of HCC showed a per-lesion sensitivity of 66% (95% CI, 60–72%) for multiphasic CT and 82% (95% CI, 75–87%) for multiphasic MRI (extracellular contrast agents or hepatocyte-specific contrast agents), and a per-lesion specificity of 92% (95% CI, 84–96%) for multiphasic CT and 91% (95% CI, 82–95%) for multiphasic MRI [136]. Using the 2018 KLCA-NCC imaging criteria for HCC diagnosis, recent retrospective studies reported that MRI using hepatocyte-specific contrast agent had a per-lesion sensitivity of 87% and a per-lesion specificity of 86% [137], and MRI using hepatocyte-specific contrast agent had a higher sensitivity than extracellular contrast agent (79% vs. 69%), but similar specificity (96% vs. 94%) [138].
When an imaging diagnosis of HCC cannot be made on a first-line imaging study, a second-line imaging study can be applied to enhance the sensitivity of HCC diagnosis [139,140]. Imaging modalities for second-line studies include multiphasic CT, multiphasic MRI with extracellular contrast agents or hepatocyte-specific contrast agents, and CEUS with blood-pool contrast agents or Kupffer cell-specific contrast agents (Fig. 3). CEUS with blood-pool contrast agents showed high specificity for HCC diagnosis in a recent large multi-center retrospective study [141]. Moreover, a meta-analysis found that CEUS had a sensitivity of 84% (95% CI, 79–87%) and a positive predictive value of 89% (95% CI, 86–93%), which was comparable to multiphasic CT and MRI with extracellular contrast agents [142]. However, considering that the purpose of diagnostic imaging study also includes determining the tumor extent and staging, CEUS has limitations in these aspects, and therefore, is not recommended as a first-line imaging study. Instead, it can be used as one of second-line imaging studies if the first-line imaging study is inconclusive.
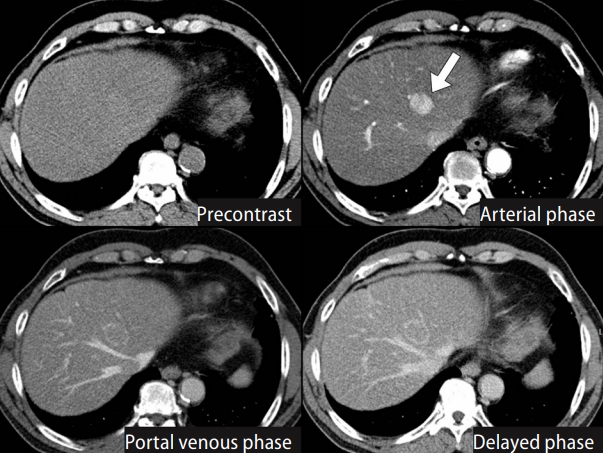
Non-invasive diagnosis of “definite” HCC is based on the radiological hallmarks on multiphasic CT or multiphasic MRI (extracellular contrast agents or hepatocyte-specific contrast agents) for a liver nodule ≥1 cm detected in high-risk patients. The radiological hallmarks for diagnosing “definite” HCC are arterial phase hyperenhancement (APHE) with washout appearance in the portal venous, delayed, or hepatobiliary phases (hepatobiliary phase finding is included if hepatocyte-specific contrast agents are used) (Table 3, Fig. 4). The definition of each imaging feature used for HCC diagnosis in this guideline adopts the latest Liver Imaging Reporting and Data System (LI-RADS) lexicon (https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS).
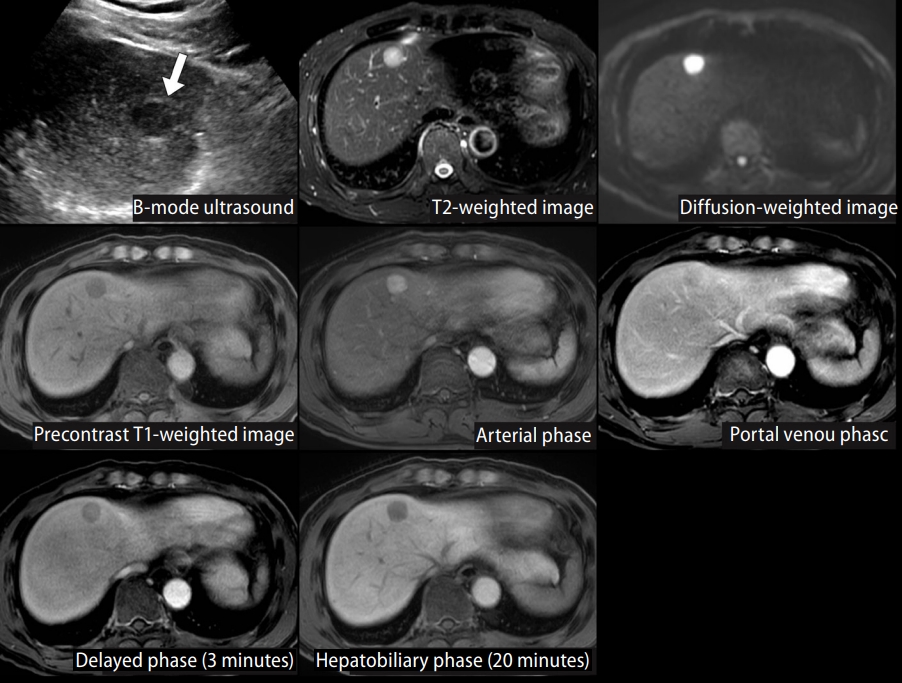
Definite hepatocellular carcinoma (HCC) on multiphasic magnetic resonance imaging (MRI) with hepatocyte-specific contrast agent. A 1.7-cm liver nodule (arrow) is detected on surveillance ultrasound in a patient with liver cirrhosis. The lesion shows the radiological hallmarks of HCC, i.e., arterial phase hyperenhancement and washout appearance (portal venous phase, delayed phase, and hepatobiliary phase) on multiphasic MRI using hepatocyte-specific contrast agent (gadoxetic acid) but does not show marked T2 hyperintensity or targetoid appearances on diffusion-weighted images and contrast-enhanced images. Therefore, this nodule can be noninvasively diagnosed as “definite” HCC.
Prospective studies have demonstrated that the imaging criteria of APHE with washout appearance on portal venous or delayed phases on multiphasic CT or MRI resulted in sensitivities of 65–89% and specificities of 91–100% [139,140]. Following these criteria provides high specificity but limited sensitivity, especially for nodules less than 2 cm in diameter (sensitivity, 41–62%) [143,144]. However, when hypointensity in the hepatobiliary phase is also considered equal to washout appearance, sensitivity is increased [145-147]. Given the medical environments in South Korea where hepatocyte-specific contrast agent is commonly used for liver MRI and pursues early detection and treatment of HCC, high sensitivity is preferred for the diagnosis of HCC. Therefore, since the previous version (ver. 2018), KLCA-NCC guidelines have defined washout appearances in not only the portal venous and delayed phases but also the hepatobiliary phase. It should be noted that this principle carries the risk of misdiagnosis of hemangioma and intrahepatic cholangiocarcinoma (CCA) as an HCC [147]. Therefore, in order to exclude hemangioma and intrahepatic CCA, these diagnostic criteria should not be applied in lesions showing marked T2 hyperintensity or targetoid appearances on diffusion-weighted images or contrast-enhanced images. In addition, focal eosinophilic liver diseases are relatively common in South Korea, which can mimic HCC on imaging, especially on MRI using hepatocyte-specific contrast agents. To avoid a false-positive diagnosis, the peripheral eosinophil count should be checked before making an imaging diagnosis of HCC [148]. For the assessment of APHE, the use of arterial subtraction images can increase the sensitivity of HCC diagnosis by detecting more APHEs, especially for nodules with precontrast T1 hyperintensity or with equivocal enhancement on arterial phase images [149-151]. However, to avoid false-positive diagnosis, the use of arterial subtraction imaging to detect APHE is recommended only in lesions without rim APHE. In addition, for the imaging diagnosis of HCC, recent studies have reported that the combination of imaging findings from multiphasic CT and multiphasic MRI may improve diagnostic performance compared to CT or MRI alone [152,153].
If there is a tumor thrombus in the portal vein or hepatic vein, which is often associated with HCC, HCC can be diagnosed based on imaging findings of the contiguous parenchymal mass. In cases of HCC with tumor thrombus, the parenchymal mass frequently shows atypical imaging features, and sometimes only tumor thrombi are present without a visible parenchymal mass, making it difficult to diagnose HCC [154]. Since non-HCC malignancies, including intrahepatic CCA or combined hepatocellular-cholangiocarcinoma (combined HCC-CCA), may also rarely be accompanied by tumor thrombus [155,156], it would be inappropriate to diagnose HCC with the sole finding of tumor thrombus on imaging.
When CEUS (blood-pool contrast agents or Kupffer cell-specific contrast agents) is performed as a second-line imaging study for a nodule ≥1 cm detected in high-risk patients, the radiological hallmarks for diagnosing “definite” HCC are APHE with late (≥60 seconds) and mild washout or washout appearance in the Kupffer phase (Kupffer phase finding is included if Kupffer cell-specific contrast agents are used) (Fig. 5). If a nodule shows early washout (<60 seconds) or punched-out pattern washout within 120 seconds after contrast injection, it should be excluded due to the possibility of non-HCC malignancies, such as intrahepatic CCA or metastasis [157]. In addition, these criteria should not be applied to lesions presenting with rim or peripheral globular enhancement on arterial phase, which are typical imaging features of intrahepatic CCA and hemangioma, respectively [157]. As discussed above, CEUS with blood-pool contrast agent showed comparable diagnostic performance to multiphasic CT or MRI [142]. Moreover, regarding CEUS with Kupffer cell-specific contrast agents, a recent meta-analysis found a good overall diagnostic performance, with a sensitivity of 90% (95% CI, 82–95%) and a specificity of 97% (95% CI, 93–98%) [158]. A prospective intra-individual comparative study reported that CEUS with Kupffer cell-specific contrast agents had a significantly higher sensitivity compared to CEUS with blood-pool contrast agents (79% [95% CI, 64–90%] vs. 54% [95% CI, 38–67%]), without difference in specificity (100% [95% CI, 79–100%] vs. 100% [95% CI, 79–100%]) [159]. In another prospective study, CEUS with Kupffer cell-specific contrast agents demonstrated diagnostic performances similar to multiphasic CT or multiphasic MRI [160].

Definite hepatocellular carcinoma (HCC) on contrast-enhanced ultrasound. A 3.5-cm liver nodule is detected in a patient with chronic hepatitis B. On contrast-enhanced ultrasound using blood-pool contrast agent, the nodule shows arterial phase hyperenhancement and mild washout on 3 minutes delayed image. Therefore, it can be noninvasively diagnosed as “definite” HCC.
In nodules ≥1 cm that do not meet the non-invasive diagnostic criteria of “definite” HCC, a diagnosis of “probable” HCC can be assigned by applying ancillary imaging features (Table 4, Figs. 6, 7) [161]. There are two categories of ancillary imaging features: i) imaging features favoring malignancy in general (mild-to-moderate T2 hyperintensity, restricted diffusion, threshold growth) and ii) those favoring HCC in particular (enhancing or non-enhancing capsule, mosaic architecture, nodule-in-nodule appearance, fat or blood products in the mass). For nodules without APHE, “probable” HCC can be assigned only when the lesion fulfills at least one item from each of the two categories of ancillary imaging features. For nodules with APHE but without washout appearance, “probable” HCC can be assigned when the lesion fulfills at least one of aforementioned ancillary imaging features. Like “definite” HCC, the diagnosis of “probable” HCC should be applied only to a lesion which does not show either marked T2 hyperintensity or targetoid appearances on diffusion-weighted images or contrast-enhanced images to rule out the possibility of hemangioma or intrahepatic CCA. “Probable” HCC in this guideline corresponds to the concept of LR-4 (probably HCC) of the LI-RADS. In a recent meta-analysis, the pooled percentages of LR-4 nodules confirmed as HCC and overall malignancy were 74% and 80%, respectively [162]. During follow-up, 20–34% of LR-4 nodules progressed to LR-5 (definitely HCC) within 3 months and 37–75% to LR-5 within 6 months [163-165]. For “probable” HCC, therefore, a follow-up imaging study within 3 months or biopsy should be considered, and a treatment plan for the lesion may be determined through multidisciplinary discussion.
Probable hepatocellular carcinoma (HCC) on dynamic contrast-enhanced computed tomography (CT). On dynamic contrast-enhanced CT in a patient with chronic hepatitis B, there is a 2-cm liver nodule (arrow) with arterial phase hyperenhancement. This nodule does not show a washout appearance in the portal venous phase or delayed phase, so it cannot be non-invasively diagnosed as “definite” HCC. However, based on the presence of enhancing capsule in the portal venous phase and delayed phase, an ancillary imaging feature of HCC, this nodule can be diagnosed as “probable” HCC.
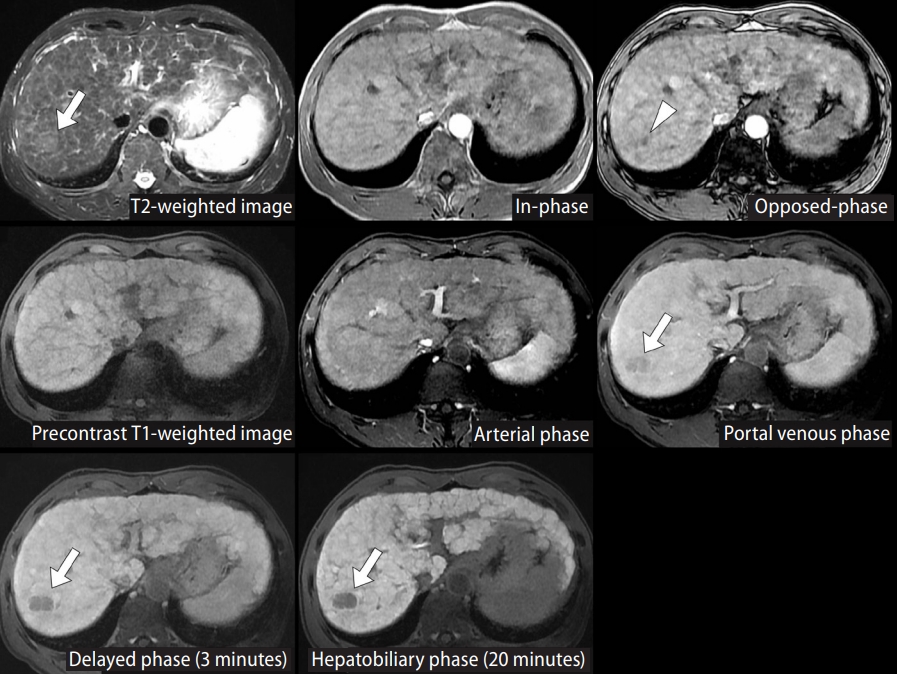
Probable hepatocellular carcinoma (HCC) on multiphasic magnetic resonance imaging (MRI) with hepatocyte-specific contrast agent. On multiphasic MRI with hepatocyte-specific contrast agent (gadoxetic acid), a 2.5-cm nodule (arrows) is found in segment VII of the liver in a patient with liver cirrhosis. This lesion is indistinguishable from surrounding liver parenchyma on precontrast T1-weighted image and arterial phase image but shows hypointensity on portal venous phase, delayed phase, and hepatobiliary phase images. Since it does not show arterial phase hyperenhancement, an imaging diagnosis of “definite” HCC cannot be made. However, it shows mild-to-moderate T2 hyperintensity and focal signal drop on the opposed phase image in comparison with an in-phase image, which suggests the presence of intra-tumoral fat. Therefore, based on MRI ancillary imaging features, this nodule can be diagnosed as a “probable” HCC.
For nodules detected by surveillance, if imaging studies cannot make a diagnosis of “definite” or “probable” HCC, they can be assigned as an “indeterminate” nodule. The category of “indeterminate” corresponds to the concept of LR-3 (indeterminate probability of malignancy) of the LI-RADS. In a recent meta-analysis, the pooled percentages of LR-3 nodules confirmed as HCC and overall malignancy were 38% and 40%, respectively [162]. During follow-up, 0–25.8% of LR-3 lesions progressed to LR-5 (definitely HCC) within 6 months and 8.9–57.3% to LR-5 in 6–12 months [163-165]. In addition, according to a Korean domestic study on the prediction of progression to HCC, among 474 indeterminate nodules ≤2 cm in HBV-related cirrhosis, 17% progressed to HCC during a median follow-up of 36 months. In this study, old age, presence of APHE, large nodule size (>1 cm), low serum albumin level (≤3.5 g/dL), and high serum AFP level (≥100 ng/mL) were identified as independent risk factors for progression to HCC [166]. For an “indeterminate” nodule, a follow-up imaging study within 6 months or biopsy should be considered, taking into account the probability of HCC and its potential future progression to HCC. The International Liver Cancer Association recommends follow-up of up to 2 years for indeterminate nodules, considering the doubling time of HCC [167].
For subcentimeter nodules detected on HCC surveillance in high-risk patients, follow-up surveillance within 6 months is recommended. With recent advances in imaging techniques, subcentimeter nodules with characteristic imaging features of HCC are more commonly found. Some HCC guidelines from Asian countries allow the imaging diagnosis of subcentimeter HCC [116,129,168]. In addition, recent studies have revealed that the use of ancillary imaging features may improve the diagnostic performances for subcentimeter HCCs [148,169-172]. However, the sensitivity of imaging diagnosis for subcentimeter HCCs is reported to be lower than that of HCCs ≥1 cm (<1 cm vs. ≥1 cm: 31% vs. 82%, P<0.001 for CT; 48% vs. 88%, P=0.02 for MRI) [173]. Even MRI with hepatocyte-specific contrast agents showed a significantly lower per-lesion sensitivity (46%) and positive predictive value (48%) for subcentimeter HCCs than those for HCCs ≥1 cm (sensitivity, 95%; positive predictive value, 78%) [171]. In a retrospective study of subcentimeter nodules showing typical imaging features on MRI with hepatocyte-specific contrast agents, the specificity for HCC diagnosis was reported to be 50% [174], which was very low compared to the specificity of approximately 90% in nodules ≥1 cm [137]. These results suggest that the probability of a false positive diagnosis is high for subcentimeter nodules. Therefore, a conservative approach is preferred in subcentimeter nodules, with close monitoring of interval growth or changes in the imaging features in follow-up studies within 6 months.
For the pathologic diagnosis of HCC, biopsy is considered a relatively safe procedure. However, in clinical practice, it is often difficult to perform a biopsy due to the presence of ascites, bleeding risk associated with poor hepatic function, concerns for needle track seeding, or challenges in tumor targeting. Biopsy techniques for the liver nodules in cirrhotic patients include core needle biopsy, fine needle aspiration cytology, and fine needle aspiration biopsy. Among them, only core needle biopsy is recommended for the diagnosis of early HCC or dysplastic nodule, as it enables the observation of cellular and structural atypia. Cytology examination methods, such as fine needle aspiration cytology and fine needle aspiration biopsy, can be helpful in the diagnosis of advanced HCC with moderate or poor differentiation. The sensitivity of the pathologic diagnosis for HCC has been reported to be about 72%; however, it varies depending on the tumor location, size, and degree of differentiation. Its sensitivity is lower in small HCCs of <2 cm [175,176], or when tumors that are difficult to target are included [175]. As the risk of tumor seeding due to biopsy has been reported to be 0.6–5.1%, there is considerable objection to the biopsy procedure in patients who are likely to be cured by surgery or LT [177,178]. Moreover, with biopsy, it is difficult to detect stromal invasion which is a critical clue to differentiate early HCC from dysplastic nodule, and the false negativity of biopsy was reported to be approximately 33% [175,176]. Hence, the majority of HCCs are non-invasively diagnosed using imaging studies in clinical practice.
Clinical interests in the pathologic diagnosis in addition to the imaging diagnosis have recently been increasing in order to diagnose HCC at an earlier phase. Since the majority of early HCC consists of well-differentiated tumor, histologic analysis (a combination of small cell change and increased cell density [>2 times that of the surrounding tissue], pseudo-glandular pattern, unpaired arteries and frequent absence of portal veins, and stromal invasion), together with immune-histochemical staining of the relevant markers (marker panel; heat shock protein 70, glypican 3, and glutamine synthetase) are useful for its diagnosis. In particular, when two of the above markers are positive, the sensitivity and specificity for diagnosing early HCC were reported to be 60% and 100%, respectively [179]. Given that imaging studies sometimes fail to differentiate between HCC and less common primary liver cancers, including combined HCC-CCA and intrahepatic CCA, biopsy is required when an accurate diagnosis is difficult due to atypical imaging features or an atypical clinical course. Confirmatory biopsy should also be considered for differential diagnosis of tumors that are refractory to the best standard treatment. For HCC or CCA with poor differentiation, it is hard to differentiate them only by histological findings; therefore, the diagnosis should be made by integrating the results of various immune-histochemical staining to identify hepatocyte differentiation (arginase-1, Hep Par-1, polyclonal carcinoembryonic antigen (CEA), CD10, glypican-3, and AFP, etc.) or cholangiocyte differentiation (K7, K19, and EpCAM, etc.) [180]. In addition, K19-expression, which is found in 4–28% of HCCs, is associated with poor prognosis, and in some cases it is necessary to differentiate the tumor from intrahepatic CCA when it is positive [181]. Based on the recent molecular and histopathologic findings, approximately 35% of HCCs can now be classified into specific subtypes. It has been reported that, in comparison to the conventional HCC, macrotrabecular-massive, neutrophil-rich, and vessel encapsulating tumor clusters (VETC) subtypes show worse prognosis; lymphocyterich and clear cell subtypes show relatively favorable prognosis; fibrolamellar, steatohepatitic, and chromophobe subtypes show similar prognosis; and scirrhous subtype shows similar or worse prognosis [182]. Recent advances in pathogenetic studies have suggested several categories according to the histopathologic features of HCC, which seem to be helpful in predicting the treatment response or prognosis in clinical practice or identifying therapeutic targets [183]. However, there are still no histological biomarkers that can directly guide treatment decisions. Therefore, in HCCs that can be diagnosed by imaging, it is necessary to further evaluate the role and value of biopsy in the upcoming era of precision medicine [184,185].
The role of serological biomarkers in diagnosing HCC is limited due to their high false-positive and false-negative rates [186]. Serum AFP levels remain within the normal range in 35% of patients with small HCCs, whereas the levels can be elevated not only in HCC patients but also in non-specific conditions, such as aggravation of hepatitis and active regeneration of hepatocytes [112,187,188]. Therefore, AFP alone is insufficient to make a diagnosis of HCC. Although recent retrospective multi-center studies have reported that serum AFP levels could improve the performance of distinguishing HCC from other diagnoses when combined with imaging features [189,190], the practical interpretation and application of these results have not been established yet.
To date, the criteria for diagnostic imaging on recurrent intrahepatic HCC are not well-established. However, in patients previously diagnosed with HCC, high sensitivity should be pursued since the pre-test probability of HCC is higher than those without [191,192]. Therefore, newly detected or growing nodules in a follow-up study of patients with a history of prior HCC can be diagnosed as recurrent HCC regardless of size, if they show radiological hallmarks of HCC or ancillary imaging features of HCC with an increase in size.
Radiation exposure dose and the risk of CT examination in HCC patients
The International Commission on Radiological Protection (ICRP) reported that the cancer risk after radiation exposure exhibits a linear no-threshold dose-response relationship [193,194]; therefore, it is critical to minimize the medical radiation exposure. However, there has been no report on the direct risk of diagnostic radiation exposure to patients. The dose of radiation exposure from four-phase liver CT is approximately 20–30 mSv. Moreover, according to the Biological Effects of Ionizing Radiation VII phase 2, the additional lifetime attributable risk of incidence and mortality of solid cancer or leukemia were reported as 0.148% and 0.09%, respectively, in a 50-year-old man exposed to 25 mSv of medical radiation [195,196]. The ICRP 2007 recommendations on radiological protection included the following: “Dose limits do not apply to medical exposures. If they did, the effectiveness of diagnosis or treatment might be reduced, doing more harm than good for the patient. The emphasis is on justification of medical procedures and optimization of protection [197].” In addition, the risk of radiation-associated malignancy is considered less significant in patients with decreased life expectancy, such as elderly or severely ill patients [198]. For this reason, it is not recommended to strictly limit the radiation dose for the diagnosis and follow-up evaluation of HCC. However, unnecessary CT examinations should be avoided, and alternative imaging studies should be considered particularly in patients with long life expectancy. Recently, various dose reduction techniques that do not impair the image quality or diagnostic ability for focal liver lesions, such as iterative reconstruction or deep learning-based reconstruction combined with low tube voltage, are being developed [199-203]. To optimize radiation exposure, the use of low-dose CT techniques as well as alternative imaging modalities, such as MRI, should to be considered in HCC patients.
[Recommendations]
1. The diagnosis of HCC can be made pathologically or using the typical hallmarks of HCC obtained by non-invasive imaging in high-risk groups (chronic hepatitis B [A1], chronic hepatitis C [B1], or cirrhosis [A1]).
2. For a new liver nodule ≥1 cm detected by surveillance tests in high-risk patients, multiphasic CT, or multiphasic MRI (extracellular contrast agents or hepatocyte-specific contrast agents) should be performed as a first-line imaging study for the diagnosis of HCC (A1). If first-line imaging study is inconclusive for the diagnosis of HCC, secondline imaging study including multiphasic CT, multiphasic MRI (extracellular contrast agents or hepatocyte-specific contrast agents), and contrast-enhanced US (blood-pool contrast agents or Kupffer cell-specific contrast agents) can be applied (B1).
3. Imaging diagnosis of “definite” HCC can be made for the nodule ≥1 cm detected by surveillance tests in high-risk patients based on the following radiological hallmarks: (1) the radiological hallmarks in multiphasic CT or MRI with extracellular contrast agents are APHE with washout appearance in the portal venous or delayed phases (A1). (2) The radiological hallmarks in multiphasic MRI with hepatocyte-specific contrast agents are APHE with washout appearance in the portal venous, delayed, or hepatobiliary phases; these criteria should be applied only to a lesion which does not show either marked T2 hyperintensity or targetoid appearances on diffusion-weighted images or contrast-enhanced images (B1). (3) The radiological hallmarks in contrast-enhanced US (blood-pool contrast agents or Kupffer cell-specific contrast agents) performed as a second-line imaging study are APHE with late (≥60 seconds) and mild washout or washout appearance in the Kupffer phase; these criteria should be applied only to a lesion which does not show either rim or peripheral globular enhancement on arterial phase (B1).
4. In nodules ≥1 cm that do not meet the radiologic diagnosis criteria of “definite” HCC, a diagnosis of “probable” HCC can be assigned by applying ancillary imaging features of HCC (B1). There are two categories of ancillary imaging features including imaging features favoring malignancy in general (mild-to-moderate T2 hyperintensity, restricted diffusion, threshold growth) and those favoring HCC in particular (enhancing or non-enhancing capsule, mosaic architecture, nodule-in-nodule appearance, fat or blood products in the mass). For nodules without APHE, “probable” HCC can be assigned only when the lesion fulfills at least one item from each of the two categories of ancillary imaging features. For nodules with APHE but without washout appearance, “probable” HCC can be assigned when the lesion fulfills at least one of the aforementioned ancillary imaging features.
5. For “probable” HCC, follow-up imaging study within 3 months or biopsy should be considered (C1). For “indeterminate” nodules that cannot be diagnosed as “definite” or “probable” HCC by imaging, follow-up imaging study within 6 months or biopsy should be considered (B1). Follow-up study should be performed using one of the first-line imaging modalities.
6. For subcentimeter nodules newly detected on HCC surveillance in high-risk patients, follow-up surveillance test within 6 months is recommended (C1).
7. Newly detected or growing nodules in the follow-up study of patients with a history of prior HCC can be diagnosed as recurrent HCC regardless of size if they show the radiological hallmarks of HCC or ancillary imaging features with an increase in size (C1).
8. Although it is not recommended to strictly limit the radiation dose for the diagnosis and follow-up evaluation of HCC, unnecessary CT examinations should be avoided. To optimize radiation exposure, the use of dose reduction techniques as well as alternative imaging modalities should to be considered in HCC patients (C1).
STAGING
Cancer staging plays a pivotal role in predicting the prognosis as well as in selecting the treatment modality to maximize survival. It also facilitates the exchange of information and trial design. Since HCC mostly develops in patients with cirrhosis or chronic liver disease, not only the tumor burden but also the underlying liver function affects prognosis [204,205]. In the treatment of HCC, liver function is an important factor influencing the OS [206]. Therefore, an ideal HCC staging should include both tumor staging and liver function, which makes it complicated. This is the reason why although several staging systems for HCC have been devised, there is still no global consensus [207].
The American Joint Committee on Cancer (AJCC) has led a collaborative effort with the Union for International Cancer Control (UICC) to maintain a cancer staging system (https://www.uicc.org/resources/tnm). This system classifies the extent of disease mostly based on anatomic information regarding the primary tumor, regional lymph nodes, and distant metastases (i.e., tumor-node-metastasis [TNM] staging system), and has been modified repeatedly. The 8th edition was proposed in 2017. Compared to the 7th edition, the 8th edition was revised to classify tumors less than 2 cm as T1a regardless of the presence of microvascular invasion, and T4 if there is an invasion of the portal vein or major branches of the hepatic vein. However, recent studies have shown that prognosis is not well-reflected in the 8th edition, as the presence of vascular invasion in tumors less than 2 cm was not considered [208,209]; therefore, further validation studies are warranted for the 8th edition. The KLCA-NCC guidelines had adopted the 5th version of the modified UICC (mUICC) staging system as a primary staging system for HCC in 2003 [210,211]. Thus, the continued use of this staging system may facilitate consistency in the analyses of registry data (Table 5). A recent Korean study reported that the mUICC staging system better reflects the OS and disease-free survival (DFS) compared to the AJCC staging system [212]. However, the mUICC staging system lacks international validation and has limitations, such as difficulty in the exchange of extensive information internationally, since it differs from the AJCC/UICC TNM staging system. In addition, the revised mUICC staging system [211] has defined biliary tract invasion and vascular involvement as same stages. However, the reason for this is unclear, and biliary tract invasion is different from vascular invasion in terms of the indication for surgery and prognosis following treatment; therefore, further research to validate this guideline is necessary. For the staging of HCC, chest CT, bone scan, positron emission tomography (PET) CT scans may be required in addition to dynamic CT or MRI of the primary liver tumor. The risk of distant metastasis is low for patients with early-stage HCC; therefore, tests for the evaluation of extrahepatic metastasis should be carefully selected. Gastroscopic examination is also required to confirm the presence of portal hypertension, which is important in the treatment decision process.
The Barcelona Clinic Liver Cancer (BCLC) staging system, which includes factors related to tumor stage, liver function, and performance status of the patient, was last updated in 2022 [213]. Preserved liver function status was defined as Child-Pugh grade A and the absence of ascites. It suggests the most recommendable treatment modality for each stage, and is endorsed by the American Association for the Study of Liver Diseases (AASLD), the European Association for the Study of the Liver (EASL), and the European Organization for Research and Treatment of Cancer (EORTC). However, the use of the BCLC staging system is limited in a way as it contains a subjective component (i.e., performance status), crude evaluation of liver function (i.e., Child-Pugh class), and unduly simplified recommendations for treatment modality [127,214]. The Hong Kong Liver Cancer (HKLC) staging system was developed for Asian patients, most of whom were diagnosed with hepatitis B. Patients with intermediate or advanced stage disease according to the BCLC staging system were more likely to undergo more active treatment than the BCLC staging system, and the survival rate was increased when the patients followed the HKLC staging system [215]. In a follow-up study, validation was performed by changing the 9-stage system to a 5-stage system. However, further validation is required for non-Asian populations and liver cancer from other causes [216].
The evaluation of extrahepatic metastasis is critical for the accurate determination of cancer stage and treatment strategy. Common sites of HCC metastasis include the lung, lymph nodes, bone, adrenal gland, and peritoneum [217]. However, the indications and methods to detect these metastatic lesions have not yet been established. The recently revised National Comprehensive Cancer Network (NCCN) guidelines recommend chest CT and CT or MRI of the pelvis as routine staging workups, and bone scan and/or specific bone imaging in those with bone pain or suspicion of bone metastases on cross-sectional images [218]. Several meta-analyses and retrospective studies have found that 18F-fluorodeoxyglucose (FDG) PET-CT was useful in detecting extrahepatic metastasis in patients with HCC [219-221]. In a prospective Korean study including 35 metastatic HCC patients, the sensitivity of FDG PET-CT for extrahepatic HCC lesions was reported to be 85.7% [219]. In particular, the detection rates of lung and bone metastases, which were the most common types of HCC metastases, were 80% and 100%, respectively. Another Korean study also demonstrated that 5% of BCLC stage A (six of 119) and 1.4% of BCLC stage B (one of 71) HCC patients were shifted to BCLC stage C after identifying extrahepatic lesions using FDG PET-CT [222]. An U.S. cohort study of 101 treatment-naïve patients reported changes of BCLC staging and treatment strategy in 5.9% and 9.9%, respectively, of the patients by adding FDG PET-CT after initial staging with contrast-enhanced CT or MRI [223]. Also, dual tracer PET-CT (18F-fluorocholine and FDG PET-CT) detected new lesions in 26 patients (21%), updated the BCLC stage in 14 (11%), and modified treatment strategy in 17 (14%), compared to conventional imaging alone, in a retrospective cohort of 122 HCC patients from France [224]. Hence, FDG PET-CT may be selectively considered for patients with HCC prior to curative surgical treatments, such as hepatic resection and LT.
[Recommendations]
1. This guideline adopts the mUICC stages as the primary staging system, with the BCLC staging system and the AJCC/UICC TNM staging system serving as complementary systems (B1).
2. FDG PET-CT can be utilized for staging prior to treatments with curative intent, such as hepatic resection or LT (C1).
3. Chest CT, pelvis CT, and bone scan can be used for HCC staging workup if extrahepatic metastasis of HCC is suspected (C1).
TREATMENT OVERVIEW
The goal of HCC treatment may vary according to the stage of cancer, underlying liver function, and performance status of the patient. However, the ultimate goal is to increase the OS and improve the quality of life. In order to achieve this, establishing multidisciplinary treatment plans by various experts, including hepatologist, gastroenterologist, surgeon, radiologist, interventional radiologist, oncologist, radiation oncologist, pathologist, and other related medical practitioners is necessary [225]. It would be effective to make personalized treatment plans based on the opinions of relevant experts as there is a wide range of treatment options available for HCC, including hepatic resection, LT, locoregional ablative therapies, transarterial therapies, external-beam radiation therapy, and systemic therapies. Furthermore, unlike other types of cancer, HCC often develops in the presence of underlying liver cirrhosis and its complications may occur during cancer treatment [218,226]. Although there has been no large-scale prospective study on the effectiveness of multidisciplinary approach in patients with HCC conducted to date, a number of retrospective studies have consistently reported improvements in the early diagnosis rates, the likelihood of patients actively receiving cancer treatments, and the OS [227-231]. In subgroup analyses, significant improvements in OS were particularly observed in difficult-to-treat cases, such as patients with liver dysfunction, and intermediate or advanced HCCs [227,228]. These results may indicate that multidisciplinary approaches allow medical specialists from different fields to actively communicate with one another, share patient’s clinical information without delay, and apply the latest treatment strategies, including clinical trials. Therefore, a multidisciplinary approach may play a key role in improving patient satisfaction, reducing tumor progression, and prolonging patient survival [229,232-238]. Multidisciplinary approaches for HCC began developing in the early 2000s, but there are still no clear guidelines regarding the optimal frequency, format, and management, including necessary expenses. In addition, more evidence is still required on clinical outcomes and cost-effectiveness. Prospective studies are needed for the precise assessment of clinical benefits and to establish detailed guidelines on multidisciplinary approach in HCC patients.
The choice of treatment method should be as evidence-based as possible, and the best evidence is a meta-analysis targeting RCTs or prospective controlled studies, and prospective large-scale cohort studies to confirm survival. Although these studies are gradually increasing, the best evidence such as RCT for the treatment of HCC is still lacking, so much of the treatment plan is based on moderate evidence. Therefore, much understanding and attention are needed in the treatment application. It is difficult to establish a balanced multidisciplinary treatment plan in clinical practice because there is a lack of objectivity in the treatment indications and results claimed by each department that directly performs patient treatment, so a more objective evaluation is needed through collective discussion by expert groups such as this guideline revision committee.
The best treatments recommended in this guideline are the results of evidence-based medicine. Prerequisites to adequately apply these recommendations include actual facilities and trained personnel to provide all possible treatments for the patients, as well as the financial condition of patients and cooperation from patients and guardians. Therefore, considering the various aforementioned requirements, these guidelines first provided both the best and alternative treatments for each mUICC staging in 2014, and the same manner is used in the revised guidelines (Fig. 8). However, as different treatments may be selected for HCC depending on the underlying liver function, performance status, and symptoms in addition to staging, not all possible cases could be listed and summarized in the guidelines. Recommendations for specific treatments are made based on medical evidence and expert opinions for various HCC conditions, and they are described in detail in each treatment section of these guidelines.
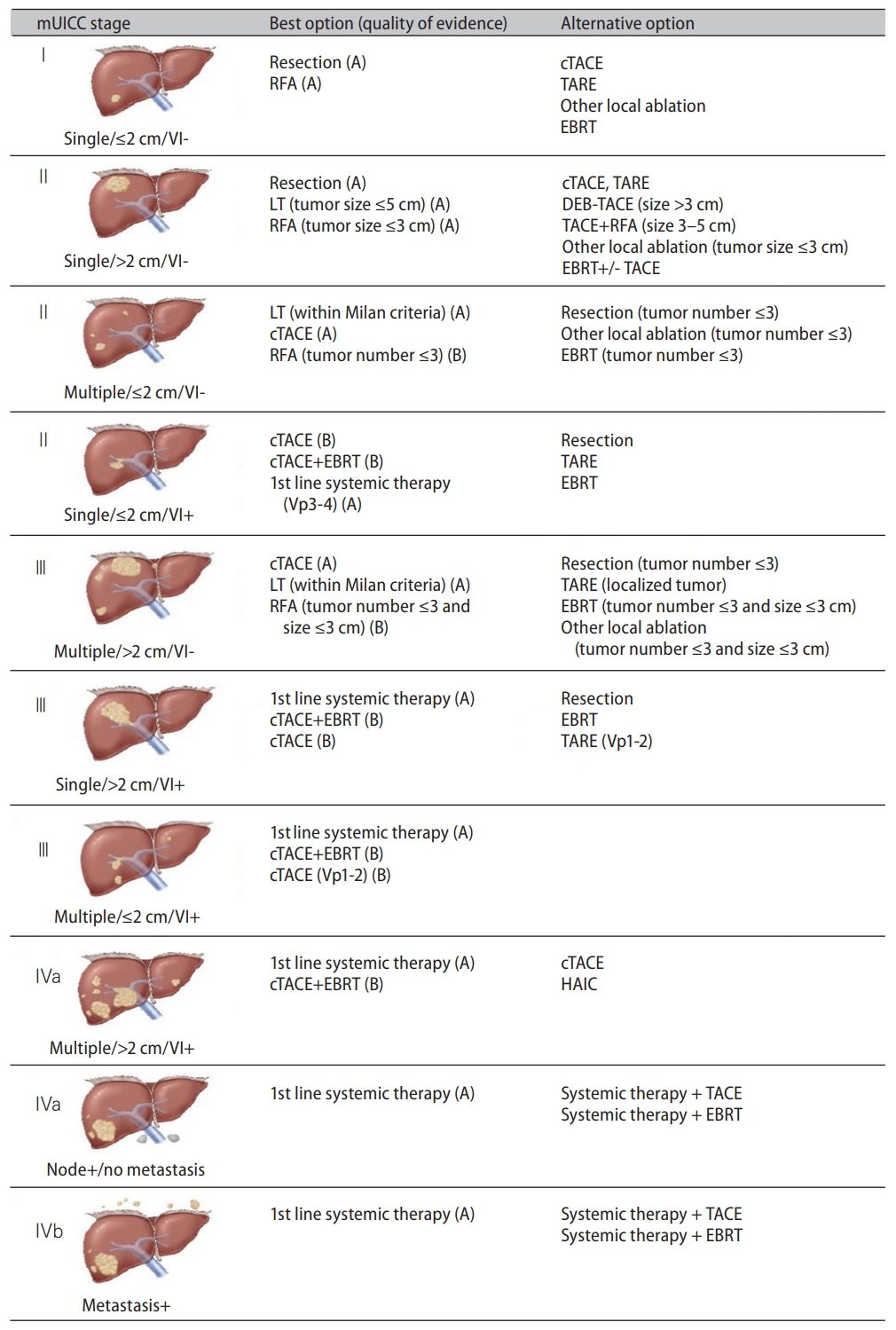
First-line treatment of 2022 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for patients with hepatocellular carcinoma, Child-Pugh class A, no portal hypertension, and Eastern Cooperative Oncology Group performance status 0–1. mUICC, modified Union for International Cancer Control; VI, vascular or bile duct invasion; RFA, radiofrequency ablation; cTACE, conventional transarterial chemoembolization; TARE, transarterial radioembolization; Other local ablation, percutaneous ethanol injection (PEI), microwave ablation (MWA), and cryoablation; EBRT, external beam radiation therapy; Vp, portal vein invasion; LT, liver transplantation; DEB-TACE, drug eluting bead-TACE; TACE, cTACE and DEB-TACE; HAIC, hepatic arterial infusion chemotherapy.
This overview summarizes the treatments for HCC patients with various mUICC disease stages with good liver function (Child-Pugh A level) and good performance status (Eastern Cooperative Oncology Group [ECOG] performance 0–1) without any complications of portal hypertension to promote understanding of treatments in general. These guidelines have separately dealt with second-line treatment for the first time, but this management overview provides information only on the initial treatment. Second-line treatments for residual, recurred, or progressed cancer after the initial treatment are later described separately, along with the recommendations.
HEPATIC RESECTION
Hepatic resection is not only a primary treatment modality for patients with solitary HCC unaccompanied by liver cirrhosis [239], but also a preferentially considered option for cirrhotic patients with sufficient hepatic functional reserve [240,241]. The outcomes of hepatic resection for HCC have markedly improved following recent advances in preoperative tests and surgical skills, as well as the accumulation of experience in postoperative management [242]. Recent studies have shown that postoperative mortality after HCC resection is less than 1–3%. In addition, the 5-year OS and DFS rates are 46% to 69.5% and 23% to 56.3%, respectively [243-246]. The 5-year recurrence rate after hepatic resection of HCC ranges from 43.7% to 77%, and about 80% to 95% of postoperative recurrences are intrahepatic [247]. Intrahepatic recurrences are divided into intrahepatic metastasis and de novo HCC by multicentric carcinogenesis. The two recurrence entities can be differentiated by the means of genomic hybridization, DNA fingerprinting, DNA microarray, or HBV integration pattern [248]. However, no clinical definition of either entity has been established. In general, late recurrence more than 2 years after primary resection is considered as a de novo HCC [249]. Risk factors associated with recurrence after resection are classified as either tumor-related or underlying disease-related. Tumor-related factors, which are usually related to early recurrence, include the tumor size and number, microvascular invasion, poor tumor differentiation, high serum AFP and prothrombin induced by vitamin K absence II (PIVKA-II) levels, and positivity of 18F-FDG PET. Meanwhile, underlying disease-related risk factors, which influence late recurrence, include cirrhosis, high serum HBV DNA levels, and active hepatitis [219,249-255]. Nevertheless, no association between risk factors and timing of recurrence is evident in many cases, since this time-dependent classification does not actually reflect the tumor-pathologic mechanism of HCC recurrence.
Imaging modalities, such as CT and MRI, as well as serum tumor markers, are the recommended surveillance tools during follow-up. Serum AFP, a traditional tumor marker of HCC, is also an effective marker for recurrence when liver function is normalized after resection in cases with preoperatively elevated AFP levels [256]. PIVKA-II is another HCC marker with increasing utility for diagnosis, follow-up, and prognostication of HCC [250, 257].
Preoperative evaluation
Child-Pugh classification is conventionally used to preoperatively assess the safety of hepatic resection (Table 6) [258]. Hepatic resection is commonly performed in patients with Child-Pugh class A with ECOG performance status 0–2 (Table 7).
However, Child-Pugh classification is an insufficient preoperative indicator of operability as many patients’ liver function can remain in Child-Pugh class A despite advanced cirrhosis [259,260]. Therefore, the indocyanine green 15-minute retention rate (ICG-R15), which was suggested for use in Japan, is utilized at many Korean institutions as a preoperative test for the prediction of residual liver function [261].
Although major hepatic resection is recommended only for patients with ICG-R15 ≤10%, a recent study reported safe right hemihepatectomy even in patients with an ICG-R15 of up to 14% [262]. In contrast, portal hypertension and serum bilirubin level have been suggested as the criteria to determine resectability in Europe and the United States, in which portal hypertension is defined as a hepatic venous pressure gradient ≥10 mmHg [263].
Esophageal varix and thrombocytopenia <100,000/mm3 accompanied by splenomegaly and ascites are also indicators of portal hypertension, and thrombocytopenia is considered the most clinically relevant criterion.
In patients with portal hypertension, the post-hepatectomy complication rate is high and long-term prognosis is poor [263-265] However, some recent studies reported comparable outcomes even in patients with portal hypertension [266-269].
Minor hepatic resection instead of major hepatic resection should be considered in patients with mild portal hypertension, as resection volume is closely associated with the risk of postoperative hepatic insufficiency. HCC is usually accompanied by chronic liver disease in most cases. In order to predict postoperative hepatic insufficiency, the assessment of future liver volume or remnant liver volume after resection is as important as the hepatic reservoir function test. Although 70% to 80% of the volume can be resected in healthy liver, a much lower resection volume is allowed for diseased or cirrhotic liver. There have been few studies about the safe remnant liver volume in patients with cirrhosis. Nevertheless, a remnant liver volume ≥40% is generally recommended in cirrhotic patients for safety [270]. Recently, several noninvasive tests to measure the severity of hepatic fibrosis have been developed. Among them, liver stiffness measurement (LSM) with transient elastography was recently reported to be effective for predicting postoperative hepatic failure and recurrence [271-274]. The optimal LSM cut-off value varies according to background liver condition and measurement methods [271,274-277]. Recently, a meta-analysis study and the EASL guidelines reported that significant risk of posthepatectomy liver failure can be predicted by liver stiffness above 11.3–14.2 kPa and 12–14 kPa, respectively [278].
Dynamic contrast-enhanced CT is the basic test utilized as a preoperative radiologic study to assess the possibility of resection. MRI using a hepatic cell-specific contrast medium is superior to CT for HCC detection, especially for small HCCs <1 cm [279,280], and may be a useful method to assess resectability and to formulate resection plans. Gadolinium-EOB-DTPA MRI was also proposed for the evaluation of liver function, like ICG-R15. Several studies reported that it could be used as a novel tool to assess or monitor liver function during perioperative period [281-284].
Further examinations may be necessary to find extrahepatic metastases before hepatic resection in patients with HCC. 18F-FDG PET-CT may be effective for investigating extrahepatic metastasis [285], although its sensitivity is very low for the diagnosis of intrahepatic HCC [219]. In addition, chest CT and bone scan may also be helpful [286].
Basic principles of hepatic resection
One reason why hepatic resection has recently become safer is the reduction in the amount of intraoperative hemorrhage, which minimizes the amount of transfusion required. Blood transfusion has been reported to compromise anticancer immunologic mechanisms and increase postoperative recurrence [287]. However, a recent meta-analysis study reported that intraoperative or postoperative blood transfusion was not associated with DFS [288,289]. Recent transfusion rates in hepatic resection are ≤10% owing to selective hepatic blood flow occlusion, maintenance of low central venous pressure, and precise transection of the hepatic parenchyma [290]. However, a recent prospective randomized study reported that goal-directed fluid therapy based on the stroke volume was sufficient to minimize bleeding, without the need to unconditionally lower the central venous pressure during surgery [291]. In addition, although the Pringle’s maneuver is a useful method for lowering intraoperative bleeding, caution is still required as a meta-analysis reported that it may increase early recurrence [292,293].
The debate regarding anatomical and non-anatomical HCC resection continues. Several retrospective studies [294-299] and a meta-analysis [300] suggested that anatomical resection may be superior to non-anatomical resection in terms of securing the resection margin and removing micro-metastases. A recent prospective randomized trial showed that anatomical resection decreased the early recurrence rate within 2 years after hepatic resection, but did not affect 5-year DFS or OS [301]. In two recent meta-analysis studies, anatomical resection showed no difference in surgical complications compared to non-anatomical resection, while showing superior results in DFS and OS [302-304]. Therefore, it is desirable to consider anatomical resection, if possible, for HCC resection.
Securing a tumor-free resection margin is critical to improve long-term prognosis. One prospective randomized trial showed that a resection margin >2 cm led to better outcomes after HCC resection [305]. However, according to recent meta-analyses, it was reported that a resection margin of 1 cm or more is sufficient [306,307]. Therefore as excessive hepatic resection is closely associated with complications in patients with cirrhosis, determining the appropriate extent of resection with patient safety as the top priority is important although a sufficient margin from the tumor and anatomical resection are recommended [308-310].
Transarterial chemoembolization (TACE), performed before hepatic resection for the purpose of improving postoperative prognosis, is not recommended [311-313]. Patients with liver cirrhosis need more sufficient remnant liver volume than patients with normal liver, since the remnant liver volume after hepatic resection is an important prognostic factor for hepatic insufficiency [314,315]. When insufficient remnant liver volume is expected, portal vein embolization before hepatic resection or portal vein ligation during hepatic resection may enable extensive hepatic resection by inducing compensatory hypertrophy of the residual liver [316-318]. Recently, resection using Associated Liver Partition and Portal vein Ligation for Staged hepatectomy (ALPPS) has been reported for cases of insufficient remnant liver volume even in HCC patients, but it has not been universalized yet [319].
The hanging maneuver is frequently used during hepatic resection, although there is no report on its effect on survival or recurrence after HCC resection. Nevertheless, the hanging maneuver can shorten surgical time and reduce the amount of bleeding [320]. The anterior approach, which is often used for the resection of large tumors, is associated with less bleeding, a lower transfusion rate, and better survival, according to a meta-analysis [321].
Minimally invasive hepatic resection
Techniques of laparoscopic liver resection (LLR) have evolved rapidly, and its indications have extended. LLR can be applied for HCC located in the posterosuperior segments and caudate lobe as well as in the left lateral section and anterolateral segments. Compared to open liver resection (OLR), LLR has led to less postoperative pain, complications, and shorter postoperative hospital stays although the overall recurrence rate and survival rate were not significantly different between the two groups [322-324].
With the development of laparoscopic techniques and surgical instruments, especially laparoscopic imaging system (4K, 3D, and indocyanine green fluorescence images), major hepatectomy, hepatectomy for recurrent HCC, hepatectomy for HCC in patients with liver dysfunction have also gradually increased [325-327]. A recent study showed that compared to OLR, LLR for patients with Child-Pugh B7 cirrhosis or portal hypertension was associated with less perioperative bleeding, postoperative pain, complications, and shorter postoperative hospital stays. However, the overall recurrence rate and survival rate were not significantly different between the two groups [328-330].
Techniques of robotic liver resection has also evolved, and its indications have extended. However, robotic liver resection for HCC is still performed only in highly experienced centers, and further comparative studies with OLR and LLR should be performed in the near future [331].
Indication of hepatic resection
In general, hepatic resection shows a good prognosis when performed for one or two tumors of small sizes. As the size of the tumor increases, the frequency of vascular invasion also increases which leads to poor prognosis. However, according to recent studies, microvascular invasion was not observed in about one-third of patients with tumors sized more than 10 cm, and surgical treatment showed better results compared to non-surgical treatment even in those patients [332-334]. Accordingly, hepatic resection can be favorably considered when operable in patients with a large sized tumor. For multiple tumors, surgical treatment may be limited in its indication. As recent reports have shown that liver resection was more effective than non-surgical treatment for ≤3 tumors [335-337], hepatic resection can be considered even for multiple liver tumors that are ≤3 in number and not indicated for LT. With the development of surgical techniques and improvement in patient management, even elderly patients have shown similar short-term and long-term results after hepatic resection as in other age groups, whereas major hepatic resection should still be performed with caution due to the decreased regenerative capacity of the liver in elderly patients [338-340].
Although the long-term outcome of ruptured HCC is inferior to that of unruptured HCC [341-343], patients who received hepatic resection after emergency transarterial embolization for hemostasis revealed better survival rates compared to those who only underwent TACE [344]. Although primary hepatic resection was performed effectively in patients with good liver function in some reports [345,346] it is more safe and effective, when the patient is hemodynamically unstable, to perform transarterial embolization first followed by elective surgery after an accurate evaluation of residual liver function [347,348].
Generally, tumor invasion to the major hepatic veins or major portal veins has been considered as a contraindication of hepatic resection. However, recent retrospective studies have shown that the OS of hepatic resection was better than that of non-surgical treatment modalities, such as TACE, radiation therapy, or sorafenib, unless the main portal trunk or contralateral branch was involved [349-354]. In addition, according to a Korean multicenter study and a Korea-Japan joint study, the 5-year survival rate after hepatic resection for HCC with bile duct invasion was 32.0–43.6%, which was fairly appreciable, and aggressive hepatic resection including bile duct resection was helpful to improve survival [355,356]. Therefore, even for HCC that has invaded blood vessels or bile ducts, hepatic resection can be selectively considered if the patient’s general condition is tolerable.
[Recommendations]
1. Hepatic resection is the primary treatment modality for single HCC limited to the liver in Child-Pugh grade A patients without portal hypertension and hyperbilirubinemia (A1).
2. Limited hepatic resection can be selectively performed for Child-Pugh A or B7 single HCC with mild portal hypertension or hyperbilirubinemia (C1).
3. Hepatic resection may be considered even in the cases of HCC with invasion to the portal vein, hepatic vein, or bile duct if the main portal trunk is not invaded in patients with well-preserved liver function (C2).
4. Hepatic resection may be considered for three or less multiple HCCs in patients with well-preserved liver function (C2).
5. LLR for HCC located in the left lateral section and anterolateral segments can be selectively performed (B2).
6. LLR for HCC located in the posterosuperior segments or caudate lobe can be selectively performed depending on the location and size of the tumor (C2).
Treatment of intrahepatic metastasis after hepatic resection
The rate of postoperative recurrence with intrahepatic metastasis owing to local dissemination or de novo carcinogenesis is about 50–60% at 5 years after hepatic resection [296,357]. Recurrence of the tumor with intrahepatic metastasis usually presents as multiple intrahepatic recurrences. In such cases, it is often impossible to repeat curative treatment, and the risk of recurrence after treatment is high [358]. In contrast, de novo recurrence can be the target of curative re-operation or local treatment [249,263,359-363]. Typically, recurrence within 2 years after surgery is classified as early recurrence, and recurrence after 2 years is classified as late recurrence. The risk factors for recurrence can be divided into tumor-related factors and underlying liver disease-related factors. Tumor-related risk factors include the tumor size, number, degree of differentiation, vascular involvement, serum AFP level (elevated before surgery), serum PIVKA-II level, lack of adequate resection margin, and non-anatomical resection, which are mainly associated with early recurrence [249,253,362-368]. The risk factors related to underlying liver disease are high serum HBV DNA levels before and after surgery for chronic hepatitis B [254,369-371] and persistent active inflammation and degree of hepatic fibrosis for chronic hepatitis C [371,372]; these are associated with late recurrence. In a randomized prospective study of repeated hepatic resection and RFA for intrahepatic recurrence, no statistically significant differences were found in the 5-year DFS and OS between the repeated hepatic resection group and the RFA group (36.2% and 43.6% in the repeat hepatic resection group vs. 30.2% and 38.5% in the RFA group, respectively). In this study, RFA had a higher early recurrence rate compared to repeated hepatic resection. In subgroup analysis, the survival rate of repeat hepatic resection was statistically higher than that of RFA when the tumor size was 3 cm or more and AFP was 200 ng/mL or higher. According to previous retrospective studies, the incidence of complications after repeated hepatic resection was higher than that of RFA [247,364,373]. Salvage LT for recurrent intrahepatic HCC after hepatic resection requires a cautious approach [374]. If intrahepatic recurrence after hepatic resection does not progress after locoregional therapies, such as RFA, TACE, or radiation therapy, salvage LT is the most effective treatment to increase the DFS and OS rates compared to repeated hepatic resection or other local treatments. Salvage LT should be determined by carefully considering the shortage of liver grafts from deceased donors or the problems related to living donors [359,375]. However, the patients who undergo repeated resection are limited in clinical practice, since they have small residual liver parenchyma after resection and are at risk of additional recurrence [376]. For recurrent HCC which is not indicated for repeated hepatic resection, non-surgical local treatments, such as RFA and TACE, can be applied. RFA has been extensively performed as a minimally invasive treatment for small relapsing HCCs [360,377]. TACE is the most widely used treatment for multiple HCC recurrences [378-380]. The meta-analysis that compared the effects of each of the above-mentioned treatments revealed that there was no difference in survival benefit among the treatment modalities for recurrent tumors after surgery. Therefore, appropriate treatment option should be selected considering the remnant liver function, the location and the number of recurrent tumors [377].
[Recommendations]
1. For recurrent HCC after being cured by hepatic resection, the retreatment method can be selected considering the timing of recurrence, remnant liver function, performance status, and the size, location, number of recurrent tumors (C1).
LIVER TRANSPLANTATION
LT is the treatment of choice for HCC within Milan criteria (a single tumor ≤5 cm or small multinodular tumors [≤3 nodules, ≤3 cm]), if unsuitable for resection. LT involves the complete removal of a diseased liver, including HCC, and replacement with a new liver. Theoretically, it is the ideal and the most effective treatment method providing excellent and unparallel long-term survival outcomes. However, there are limitations in its application due to insufficient deceased organ donation and living donor liver transplantation (LDLT) is currently the main type of LT for HCC in South Korea.
The Milan Group in Italy reported an excellent result (i.e., a 4-year survival rate of 75% and a DFS rate of 83%) after LT in HCC patients with the following conditions: (1) no extrahepatic metastasis and no vascular infiltration in the radiologic study before transplantation; (2) a single nodule of 5 cm or less; and (3) three or fewer nodules in cases with multiple nodules and each nodule being 3 cm or less [381]. Since then, the Milan criteria have been widely used for LT in patients with HCC. A recent systematic review of 90 studies, comprising a total of 17,780 patients over 15 years, identified the Milan criteria as an independent prognostic factor for a favorable outcome after LT. The overall 5-year survival of patients meeting the Milan criteria (65% to 78%) was similar to that of non-HCC patients, according to the European and American transplant registries [382,383].
Recent advances in imaging technologies have enabled non-invasive diagnosis of HCC with higher accuracy. However, small lesions, which could not be detected with imaging studies at the time of the establishment of the Milan criteria, can be detected on imaging studies with current technologies, and can cause confusion regarding whether or not a patient meets the Milan criteria. A recent meta-analysis including 22,392 patients concluded that the size of the largest tumor and the total diameter of nodules were the best predictors of outcome, while number of tumors was not associated with the outcome of LT [384]. Sugimachi et al. [385] also reported poor diagnostic accuracy of imaging for small (<1 cm) HCCs and the limited effect of preoperatively unobserved tumors on prognosis after LT. Therefore, lesions ≤10 mm or with atypical findings should not be used to decide for or against transplantation.
Before transplantation, HCC patients undergo tests for staging in addition to general whole-body examination. In addition to dynamic contrast enhancement CT or MRI, extrahepatic staging should include CT of the chest, and CT or MRI of the abdomen and pelvis. Imaging of the brain, bone scintigraphy, and 18F-FDG PET-CT may be performed [386]. 18F-FDG PET-CT can help characterizing the biology of HCC, since PETpositive tumors more frequently display unfavorable histological features (e.g., high cellular dedifferentiation and microvascular invasion) [387], resulting in poorer recurrence-free survival (RFS) after LT [388,389]. There has been no specific study nor consensus on the optimal timing or modality for evaluation of patients on the waiting list to monitor whether they remain within the acceptability criteria for LT, although dynamic CT or MRI and AFP measurement at a 3-month interval is commonly used [383].
Deceased donor LT
Although LT is a very effective treatment for HCC, the risk of waiting-list mortality is very high due to the gap between the demand and supply in deceased organ donation regardless of underlying liver disease. Especially in South Korea, the risk of dropping out from the waiting list due to tumor progression is very high owing to the low rate of deceased organ donation. Many countries have developed their own organ allocation systems according to their donation situations. Each system tried to balance the risk of drop-out between HCC and non-HCC patients, and developed various rules of bonus points for HCC patients [390,391]. The National Institute of Organ, Tissue, and Blood Management operates the Korean Network for Organ Sharing (KONOS), has adopted the model for end-stage liver disease (MELD) score in June 2016. When fulfilling the Milan criteria, patients with a MELD score of 0 to 13 receive an additional 4 points; patients with a MELD score of 14 to 20 also receive an additional 5 points, while those with a MELD score of 21 or higher do not. Nevertheless, deceased donor liver transplantation (DDLT) in South Korea is mostly performed when the MELD score is above 30, and it is very unlikely that a graft liver from a deceased donor is to be allocated to an HCC patient without underlying decompensated liver disease. The annual case number of DDLT in South Korea reached its peaked in 2016 at 508 cases; and since then, it has decreased to 391 cases in 2019 [392]. Such decrease in the deceased organ donation rate and relative disadvantage in organ allocation to HCC patients have led the proportion of HCC patients to account for only 2–5% of the total DDLT cases in South Korea [392].
Bridging and downstaging therapy
The dropout rate at which LT becomes infeasible due to tumor progression while waiting for LT is reported to be 15–30% per year [393,394], and bridging therapy using loco-regional therapy is reported to reduce the dropout rate to 0–25% [395-397]. However, these figures are based on Western studies, and may not be applicable to South Korea. A recent report showed promising results after LT when the waiting period prior to LT was within 6 to 18 months in HCC patients [398]. Since the possibility of HCC progression is high when the waiting period for transplantation is prolonged, HCC treatment prior to transplantation is recommended if the waiting period for transplantation of more than 6 months is expected [395,398,399].
Many studies have been conducted on the effects of pretransplant HCC treatments on the outcomes of LT; and so far, many studies have reported that treatment using loco-regional therapy in patients within the Milan criteria is not related to a reduction in recurrence of HCC after LT and an increase in the survival rate [368,400-405]. However, a recent study using Organ Procurement and TransplantationNetwork (OPTN)/Scientific Registry of Transplant Recipients (SRTR) in the United States showed that patients who received locoregional therapy before LT had higher survival rates than those who did not, and that the longer the waiting period for transplantation, the higher the survival rate after transplantation [406]. Therefore, further research is needed.
Loco-regional therapies, including TACE, RFA, and stereotactic radiotherapy, along with hepatic resection are generally used to treat patients before transplantation [395,396,407-410], and they are implemented not only to reduce the dropout rate due to tumor progression during the waiting period but also for downstaging after planning LT in HCC patients who are not initially indicated for LT.
The most commonly used loco-regional therapy for HCC prior to LT is TACE, which can downgrade the stage of HCC by 24–63% [406,411,412]. Downstaging is known to be more effective when the tumor size is smaller than 7 cm or there are less than three tumors [22], but there are no restrictions [413]. No difference has been reported on the outcomes of LT following transarterial radioembolization (TARE) using Yttrium-90 (90Y) and conventional TACE (cTACE) for downstaging [414-416]; however, further research is required.
There has been no large-scale prospective study on the outcomes of patients who initially did not meet the indications for LT but were downstaged to meet the Milan or University of California San Francisco (UCSF) criteria using loco-regional therapy for the purpose of LT. However, an Italian group recently conducted a RCT of 45 patients with HCC who effectively downgraded their stage to meet the Milan criteria through loco-regional therapy, and the patients who received LT after downstaging showed significantly higher DFS and OS rates compared to the patients who did not undergo LT [417]. In addition, several previous small-scale prospective studies have shown that in patients outside the Milan or UCSF criteria, their 5-year survival rate were similar to that of patients within the Milan or UCSF criteria when successful downstaging had been achieved to meet the Milan or UCSF criteria using loco-regional therapy prior to LT [405,409,418-421]. Therefore, when patients with HCC outside the Milan criteria, who are not indicated for LT, show therapeutic response to loco-regional therapies including TACE, RFA, and stereotactic radiotherapy to meet the Milan criteria, LT is recommended.
In patients with HCC outside of the Milan criteria that deviates from indication for LT, stage reduction was successfully acquired in more than 40% but recurred in 16% after LT, and in other reports, more than 80% of them were transplanted with successful stage reduction. Evaluating the therapeutic response of loco-regional therapy before transplantation can be used to select subjects for LT in patients with HCC outside the Milan criteria [415,416,422]. In evaluating the prognosis after LT, not only the pathological findings of the extracted liver tissue but also the changes in biological indicators, such as levels of tumor markers, are used [422,423]. In recently conducted studies, the recurrence rate of HCC after LT was low when a complete remission by loco-regional therapy was identified in the extracted liver tissue [368,423,424]. Also, the DFS and OS rates were higher in patients with a significant decrease in the levels of tumor markers after loco-regional therapy compared to those without [425,426].
Living donor LT
The number of DDLTs are increasing in South Korea recently due to changes in the society’s perception on organ donation and the revision of laws to promote organ donation [427,428]. However, LDLT is still the main type of LT in South Korea due to a shortage of deceased donor organs in the country. In 2019, there were 1,579 cases of LT, including 1,188 LDLTs (75.2%) and 391 DDLTs (24.8%), in South Korea [429]. Following the revision of the allocation system on DDLT, the number of deceased donors has increased for a few years but is recently on the decrease again. Therefore, the number of people on the waiting list for DDLT had decreased from 6,334 in 2013 to 4,969 in 2016 but increased to 5,734 in 2020.
According to the KONOS regulation for registration and allocation in South Korea, recipient candidates with HCC can gain a higher priority on the waiting list. However, in real clinical settings, patients with HCC in South Korea have a very low chance of receiving DDLT since most deceased donor livers are allocated to patients with a high MELD score (>30). These findings suggest that currently DDLT is not a feasible treatment modality for HCC patients in South Korea. Therefore, LDLT from a healthy donor has emerged as an alternative to DDLT as a treatment modality for HCC and a significant proportion of the LT recipients with HCC have received transplantations from living donors in South Korea. The comparative outcome of LDLT versus DDLT for patients with HCC is controversial. A meta-analysis of 633 LDLTs and 1,232 DDLTs indicated that LDLT is an acceptable option without compromising the survival rates [430]. However, the DFS was worse with LDLT than with DDLT [430]. Another meta-analysis of 1,310 patients who underwent LDLT and DDLT for HCC showed no difference in the OS and DFS [431]. A recent meta-analysis of 40,495 cases reported no statistically difference in the recurrence of HCC between LDLT and DDLT (17% vs. 14%, respectively) [432].
Patients undergoing LDLT have a short wait time and are unlikely to drop out, whereas a dropout rate of 5–30% is reported in DDLT patients. Given that an intention-to-treat (ITT) analysis includes patients who drops out of the waiting list, it is an ideal method for the comparison of LT outcomes according to the difference in donation patterns. In ITT analysis, there was no difference in the rates of OS and DFS between the two groups according to donation patterns [433,434]. The higher recurrence rates observed after LDLT in some reports is likely due to the differences in tumor characteristics, pretransplant HCC management, and wait time [435-437]. In order to compare the outcomes of LT for HCC according to the type of graft, well-designed studies are needed to reflect bias and the effects of tumor biology.
In the DDLT program, the selection criteria have been set to maximize the efficacy-efficiency of donor organs. In contrast to DDLT, the indications for LDLT in HCC patients are decided based on the balance between donor risks and recipient benefits. Several eligibility criteria besides the Milan criteria for LDLTs have been adopted by many high-volume LDLT centers. At Samsung Medical Center, patient selection according to tumor size <5 cm and AFP <400 ng/mL without limitation in the tumor number expanded patient selection; 1-, 3-, and 5-year survival rates were reported to be 92.2%, 82.6%, and 79.9%, respectively [438]. At Seoul National University Hospital, the 3-year survival rate was reported to be 86.2% if vascular invasion was absent in preoperative radiological studies and preoperative AFP was <400 ng/mL [439]. At Catholic Medical Center, LDLT was considered the preferred therapeutic option in patients with an AFP level <100 ng/mL and a tumor diameter <5 cm. The 5-year DFS and OS after LDLT were 80.9% and 76.4%, respectively [440]. At Asan Medical Center, patients with ≤6 HCCs each sized ≤5 cm and without gross vascular invasion were considered eligible for LT, and such patients had a 5-year survival rate of 81.6% [441]. In the selection of HCC patients for LT, the University of Tokyo has adopted the 5-5 rule, i.e., HCC ≤5 cm and ≤5 in number, and a RFS rate of 94% after LT was achieved [442]. Kyoto University further extended the number of tumors to 10 with serum PIVKA-II levels ≤400 mAU/mL; the resultant 5-year survival rate was 86.7% [443]. At Kyushu University, a 5-year survival rate of 82.7% was achieved in patients with HCCs ≤5 cm and serum PIVKA-II levels <300 mAU/mL [444]. In a study involving 49 centers and 653 patients in Japan, patients with HCCs beyond the Milan criteria but with serum AFP levels ≤200 ng/mL and serum PIVKA-II levels ≤100 mAU/mL had a 5-year DFS rate of 84.3% [445]. Most of these expanded criteria were made after modifying tumor size and number in the Milan criteria. However, the selection criteria have recently been amended to include biological markers, such as AFP and PIVKA-II [446]. Criteria based on tumor biology, including FDG-uptake, led to the accurate prediction of prognosis and risk factors in LT recipients with HCC [388,447-449]. European multicenter studies have shown that AFP-containing criteria better predict tumor recurrence after LT compared to criteria based on the number and size of tumors. There have been reports that even if patients with HCC exceed the Milan criteria, they can achieve good results when they fulfil the criteria including AFP [450-452]. LDLT has been proposed as an ideal setting for exploring expanded indications for HCC, considering the lack of graft allocation and priority policies for patients with HCC. Moreover, special personal relationship between the living donor and the recipient should be taken into account. Therefore, if the posttransplant outcomes of several eligible criteria beyond the Milan criteria for LDLTs are comparable to that of the Milan criteria, expanded indications can be accepted as long as the safety of the liver donor is ensured.
The safety of the liver donor is of paramount importance in the LDLT. The outcomes of living donors from South Korea are excellent [453-458]. According to the Korean Organ Transplantation Registry study including 832 living liver donors, major complication (including bile leakage, biliary stricture, portal vein stricture, wound dehiscence, and pulmonary edema) rates were 1.9%, and there was no mortality [459]. Recent literature reported similar outcomes and decrease in hospital stay and wound owing to the advance in laparoscopic surgery [460]. Robotic donor hepatectomy also reported good satisfaction for scar and recovery without increase in complication, establishing the safety and satisfaction of minimal invasive surgery [461]. However, in the early days of LDLT, the probabilities of death and life-threatening complications in healthy donors have been reported to be 0.2–0.3% and about 2% globally, respectively [458,462-465]. Recent long-term outcomes of 12,372 donors also reported higher mortality and disease prevalence in liver donors compared to the healthy control group (mortality rate 0.91 in 1,000 population) [466]. Due to the complexity of the procedure, LDLT must be restricted to centers of expertise in hepatic surgery and LT to minimize donor risk and maximize recipient outcome. Careful attention should be given to the psychosocial well-being of liver donors.
Immunosuppression after LT
Immunosuppressants, such as calcineurin inhibitors (cyclosporine, tacrolimus) and the mammalian target of rapamycin inhibitors (mTORi; sirolimus, everolimus), are used for patients with HCC after LT [467]. Recent studies have shown that the use of mTORi may be helpful for reducing recurrence and prolonging survival in HCC patients after LT, but further studies are needed [468-470]. Recent meta-analysis reported better outcomes in mTORi group than non-mTORi groups in the 5-year RFS rate (ratio, 1.13; 95% CI, 1.02–1.26 in RCT and ratio, 1.17; 95 CI, 1.10–1.24 in cohort study) [471]. Therefore, if there are no significant adverse events related to drugs, mTORi may be considered in LT recipients with HCC.
[Recommendations]
1. LT is the primary treatment modality for patients with HCC unsuitable for resection but within the Milan criteria (a single tumor ≤5 cm or small multinodular tumors [≤3 nodules, ≤3 cm]) (A1).
2. In LT candidates with HCC, loco-regional therapies or TACE are recommended if the timing of transplantation is unpredictable (B1).
3. If the HCC tumor stage is downgraded to meet the Milan criteria by loco-regional therapies, including TACE and RFA, in patients initially exceeding the Milan criteria, LT shows superior outcomes compared to other treatments (B1).
4. Expanded indications beyond the Milan criteria for LT may be considered in limited cases without definitive vascular invasion or extrahepatic spread if other effective treatment options are not applicable (C2).
5. Salvage transplantation can be indicated for recurrent HCC after resection according to the same criteria as for first-line transplantation (B1).
Treatment of intrahepatic recurrence after LT
LT within the Milan criteria is known to have a recurrence rate of 8–20% in HCC patients [472]. Due to the effects of immunosuppressants, the prognosis of HCC that recur after LT is poor, with a median survival of <12 months after the diagnosis of recurrence and a 5-year survival rate of only 22% [472,473]. In 119 patients with HCC who underwent LT, recurrence occurred in 16 patients (13.4%) during a 17.2-month median follow-up period, and intrahepatic recurrence was the most common type [474]. In another study of 857 patients with HCC who underwent LT, recurrence occurred in 106 patients (12.4%) during a median follow-up period of 15.8 months after transplantation, and the median survival period after recurrence was 10.6 months. The recurrence sites were in the order of lung (55.7%), transplanted liver (37.8%), abdominal cavity (37.7%), and bone (25.5%) [475]. The prognosis of patients with HCC who have relapsed after LT depends not only on the stage before transplantation or the pathological findings of the removed liver, but also on the time to recurrence after transplantation and whether it has invaded multiple organs. Furthermore, the treatment method for recurrent cancer is an important factor; hence, it is necessary to apply the appropriate individualized treatment to patients [476].
Even if HCC recurs after LT, the survival rate can increase if curative treatment is available. In 121 patients who had cancer recurrence after LT, 38 (31.4%) patients received hepatic resection or local therapy, 51 (42.1%) received palliative care, and the remaining 32 (26.4%) received conservative treatment [477]. Among these patients, the median survival period of those who could receive radical treatment was significantly longer than those who received other treatments. A study performed in Japan included 101 patients who underwent LDLT for HCC between 1996 and 2007, of which 17 patients with recurrence were analyzed. Nine patients underwent surgical treatment, including hepatic resection (six cases), resection of lung metastasis (10 cases), and resection of lymph node metastasis (three cases); and eight patients received non-surgical treatment. The survival rates for 1, 3, and 5 years in patients with hepatic resection were 100%, 87.5%, and 87.5%, respectively, whereas the survival rates in patients with non-surgical treatment were 50%, 12.5%, and 0%, respectively, showing significant differences [478].
When the recurrent HCC after LT is confined within the liver and hepatic resection is unviable, RFA may provide a good prognosis. In one study, of the 486 patients who underwent LT, HCC recurred in 78 patients (16%) and 15 patients underwent hepatic resection, 11 patients RFA, and 52 patients received conservative treatment. The survival rates for 1, 3, and 5 years in the surgical group were 92%, 51%, and 35%, respectively, and the survival rates in the RFA group were 87%, 51%, and 28%, showing no significant difference between the two groups (P=0.879). The RFS rates for 1, 3, and 5 years in the surgical group were 83%, 16%, and 16%, respectively, and the RFS rates in the RFA group were 76%, 22%, and 0%, respectively, with no difference between the two groups (P=0.745) [479]. Since HCC that recur after LT is often multiple or accompanied by extrahepatic metastases, it is not common to apply radical hepatic resection or RFA. Although there are limited studies on the efficacy and safety of TACE when recurrence occurs after LT, a study of 14 patients with intrahepatic or intrahepatic and extrahepatic recurrent HCC reported that the partial response (PR) after TACE was 57%, stable disease (SD) was 28%, and the disease progressed in 14% of patients. The survival rates at 6, 12, and 24 months after recurrence in patients who received TACE were 64.3%, 50%, and 22.2%, respectively, while the survival rates of 14 patients who received systemic chemotherapy were 35.7%, 21.4%, and 10.7%, respectively (P=0.034) [480]. The Child-Pugh score did not significantly increase after TACE, there was no severe adverse event, and the degree of postembolization syndrome (PES) was not different from that of patients who did not undergo LT. In a study conducted in Taiwan, 11 patients with recurrent multiple HCCs after LT underwent TACE, and the median survival rate was 6.6 months (0.3–12.7 months) with a 1-year survival rate of 12.5% [481].
Sorafenib may be used when hepatic resection, RFA, or TACE cannot be performed due to extensive recurrence, or in cases when the disease progresses after local therapy; however, there has been no well-designed RCT to verify its efficacy and safety. In a case-control study of 39 patients, 24 patients were treated with best supportive care and 15 patients were treated with sorafenib, and the median survival period was 21.3 months from the time of recurrence in the sorafenib group, which was significantly longer compared to the 11.8 months in the supportive care group (HR, 5.2; P=0.0009), and no severe adverse event was observed after sorafenib [482]. However, another study reported that sorafenib is more toxic after LT [483]. In particular, a case of death due to gastrointestinal hemorrhage was reported when sorafenib and everolimus, an mTORi, were combined to increase the anti-cancer effect [484]. Since there has been a report of severe side effects and a high rate of dose reduction, continuous monitoring of mTORi from the beginning is essential [485]. In another study, among 34 patients with recurrent HCC after LT, 17 patients were treated with sorafenib and the remaining 17 patients received conservative treatment, with the survival rates at 3 months and 12 months in the two groups being 100% and 62%, and 73% and 23%, respectively, showing a significant difference. Adverse events occurred in the order of diarrhea (18%), elevated transaminase (11%), fatigue (11%), hand-foot skin reaction (HFSR) (6%), and nausea (6%) [486].
There has been a report on the use of regorafenib as a second-line treatment after sorafenib failure in patients with recurrence after LT. According to a multicenter retrospective study in Europe, in 28 patients who received LT, the median OS from regorafenib initiation was 12.9 months and 38.4 months since sorafenib administeration [487]. There were only common side effects in patients who received LT. Another multicenter retrospective study showed that among 132 patients who were administered sorafenib after LT, those who used regorafenib as second-line treatment had a significantly higher survival rate compared to those who received only supportive care after the failure of sorafenib, and multivariate analysis showed that regorafenib independently lowered mortality [488].
The use of other tyrosine kinase inhibitors such as lenvatinib, cabozantinib, and ramicirumab, a monoclonal antibody, may also be considered, but evidence is still insufficient to verify the safety and efficacy of their use after LT. Recently, reports on the use of immune checkpoint inhibitors targeting cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) and programmed cell death (PD)-1/programmed cell death-ligand 1 (PD-L1) in patients with HCC who have undergone LT have been released [489-491]. According to these reports, rejections due to the immune checkpoint inhibitors may occur in up to half of them, and immediately after 1–2 weeks of commencing immunotherapy. Treatment strategies commonly used for rejections, such as steroids, may work; however, the use of immune checkpoint inhibitors in patients who receive LT requires much attention.
[Recommendations]
1. For recurrent HCC after being cured by LT, the retreatment method can be selected considering the time to recurrence, liver function, performance status, size, location, and the number of recurrent tumors (C1).
LOCAL ABLATION THERAPIES
Local ablation therapies are widely performed as non-surgical treatments for HCC, as they are easy to perform and induce tumor necrosis with minimal damage to the normal hepatic parenchyma. Among various local ablation therapies, RFA and PEI are accepted as standard treatments. In recent years, microwave ablation and cryoablation have been considered as effective local ablation therapies, while clinical trials are underway for other modalities, such as laser ablation therapy and high-intensity focused US.
The indications for local ablation therapies include patients with a single HCC ≤5 cm or up to three nodules ≤3 cm, although minor discrepancies exist across different investigators and studies. Efforts to apply local ablation therapies to larger HCCs have been made; however, the treatment outcomes are closely associated with the tumor size. If the corrected platelet count is less than 50,000/mm3, the prothrombin time is less than 50%, or the international normalized ratio (INR) is equal to or higher than 1.5–1.8, then the risk of tract bleeding following the ablation procedure may be high [492,493].
RFA
RFA is the most widely used local ablation therapy for HCC. Very fast alternating currents (460–500 kHz) flow in the vicinity of radiofrequency electrodes, inducing internal friction among molecules. The internal heat generated by the internal friction can evoke tissue necrosis. Exposure to temperatures higher than 60°C causes almost immediate protein denaturation and destruction of cell membranes, followed by coagulative necrosis. Similar necrotic effects can also be obtained by maintaining the temperature of 45–50°C for ≥3 minutes. The main advantage of RFA compared with PEI is that fewer treatment sessions are required to achieve complete tumor necrosis. For HCC nodules ≤2 cm, RFA results in a higher complete tumor necrosis rate compared to PEI [494-497]. Most procedures are performed via a percutaneous approach; however, a laparoscopic or open surgical approach may sometimes be required.
The initial complete tumor necrosis rates, which were evaluated by CT or MRI within 1 day to 1 week after RFA, were reported to exceed 95%. If RFA procedures are repeated for residual viable tumors, a complete tumor necrosis rate of almost 100% can be achieved [496,498]. However, the 3-year local tumor progression (LTP) rate after RFA ranges widely from 0.9% to 21.4% [453,498,499]. According to Shiina et al. [498], the 10-year LTP rate after RFA was 3.2%. However, Kim et al. [453] reported a 10-year LTP rate of 38.2% after RFA, and there is a big difference in LTP rate across institutions. The independent factors associated with the OS after RFA include initial complete tumor necrosis, Child-Pugh score, number and size of tumors, and pre-operative serum AFP level. The best outcome after RFA can be achieved in patients with a single HCC <2 cm in diameter and Child-Pugh class A function. If the tumor location is ideal for performing RFA, the efficacy of RFA is comparable to that of hepatic resection. Hence, some reports suggest that RFA should be considered a primary treatment [214,499]. The treatment outcome after RFA of HCC is affected by the location of the tumor. The best results can be expected when the tumor is not attached to the hepatic capsule, intrahepatic blood vessels, or central bile duct [500]. Subphrenic HCCs have a high risk of LTP after US-guided RFA, and the frequency of peritoneal seeding has been reported to be up to 9.5% [501,502]. In addition, when 3 mm or more of the tumor surface is in contact with the portal vein or hepatic vein, RFA may not be effective due to the heat-sink effect, and the risk of complication increases due to blood vessel or bile duct damage [501,503,504].
The long-term survival outcomes after RFA of HCC patients are dependent on the tumor size. For Child-Pugh class A patients with tumors <2 cm, the 3- and 5-year OS after RFA are approximately 90% and 65–70%, respectively [453,498,499]. Meanwhile, the corresponding OS for 2–5 cm tumors are 65–75% and 50%, respectively [453,498]. The therapeutic efficacy of RFA has been improved with the introduction of antiviral treatment [505], and the 5-year rates of OS were 83.7–85.1% in the recent RFA studies from South Korea in HCC patients within the Milan criteria [501,506].
No-touch RFA has recently been performed after placing multiple electrodes outside the tumor. It showed a lower LTP rate compared to conventional tumor-puncturing RFA [507,508]. A prospective multicenter study also found improved local tumor control after no-touch RFA for HCC [509]. However, further investigation is warranted to evaluate whether no-touch RFA would also enhance the survival outcomes after treating patients with HCCs.
Most studies comparing RFA with hepatic resection for HCC were not RCTs; even with RCTs, their sample size was not big enough to make a definite conclusion [510]. Three RCTs, including a recently published study, showed no significant difference in survival rate between the two treatments [511-513]. In a RCT that reported a significant difference in survival rates between the two therapies, the number of patients included in the single HCC <3 cm group was too small, and the 1-year survival rate of RFA was 91%, which was substantially lower than the 100% survival rate of hepatic resection [514]. A meta-analysis of eight RCTs showed that the 5-year OS and DFS were not significantly different between the hepatic resection and RFA groups for HCC patients within the Milan criteria [515]. In a prospective controlled study recently published in South Korea [516], there was no difference in the survival rates between hepatic resection and RFA; however, the DFS was longer in the hepatic resection group. Other non-RCTs reported no significant difference in survival rates between hepatic resection and RFA in treating HCC ≤3 cm in diameter [517-519]. Hepatic resection had a higher incidence of complications and a longer hospital stay of 8 to 9 days on average [520].
A RCT comparing repeat hepatic resection and RFA in HCC patients who relapsed within the Milan criteria after hepatic resection also showed the same results as patients with treatment-naïve HCC. However, in patients with recurrent HCCs >3 cm and AFP levels ≥200 ng/mL, repeat hepatic resection showed better OS and DFS rates compared to RFA.
It is well-known that MRI findings, serum levels of tumor markers, and tumor size are related to microvascular invasion of HCC. HCCs with a high risk of microvascular invasion have shown poor prognosis after RFA [366,521,522]. However, since no RCT or meta-analysis has been performed yet, additional studies are needed.
For HCCs >3 cm, the local recurrence rates after RFA range from 30% to 50% [453], and combined treatment with TACE and RFA can be considered for these tumors. In three or fewer HCCs of ≤3 cm in diameter, the survival rate and recurrence rate were not significantly different between the combined treatment and RFA alone groups [523]. In contrast, when the size of HCC ranged from 3 cm to 5 cm, the LTP rate and survival rate were better in the combined treatment group [524,525]. A meta-analysis of seven RCTs showed better survival in the combined treatment group than the RFA monotherapy group; however, the subgroup comparison of tumors <3 cm in size showed no significant difference in survival rate between the combined treatments and RFA alone groups [526]. In a meta-analysis of eight RCTs comparing RFA alone and combined TACE and RFA, the combined treatment group showed better survival and recurrence rates; however, there was no significant difference in the major complication rates between the two groups [527,528]. Considering the results above, the combination of TACE and RFA in treating HCCs with 3–5 cm in size showed a higher survival rate and lower recurrence rate compared to RFA alone, with no significant difference in the incidence of complications between the two treatments.
Despite these favorable outcomes, RFA has some disadvantages. First, the risk of major adverse events is usually higher than that of PEI, particularly when the tumors are located near the liver hilum or major abdominal organs, such as the colon. In addition, the heat-sink effect may hinder the effective transmission of heat energy to a tumor adjacent to relatively large intrahepatic vessels [497,529,530]. Sometimes, however, the risk of thermal injury to the adjacent abdominal organs can be overcome by inducing artificial ascites [531]. Another major limitation of RFA is that HCCs <2 cm may not be visible on the conventional US. However, recent applications of US contrast agents and fusion imaging techniques have broadened the indications for RFA in such cases [532,533]. In a prospective study of 216 patients with HCCs <5 cm conducted in South Korea, 30 (39.5%) of 76 HCCs not visible on the B-mode US were recognizable on fusion imaging [532]. Also, for 60 HCCs untreatable with RFA under B-mode US guidance, all of them could be treated when fusion imaging was applied. In this study, the technical success rate was 97.1% after fusion imaging-guided RFA. On the other hand, for small HCCs which are challenging to detect on the B-mode US, the detection rate was improved when the CEUS was performed [533]. In particular, the detection rate of HCC was higher when CEUS was performed with fusion imaging than when the CEUS was used alone.
The mortality rate due to procedure-related complications after RFA is reported to be 0.1–0.5%, and the major complication rate after RFA is less than 5% [499,529,530]. Major complications include needle tract seeding, hemoperitoneum, hemothorax, liver abscess, massive infarction of liver parenchyma, intestinal perforation, and pneumoperitoneum [498].
In conclusion, for HCCs within the Milan criteria, hepatic resection has shown a lower recurrence rate than RFA and a higher postoperative complication rate; however, further studies are warranted to verify the difference in the survival rate. For single nodular HCCs <3 cm in diameter, RFA has an equivalent survival rate, higher LTP rate, and lower complication rate than hepatic resection. Therefore, it can be used as an alternative treatment for surgery if the location of HCC is ideal to perform RFA.
PEI
PEI was widely used in treating HCC, since it is relatively simple to perform and adverse reactions are infrequent. However, it has to be performed repetitively in contrast to RFA, and it is difficult to obtain complete necrosis for tumors >3 cm as the diffusion of injected ethanol may be blocked by the fibrous septum or tumor capsule, resulting in a decreased therapeutic effect. Therefore, PEI has been largely replaced by RFA. The tumor necrosis rate of PEI was reported to be 66–100% [495-497,534]. Tumor size is important; tumors <2 cm in diameter have more than a 90% tumor necrosis rate. However, as the tumor size increases, the necrosis rate decreases, and the tumor necrosis rate is only 50% for tumors 3–5 cm in size. LTP rates after PEI range between 24% and 34%, but it was reported to be as high as 43% for HCCs ≥3 cm [535-538]. For patients with Child-Pugh class A function and a solitary HCC <2 cm, the 3- and 5-year OS are 70–80% and ≥ 50%, respectively. For HCCs 2–3 cm in diameter, the 3-year OS ranges from 47% to 64% [495,534].
Among the RCTs comparing RFA and PEI in patients with HCC [495-497,534,539,540], except for those published in Italy [539,540], RFA showed a significantly lower LTP rate and a higher survival rate. In particular, in a meta-analysis of four RCTs, the 3-year survival rate of RFA was significantly higher than that of PEI [541-544]. However, there was no significant difference in the survival rates between the subgroups of HCCs <2 cm in diameter [543]. These results suggest that the RFA group has a lower LTP rate and a higher survival rate compared to the PEI group; however, further study is needed. In HCCs <2 cm in diameter, studies have reported a similar OS, and PEI can be considered if RFA is not feasible [545]. PEI can be performed to treat perivascular tumors to reduce the heat-sink effect of RFA. However, the risk of biliary stricture also exists with PEI if the tumors are located in the liver hilum [546,547].
Microwave ablation and cryoablation
Recently, the use of microwave ablation and cryoablation are increasing. The advantage of microwave ablation over RFA is that effective ablation can be expected even for tissues with low electrical conductivity, and an ablation temperature over 100oC can be achieved rapidly [548]. Therefore, the treatment efficacy of microwave ablation is less affected by blood vessels located near the tumor, and the size of the ablation zone is larger. For these reasons, microwave ablation is frequently used for HCCs ≥2 cm instead of RFA. Meanwhile, monitoring the ablation zone during cryoablation is relatively easy since the ice ball shows a clear margin under the US, non-enhanced CT, or MRI guidance. Moreover, cryoablation has less procedure-related pain [548,549]. However, cryoablation with a single probe generates a small ablation zone, requiring multiple cryoprobes in most cases, and it is rather time-consuming compared to other thermal ablations.
In Child-Pugh class A and B patients with up to three HCCs and a tumor size ≤4 cm, a RCT showed no significant differences in the 2-year LTP rate between RFA and microwave ablation [550]. In a RCT comparing the RFA and the microwave ablation for HCC ≤3 in number and up to 5 cm in size in Child-Pugh class A and B patients, there were no significant differences in the OS, DFS, and complication rate between the two groups. However, the total ablation time of microwave ablation was shorter than that of RFA [551]. A meta-analysis comparing RFA and other ablation therapies revealed no significant difference in the OS and major complication rate between RFA and microwave ablation [544,552-554]. On the other hand, combined TACE and microwave ablation showed a higher OS and lower recurrence rate than microwave ablation alone in a RCT for treating HCCs that are 3–5 cm in size [555].
In patients with Child-Pugh class A and B liver cirrhosis and one or two HCCs, a multicenter RCT showed no significant difference in the 1-, 3-, and 5-year OS, DFS, and major complication rate between RFA and cryoablation [556]. However, cryoablation has been reported to have a lower complication rate compared to RFA in treating HCCs located near the bile duct or intrahepatic vessels [557,558].
In the limited RCTs and meta-analyses mentioned above, microwave ablation and cryoablation showed similar results in terms of the OS, recurrence rate, and major complication rate compared to RFA. Currently, in South Korea, the cost of cryoablation is higher than that for RFA. Additional large-scale prospective RCTs are needed to confirm the difference in therapeutic efficacy among various local ablation therapies.
Other local ablation therapies
Clinical trials on other local ablation therapies, such as high-intensity focused US and laser ablation, are underway. However, as there are few comparative studies with standard treatment, further technological developments and outcomes from the ongoing clinical trials are required to verify their efficacy in managing HCC.
Treatment of intrahepatic recurrence after RFA
LTP was reported to be higher in patients who underwent RFA than in those who underwent hepatic resection [514,559]. LTP is defined as recurrence of tumor at the treatment site or margins in which complete response (CR) was verified after initial local ablation therapy. The 3-year LTP rate after RFA has been reported to be 14.5% for HCC patients within the Milan criteria [560].
A large-scale retrospective study at a single institution in South Korea reported that the 5- and 10-year cumulative recurrence rates were 73.1% and 88.5%, respectively, after RFA for HCC patients within the Milan criteria [453]. RFA showed the best therapeutic efficacy for patients with small single nodular HCC (especially tumors ≤2 cm) and well-preserved liver function with a 5-year survival rate of 70% [499]. Since repeated RFA for recurred HCC after RFA can improve survival if it achieves a CR, an early detection of recurrence is essential [561]. Surgical treatment, such as hepatic resection and salvage LT, for recurrent HCC after RFA, showed similar therapeutic efficacy compared to repeated RFA [562,563]. If surgical treatment or RFA is not feasible, TACE can be applied [564].
[Recommendations]
1. RFA has an equivalent survival rate, a higher LTP rate, and a lower complication rate compared to hepatic resection in patients with a single nodular HCC ≤3 cm in diameter (A1).
2. Combined therapy with TACE and RFA or microwave ablation increases the survival rate in patients with 3–5 cm HCCs that are not amenable to hepatic resection compared to RFA or microwave ablation alone (A2).
3. In the treatment of HCC, microwave ablation and cryoablation are expected to produce comparable rates of survival, recurrence, and complications to those of RFA (B2).
4. Contrast-enhanced US and fusion imaging improve the detection rate and the technical success rate of local ablation therapy for HCCs ≤2 cm (B1).
TACE AND RADIOEMBOLIZATION
The majority of HCCs are unresectable at the time of diagnosis due to portal hypertension, poor liver function, multiplicity of tumors, portal vein tumor invasion, inability to secure sufficient resection margin, old age, and severe comorbidities [565]. TACE is the most commonly used non-surgical treatment modality for these patients; tumor necrosis can be achieved by the combined effects of antitumor chemotherapy and selective ischemia of tumor tissue [427,565-567]. TACE can be classified as cTACE using lipiodol and drug-eluting bead (DEB)-TACE. TARE is an internal radiation therapy in which the microspheres containing radioactive isotopes are infused into the hepatic artery. As safe and effective methods of delivering radiation to tumors are established, TARE is increasingly being used for the management of HCC.
cTACE
The cTACE procedure involves the injection of a mixture of chemotherapeutic agents, such as doxorubicin, cisplatin, and mitomycin, with iodized oil into the tumor-feeding artery as an emulsion, followed by embolization using gelatin sponge particles, polyvinyl alcohol particles, or microspheres, which induce tumor ischemia. In order to maximize the anticancer effect and minimize liver damage, TACE should be performed as selectively as possible through the tumor-feeding arteries [568,569]. Superselective TACE through the tumor-feeding arteries can significantly increase the tumor necrosis and the local control rate [570-572]. In addition, cone-beam CT during TACE can help demonstrate tumors, tumor-feeding arteries, and iodized oil accumulation at the tumor during procedure more precisely and also detect occult lesions, thereby resulting in a better therapeutic effect [573-576]. Regarding the repetition strategy of TACE, on-demand repetitions to treat the residual or recurrent tumors can minimize the incidence of procedure-related liver toxicity, which is therefore preferable to on-schedule regular repetitions every 1–2 months. Although TACE has been used in clinical practice for a long time, its detailed techniques are not standardized, and the differences according to chemotherapeutic agents and embolic materials are still insufficiently known [577]. In a recent multicenter RCT conducted in Japan, there was no significant difference in tumor response rate and survival rate between miriplatin and epirubicin in cTACE [578].
Compared with best supportive care, several RCTs and meta-analyses have confirmed that cTACE results in a more favorable tumor response, time to progression (TTP), and survival outcomes in patients with unresectable HCC [579-583]. A prospective cohort study by the Japanese Liver Cancer Study Group reported that the 1-, 3-, 5-, and 7-year survival rates of 8,510 patients who underwent TACE were 82%, 47%, 26%, and 16%, respectively; for tumors larger than 5 cm, the 1-, 3-, and 5-year survival rates were 63%, 30%, and 16%, respectively [581]. In a prospective multicenter study performed in 27 Japanese and South Korean centers, the complete or partial remission rate according to the modified Response Evaluation Criteria in Solid Tumors (mRECIST) criteria was 73% and the 2-year OS was 75%; these figures were higher than those previously reported in the literature [584]. These results were supported by a recent systematic review of 101 articles on cTACE published over the last 30 years, which showed that the OS was 70.3% at 1 year, 51.8% at 2 years, 40.4% at 3 years, and 32.4% at 5 years [583]. This outcome was similar to those of published RCTs.
Local tumor response after cTACE can vary substantially according to the size and number of tumors, as well as the patterns of tumor growth, such as tumor encapsulation and vascular invasion [581,582]. The complete remission rate is quite low for large or multiple tumors despite multiple TACE sessions. However, in small tumors, complete tumor necrosis can be obtained in more than 50% of cases after superselective cTACE [569]. A prospective cohort study conducted in South Korea comparing hepatic resection after primary cTACE with cTACE monotherapy reported that the survival rates were similar between the two treatment groups for stage T3 HCC. Moreover, the survival rate of the TACE group for stage T1 and T2 HCC was similar to that of the hepatic resection group if iodized oil was compactly retained within the tumor [585]. In a prospective cohort study of BCLC stage A HCC patients in whom resection or ablation could not be performed, the 1-month complete remission rate according to the mRECIST criteria was 67%, and the 3-year OS was 80% [586]. In three retrospective studies conducted in South Korea on patients with small HCC within the Milan criteria, there was no significant difference in the long-term (>5 years) OS among hepatic resection, RFA, and cTACE, although TTP was the shortest in the cTACE group [587,588]. Given the potential selection bias of the studies mentioned above, cTACE can be considered as an alternative to treatments with curative intent when a patient refuses surgical treatment or is at a high risk for undergoing surgery, or HCC is unsuitable for local ablation therapy.
Portal vein tumor invasion is found in approximately 30% of patients with HCCs at initial diagnosis in South Korea [566]. Systemic chemotherapy is the standard primary treatment for HCC with portal vein invasion [213]. However, in real-world practice, more aggressive treatment and various kinds of combination therapy are used, since the expected survival benefits of systemic therapies are modest and no study has yet compared systemic therapy and locoregional treatment, such as cTACE [567,589]. cTACE can be safely performed in advanced HCC patients with portal vein tumor invasion and preserved liver function, without significant risk of liver function deterioration [590-594]. In patients with unresectable HCC with portal vein invasion, survival outcomes were more favorable in the TACE-treated groups than in the supportive treatment groups [595-597]. The prognosis was better for tumors localized in one or two hepatic segments, tumors with nodular growth pattern [590,591], or when only segmental portal vein was involved [581,594]. According to a single-center retrospective analysis of cTACE for HCC with segmental portal vein invasion, the median survival was 26.9 months in patients with Child-Pugh class A, ECOG 0, and no extrahepatic spread [598]. The therapeutic effectiveness can be improved by combining cTACE and radiation therapy [49,599,600]. Recently, a Korean single-center RCT reported that cTACE combined with radiation therapy significantly increased the OS, the objective response rate (ORR), and TTP compared to sorafenib monotherapy in patients with HCC and portal vein invasion [601]. Furthermore, a few retrospective studies showed that TACE is associated with survival gain when intrahepatic HCC is treated with TACE in patients with extrahepatic spread [602-604].
There have been several studies on the combination of cTACE with systemic therapy to increase the therapeutic effectiveness compared to cTACE alone [605]. Recently, in a multicenter prospective phase 2 randomized study conducted in Japan, the combination therapy of cTACE and sorafenib showed better progression-free survival (PFS) compared to cTACE alone in HCC patients without portal invasion and extrahepatic spread [606]. Studies on combination with lenvatinib, a targeted therapy introduced into clinical practice after sorafenib, is ongoing [607], but its benefits compared to TACE alone has not yet been fully demonstrated. Further studies are needed to select the patients who would benefit most from cTACE combined with systemic therapy compared to other treatments.
The most common complication after cTACE is PES, which is a complex of symptoms, including fever, abdominal pain, nausea, and vomiting. Serious liver-related complications, including irreversible hepatic failure, hepatic infarction, abscess, and biliary injury, can occur. Sepsis, pulmonary oil embolism, cholecystitis, gallbladder infarction, and gastrointestinal complications may also occur [608]. The frequency and severity of complications are related to the tumor size, hepatic functional reserve, portal vein invasion, extent of chemoembolization, and the dose of chemoembolic agents. According to a systematic review, the most common complication after TACE was fever (57.8%), followed by liver enzyme abnormalities (52.0%), PES (47.7%), abdominal pain (42.5%), fatigue/malaise (39.9%), anorexia (38.0%), vomiting (34.2%), nausea (32.4%), and hematological/bone marrow toxicity (28.6%). Hepatic failure occurred in only 1% of the patients, and no new or unexpected safety concerns were identified [583]. The use of anti-inflammatory drugs, such as dexamethasone or parecoxib, to reduce PES before and after TACE has been reported in RCTs [609-611], but caution is still required due to the risk of adverse effects, such as worsening of viral hepatitis or diabetes.
In conclusion, cTACE is expected to have the best efficacy and safety when it is selectively performed through tumor-feeding arteries in patients with preserved liver function and good performance status to HCCs localized in the liver with nodular tumor growth and no vascular invasion.
DEB-TACE
Drug-eluting microspheres or DEBs refer to microspheres loaded with high-dose doxorubicin, which can embolize tumor feeders. Embolization of the tumor feeders with DEBs has several benefits, such as tumor ischemia, higher intratumor drug concentration, and lower serum drug concentration due to the slow release of doxorubicin from the DEBs [612].
Prospective RCTs did not show a significant difference in the tumor response rate, time-to-recurrence, and OS between the DEB-TACE group and cTACE group [613-615]. In a prospective multicenter study conducted in Europe on 173 patients who underwent DEB-TACE, the 5-year OS rate was 22.5% [616].
A prospective multicenter registry including 152 Korean patients showed a complete remission and ORR of 40.1% and 91.4% at 1 month, and 43.0% and 55.4% at 6 months, respectively [617]. PFS was 9.3 months and the 2-year OS was 79.7% [618]. There was no mortality related to complications including liver abscess. In subgroup analysis, the best tumor response was shown in 2–5 cm tumors, and the tumor response was lower in <2 cm tumors [618]. The same trend was also observed in a retrospective study conducted at a Korean single center; and in particular, the objective tumor response of DEB-TACE was significantly lower than that of cTACE in <3 cm tumors [619]. This is presumed to be because DEBs cannot reach the small tumor sufficiently. Recently, DEBs that are sized <100 μm have been introduced into clinical practice, and several small scaled studies have been reported [620,621]. Further studies regarding their safety and therapeutic efficacy are needed.
At the beginning of the introduction of DEB-TACE, since it is pharmacokinetically superior to cTACE, it was expected to have less hepatic or systemic toxicity and be more useful for patients with liver dysfunction or poor performance [622]. However, in the prospective studies, there was no significant difference in hepatotoxicity or deterioration of liver function after DEB-TACE compared to cTACE [614,615]. Pain after the procedure was less severe and less frequent, and the length of hospital stay was also shorter by 1 day in the DEB-TACE group [615,619]. Since DEBs are small permanent embolic materials, global damage to the liver parenchyma and biliary tree was reported to be two times more common compared to cTACE [623]. However, in case of superselective infusion through tumor-feeding arteries, the clinically relevant damage to the liver parenchyma and biliary tree in DEB-TACE was not significantly different from that in cTACE [619].
In conclusion, DEB-TACE has similar long-term survival, less PES, and shorter hospital stay than cTACE. Therefore, further studies are needed to establish optimal indications for DEB-TACE, considering its cost-effectiveness and the lower response rates in small tumors.
TARE using 90Y microspheres
TARE involves the injection of implantable radioactive microspheres into tumor-feeding arteries to expose the tumor to highly concentrated radiation while protecting the normal parenchyma. 90Y is the most commonly used radioisotope that emits high-energy and pure β-rays with a half-life of 64.2 hours, and the mean and maximum tissue penetration of 2.5 mm and 11 mm, respectively. The microspheres available for 90Y infusion are 20–60 μm in diameter and are made of resin or glass. The small size of the injected microspheres and their concentration in hypervascular HCC minimize the embolic effect on the surrounding tissue. Preprocedural angiography and 99mTc-labeled macroaggregated albumin scans are required to determine the treatment site, radiation dose and the degree of shunting to the lungs and any other extrahepatic organs. In particular, assessing the lung dose via hepatopulmonary shunt is important, as exceeding the permitted lung dose can increase the risk of radiation pneumonitis [624]. Recently, in a retrospective analysis of 448 patients with HCC within the Milan criteria who underwent 90Y TARE, it was reported that the estimation of lung shunt may be eliminated in these patients since the tumor burden is not large, and the required radiation dose and the degree of hepatopulmonary shunt is not high except in patients with transjugular intrahepatic portosystemic shunt [625].
According to the results of a phase 2 study of 90Y TARE conducted in the United States and Europe between 2010 and 2013, the median survival period was 24.4–26.9 months in BCLC stage A, 16.4–18 months in BCLC stage B, and 7.3–13 months in BCLC stage C [626-629]. There has been no large-scale prospective RCT comparing TACE and 90Y TARE to date, and according to the meta-analysis of three small RCTs, there was no significant difference in the survival rates and safety between the two treatments [630-633]. Two phase 3 RCTs did not demonstrate the OS of 90Y TARE to be superior to sorafenib in HCC with portal vein invasion, although it had a higher tumor response rate and fewer side effects [634,635]. Also, in a multicenter prospective RCT comparing the combination therapy of 90Y TARE and sorafenib with sorafenib monotherapy, there was no significant difference in the OS [636].
Recently, improved outcomes were reported by using a higher radiation dose than the standard dose (absorbed tumor dose, 100-150 Gy) [637]. In a multicenter retrospective study of 90Y TARE using a high radiation dose (median absorbed dose, 410 Gy) for a single HCC sized less than 8 cm, the complete remission rate was 84% and the 3-year survival rate was 86.6% [638]. In a multicenter prospective RCT conducted in France on patients with BCLC stage B and C with tumors larger than 7 cm, the standard dosimetry arm applied to deliver 120±20 Gy to the perfused lobe had a median survival period of 10.7 months, while the personalized dosimetry arm applied to deliver at least 205 Gy to the tumor had a median survival period of 26.6 months [639]. In a Korean single-center study of 90Y TARE with over 150 Gy delivered to ≥5 cm HCC, the complete remission rate was 80% [640]. According to a retrospective cohort study of patients with a single HCC sized ≥5 cm at two Korean centers, 90Y TARE showed similar OS and PFS compared to hepatic resection, with fewer side effects and superior safety [641]. Therefore, 90Y TARE, like TACE, can minimize liver damage and maximize the therapeutic efficacy when the procedure is selectively performed through the tumor-feeding artery. Further studies are needed to select appropriate patients and to compare 90Y TARE with other treatments.
The most common side effect of 90Y TARE is temporary fatigue and it can be safely performed even in the elderly or patients with large tumors due to less PES and better quality of life compared to TACE [642,643]. Radioembolization-induced liver disease (REILD) usually occurs 4–8 weeks after 90Y TARE, and the risk factors include small liver (<1.5 L), small functional liver volume associated with liver cirrhosis, systemic therapy within 2 months, and extensive infusion of 90Y microspheres to both lobes of the liver [644-646]. In some patients, delayed hepatotoxicity may occur 6 months after TARE, and it may not be recognized as REILD [647]. Tumor involvement of greater than 50% of the liver and cirrhosis have been reported to be predisposing factors for delayed REILD. Therefore, 90Y TARE should be performed when the tumor is localized and the remnant liver function is expected to be sufficient after the treatment. When 90Y microspheres are delivered to organs other than the liver, more serious complications than TACE, such as radiation pneumonitis and gastric ulcer, can occur; therefore, special attention is required.
In conclusion, 90Y TARE did not show an increase in the OS compared to standard treatments, such as TACE or sorafenib, in RCTs. However, considering the improved therapeutic efficacy when using a higher radiation dose and less PES, 90Y TARE can be an alternative treatment to cTACE in select patient groups, such as those with a single HCC.
[Recommendations]
1. cTACE is recommended for HCC patients with a good performance status without major vascular invasion or extrahepatic spread who are ineligible for hepatic resection, LT, or local ablation therapies (A1.
2. cTACE should be performed through tumor-feeding arteries using selective/superselective techniques to maximize antitumor activity and minimize hepatic damage (B1).
3. In cases of HCC with portal vein invasion, cTACE alone (B2) or cTACE combined with external beam radiation therapy (EBRT) (B1) can be considered for patients with intrahepatic localized tumors and well-preserved liver function.
4. Compared with cTACE, DEB-TACE has similar clinical outcomes in ≥3 cm HCCs; therefore, it can be considered as an alternative treatment to cTACE (A2).
5. Compared with cTACE, TARE results in a better quality of life and lower occurrence of PES; therefore, it can be considered an alternative treatment to cTACE when the remnant liver function is expected to be sufficient after the TARE treatment (B2).
Refractoriness to cTACE
cTACE has proven its survival benefit in patients with unresectable HCC [205,580]; therefore, it is recommended as a standard treatment for intermediate-stage HCC according to the BCLC staging system or HCC without major vessel invasion and extrahepatic metastasis, which is unsuitable for hepatic resection, LT, and other local treatments [648]. cTACE is generally considered as a palliative treatment and requires multiple sessions of treatment [649]. However, disease progression is frequently observed during repeated treatment with cTACE, and therefore the concepts of cTACE-refractoriness or cTACE-failure have been proposed [580,650]. In general, cTACE-refractoriness is defined as an insufficient response owing to tumor biology, and cTACE-failure is defined as a technical failure or an inappropriate indication [651,652].
Systemic treatment is considered as a standard treatment for advanced HCC with vascular invasion and/or extrahepatic metastasis. However, due to recent improvements in systemic therapies, an early switch to systemic therapies instead of repeated cTACE or an initial systemic therapy can be considered in patients with intermediate stage HCC who are expected to have a poor prognosis with cTACE. For this reason, it became critical to define the cTACE-refractoriness, and several studies to define the cTACE-refractoriness have been published recently. In a Korean single-center study, when the stage progression during repeated cTACE was set as a surrogate endpoint, the requirement of three or more sessions of cTACE or disease progression during first 6 months after the first session of TACE was associated with short PFS, which was consequently proposed as a predictor of cTACE-refractoriness [653]. These criteria may enable prompt switching to other treatments. However, there are some limitations as the deterioration of liver function after cTACE was not accounted for in the study, and the result is still not fully validated.
The Assessment for Retreatment with TACE (ART) score developed by researchers from Austria integrated post-cTACE elevation of AST, Child-Pugh score and the absence of radiological tumor response. The ART score of ≥2.5 after the first TACE was proposed as an indicator for early switching to sorafenib or other treatment, as it was associated with poor survival and significant adverse event after the second session of TACE [654]. Likewise, a French group developed the ABCR (AFP, BCLC, Child-Pugh, and response) score, which combined AFP, tumor stage, change in liver function, and radiologic tumor response, suggesting that patients with ABCR scores ≥4 may not benefit from further sessions of TACE [655].
Recently, another Korean multicenter study reported that the change in MoRAL score calculated using the two serum tumor markers AFP and PIVKA-II (=11 × √PIVKA-II + 2 × √AFP) may indicate TACE-refractoriness. In patients with intermediate-stage HCC, an increase of MoRAL score by 5% or more after the initial session of cTACE showed significantly shorter median OS compared to the control group (18.8 vs. 37.8 months; HR, 2.18; 95% CI, 1.37–34.6; P=0.001). Specifically, patients who had high pretreatment MoRAL score (≥89.5) and an increase in MoRAL score after the initial cTACE showed a median OS below 10 months and these patients were defined as the very poor prognosis group [656]. In addition, SNACOR score (utilizing size and number of tumors, serum AFP level, Child-Pugh score, and radiological response after the first session of cTACE) and ABRAS score (utilizing ALBI score, BCLC stage, radiological response after the first session of cTACE, serum level of AFP, and sex) were reported to predict poor prognosis after cTACE among Korean patients [657,658].
The 2012 European guidelines defined treatment stage migration as no response to at least two sessions of cTACE, and recommended switching to sorafenib [114]. The 2014 KLCA-NCC guidelines defined stage migration following repeated cTACE as cTACE-refractoriness, and recommended switching to sorafenib [116]. The 2014 Japanese guidelines provided the following criteria for TACE refractoriness: i) consecutive insufficient tumor response (≥2 sessions) in ≥ 50% of lesions; ii) two or more consecutive progressions in tumor number; iii) development of vascular invasion or extrahepatic spread; or iii) continuous elevation of tumor markers [659]. The 2018 KLCA-NCC guidelines defined i) no objective response (CR or PR) after two or more sessions of on-demand cTACE during 6 months, ii) development of vascular invasion, or iii) development of extrahepatic metastasis as cTACE-refractoriness, and recommended to switch treatment [660].
To date, various definitions of TACE refractoriness exist, and a treatment strategy to overcome such a condition has not been well-established. Systemic treatments with proven efficacy for advanced HCC, including sorafenib, lenvatinib, atezolizumab/bevacizumab, and durvalumab/tremelimumab, have been proposed as a treatment option to overcome cTACE-refractoriness. Although switching to systemic treatment should be recommended if HCC progresses to an advanced stage with extrahepatic spread or vascular invasion, evidence for patients with cTACE-refractoriness presenting only with intrahepatic progression is limited. A sub-analysis of the Phase III Study of Sorafenib in Patients With Advanced Hepatocellular Carcinoma (SHARP) trial showed the survival benefit of sorafenib in patients with prior TACE compared with placebo [661]. However, it remains questionable whether sorafenib is the optimal treatment for cTACE-refractoriness, as there has been no study comparing sorafenib and locoregional therapies. Two retrospective studies conducted in Japan demonstrated that a switch to sorafenib was associated with longer OS and slower hepatic functional deterioration compared to continued cTACE in patients with TACE refractoriness [662,663]. In a retrospective study on patients with TACE refractoriness in Japan, hepatic artery infusion chemotherapy (HAIC) showed promising results in terms of tumor response and survival [664]. It is warranted to evaluate the therapeutic role of various systemic agents that were recently introduced for patients with cTACE-refractoriness.
On the other hand, given the potential ischemic injury due to tissue ischemia following TACE, combination treatment strategies are under investigation, such as TACE plus systemic agents with antiangiogenic property (e.g., sorafenib) [665]. However, the patients enrolled in these clinical trials appear heterogeneous in terms of tumor stage [666], which indicates that a clinical trial designed solely for TACE-refractoriness has not yet been conducted. Several recent studies on combination treatments have shown mixed results. A systematic review with meta-analysis reported that prolonged TTP without significant improvement in OS was achieved with a combination of TACE and sorafenib, compared to TACE alone [667]. A global SPACE trial on combination of sorafenib and DEB-TACE failed to reach clinical significance in terms of TTP [668]. Another large-scale European study comparing combination of DEB-TACE with sorafenib vs. TACE with placebo did not improve PFS in unresectable, liver-confined HCC [669]. In the ORIENTAL study, an Asian multicenter study comparing orantinib vs. placebo combined with TACE, orantinib combined with TACE failed to prolong OS, which was the primary endpoint, in patients with unresectable HCC [670]. In conclusion, the amount of current evidence supporting combination treatment of TACE and systemic agents is insufficient.
[Recommendations]
1. When developing one or more of the following conditions after two or more sessions of on-demand TACE within 6 months from the first TACE, a switch to other treatments should be considered: (1) absence of objective response, (2) new appearance of vascular invasion (3) the new appearance of extrahepatic spread (C1).
EXTERNAL BEAM RADIATION THERAPY
The role of EBRT for HCC is gradually expanding. It is mainly performed when the liver function is Child-Pugh grade A or B7, and a 40–90% tumor response rate and a median survival period of 10–25 months are reported [671-674]. For EBRT, a computerized treatment plan using CT is required. In a dose-volume analysis based on a three-dimensional treatment plan, the volume irradiated with <30 Gy should be ≥40% of the total liver volume in cases with liver function of Child-Pugh grade A or B7 [675]. Regarding hypofractionated radiation therapy with less than 10 fractions, the volume of normal liver irradiated with <15 Gy should be at least 700 mL [676], and the mean dose irradiated to normal liver should be ≤28 Gy (bioequivalent dose converted to 2 Gy per fraction) [677]. Re-irradiation for recurrent intrahepatic tumors can be performed on the same dose-volume basis as the initial treatment, if the liver function is Child-Pugh grade A or B7 [678-680]. When liver function is worse than Child-Pugh grade B7, it is necessary to apply more stringent dose-volume criteria in the computerized treatment plan [681].
EBRT can be performed for HCC patients with difficulties undergoing hepatic resection, transplantation, or other local treatments. The 3-year local control and survival rate of EBRT (including hypofractionated radiation therapy, stereotactic body radiation therapy, and particle radiation therapy) ranged from 81% to 100% and 60–87%, respectively, and the 5-year local control rate and survival rate ranged from 69–97% and 43–78%, respectively [681-711]. In a meta-analysis, the combination treatment of TACE and EBRT showed a significantly better response rate as well as the 1- and 3-year survival rates, compared to TACE alone [712]. In cases where TACE was infeasible due to severe arteriovenous shunt, vascular occlusion was induced in about 20% of patients after EBRT, thereby enabling subsequent TACE [713]. Response rates of 63–88% were reported after applying EBRT for HCCs with incomplete response after TACE [714-716]. Sequential combination of EBRT after 2 weeks of TACE may cause deterioration of liver function, but liver dysfunction of grade ≥3 in the Common Terminology Criteria of Adverse Event (CTCAE) was less than 2.5% [717].
EBRT can be safely performed in advanced HCC with macrovascular invasion. After EBRT, the overall tumor response rate was reported to be 30–96%, and the median survival time was 7–34.4 months [681,686,692,718-737]. The response rates varied depending on the location of tumors; 30–83% for portal vein tumor invasion and 43–96% for inferior vena cava and right atrium tumor invasion. The median survival period after EBRT in HCC with inferior vena cava and right atrium invasion was 12.1 months and 9.3 months, respectively, which was significantly improved from those reported in previous cohort studies [735]. In a Korean multicenter retrospective cohort analysis, 67% of patients who received EBRT for HCC with portal vein invasion received combined treatment with TACE or HAIC [738]. A recent meta-analysis reported that the combination treatment of TACE or HAIC and EBRT significantly improved the objective response and OS of HCC patients with portal vein invasion compared to those treated with TACE, HAIC [739], or sorafenib monotherapy [740]. In retrospective series analyses [599,600,741] and a recent prospective RCT [601], the combination treatment of TACE and EBRT for HCC patients with portal vein invasion significantly improved the survival rates compared to sorafenib monotherapy.
A Korean multicenter cohort study reported that concurrent administration of sorafenib and EBRT improved survival [742]. According to a Taiwan National Cancer Registry cohort study and a Korean retrospective analysis, OS was significantly improved with the addition of EBRT, even after discontinuation or failure of sorafenib [743,744]. A phase 3, multicenter RCT comparing the combination treatment of EBRT and sorafenib versus sorafenib monotherapy (ClinicalTrials.gov: NCT 01730937) is currently underway in the United States, and the results will be noteworthy. There have been several small series reporting that EBRT induces an immune response and improves the treatment outcome when combined with immunotherapy, but the evidence is insufficient at present [745,746]. Several prospective clinical studies are currently underway to investigate the effects of combination treatment of EBRT and systemic therapy.
The combination treatment of EBRT and TACE or HAIC for locally advanced HCC resulted in a median survival period of 13 to 25 months [720,737,747]. In locally advanced HCC, hepatic resection or LT can be considered when downstaging of the disease is achieved by EBRT, and these surgical treatments have been safe and effective among EBRT responders [748-752]. It has also been reported that OS was significantly improved by neoadjuvant EBRT for HCC with portal vein invasion [689,753]. In addition, EBRT can be considered as a bridging treatment for patients awaiting LT [410,754-756], or as a second-line treatment for recurrent HCC after treatments such as hepatic resection, RFA, PEI, or TACE [757-762].
EBRT is also effective in relieving symptoms caused by tumors, such as cancer pain [763,764]. When jaundice occurs due to obstruction of the biliary tract by HCCs, EBRT could relieve obstruction and jaundice by reducing the tumors, which prolongs the survival [765,766]. In cases of abdominal lymph node metastasis, EBRT showed a tumor response rate of 75–95%, and prolongation of survival was also reported [767-773]. In patients with adrenal metastases, EBRT achieved disease control in more than 90% [774]. EBRT for lung metastases showed a tumor response rate in 65–75% of the patients, and symptom improvement in 90% of the patients [771,775]. EBRT for bone metastases relieved pain in 75–99% of the patients, and the symptom relief was more significant with higher radiation dose [776-780]. EBRT for spinal metastases accompanying spinal cord compression prevented neurologic dysfunction in 63–83% of the patients [781]. EBRT can be performed to relieve symptoms of brain metastases [782]. Prolongation of PFS and OS can be expected when EBRT is performed for oligometastasis [783].
In a recent phase 3 RCT, proton beam radiotherapy (PBT) for recurrent or residual HCC of ≤3 cm in size was not inferior to RFA in local control rate, and there was no difference in the PFS, OS, and toxicity rates; therefore, PBT can be considered as one of the curative therapeutic options for patients with small HCC [784]. In a single-group study in which proton therapy was applied as the initial treatment, the 5-year local control rate and OS were 94% and 69% in BCLC stage 0/A [700,711]. In other retrospective series, SBRT for recurrent tumors of ≤3 cm in size had similar local control rates to RFA [689,785-789]; SBRT was reported to have a superior local control rate than RFA for tumors sized >3 cm [453,689,785,787].
[Recommendations]
1. EBRT is recommended for patients with HCC unsuitable for hepatic resection, transplantation, local ablation treatments, or TACE (C1).
2. EBRT is performed when the liver function is Child-Pugh grade A or B7 and when the volume to be irradiated with ≤30 Gy is ≥40% of the total liver volume in the computerized treatment plan (B1).
3. EBRT can be combined for HCCs that are expected to have an incomplete response after TACE (B2).
4. EBRT can be performed for the treatment of HCC with portal vein invasion (B2).
5. EBRT can be combined with systemic therapy for HCC treatment (C2).
6. EBRT is recommended for palliating symptoms of HCC (B1).
7. PBT is not inferior in the local control rate and shows no difference in survival and toxicity rates compared to RFA in treating recurrent or residual HCCs ≤3 cm in size (A2); SBRT may not be inferior in the local control rate compared to RFA for the treatment of HCCs ≤3 cm in size (C2).
SYSTEMIC THERAPIES
Systemic therapy refers to any drug treatment that travels the bloodstream to reach cancer cells throughout the body. Molecular targeted therapy is regarded as a therapy that targets the intracellular signals involved in the growth and metastasis of cancer cells, while immunotherapy stimulates the host immune system to fight cancer cells. Currently, conventional cytotoxic chemotherapeutic agents, molecular targeted agents, and immune checkpoint inhibitors (a type of cancer immunotherapy) are utilized as systemic therapies for HCC. The primary endpoint of phase 3 clinical trial of systemic therapy is the improvement of OS in most cases and the improvement of PFS in some cases.
First-line therapies (Table 8)
Sorafenib
Sorafenib is a multi-tyrosine kinase inhibitor that targets vascular endothelial growth factor receptor-2 (VEGFR-2), platelet-derived growth factor receptor (PDGFR), Raf-1, and c-kit. Sorafenib is the first molecular targeted agent which proved the survival benefit for advanced HCC in 2007. In the SHARP trial, a global phase 3 RCT, the median survival of HCC patients with portal vein tumor invasion or extrahepatic metastasis treated with sorafenib (400 mg, twice daily) was 10.7 months, which was significantly longer than the 7.9-month survival of patients who received a placebo (HR, 0.69; 95% CI, 0.55–0.87; P=0.0006) [790]. The TTP in the sorafenib group was 5.5 months, which was also significantly longer than the 2.8 months in the control group [790]. In the phase 3 RCT conducted in the Asia-Pacific region, including Korean patients with unresectable HCC (Asia-Pacific trial), the patients who received sorafenib had a significantly longer median survival period (6.5 months) compared to patients in the control group (4.2 months; HR, 0.68; 95% CI, 0.50–0.93; P=0.01) [791]. Both phase 3 trials (SHARP and Asia-Pacific trials) enrolled patients with preserved liver function (Child-Pugh class A) and adequate performance status (ECOG performance status of 0 to 2). Thereafter, sorafenib was given as a comparator in seven global RCTs for advanced HCC. The median OS of sorafenib-treated patients was more than 10 months (range, 8.5–14.7 months), longer than that of earlier studies [792-798].
Sorafenib was administered only for Child-Pugh class A patients; however, real-world retrospective studies have reported comparable TTP and safety between Child-Pugh class A and Child-Pugh class B patients [799-806]. The OS was shorter in Child-Pugh class B patients, and the presence of ascites was significantly associated with worse prognosis among the Child-Pugh class B patients [807]. Underlying liver function may have contributed to the shorter OS in Child-Pugh class B patients compared to Child-Pugh class A patients since they showed similar TTP. According to a large-scale observational study on 3,371 sorafenib-treated patients from 39 countries, the overall serious adverse events (SAEs) occurred more frequently in Child-Pugh class B patients (60%) than in Child-Pugh class A patients (36%). Within Child-Pugh B patients, Child-Pugh class B8–9 patients (69%, 67%) experienced SAEs more frequently than Child-Pugh class B7 patients (54%). However, the incidence of treatment-related SAEs was not significantly different between Child-Pugh class A (9%) and Child-Pugh class B patients (14%) [808]. The median OS was different according to Child-Pugh class: 13.6 months for class A, 6.2 months for B7, 4.8 months for B8, and 3.7 months for B9 [808]. Collectively, sorafenib can be considered with caution for patients with liver dysfunction (i.e., Child-Pugh B patients). However, meticulous follow-up is required, since liver-related adverse events tend to occur frequently in Child-Pugh class B patients [801,803]. Careful selection and close monitoring of Child-Pugh class B8/9 patients are necessary, as only limited studies are available so far. Further interventional studies are warranted to determine the optimal use of sorafenib in these patients.
The most common adverse events related to sorafenib treatment are HFSR and diarrhea; other common adverse events include fatigue, skin rash, hypertension, dysphonia, anorexia, weight loss, constipation, and alopecia. HFSR tends to resolve spontaneously after 3 months of treatment; therefore, it is important to continue therapy with patient education and proper management [809]. Since HFSR and hypertension have been reported as potential surrogate predictors of a good response to sorafenib, the management of adverse events needs to be emphasized to clinicians and patients [810]. Creams containing urea may help prevent dryness of the hands and feet. It is recommended that patients remove thick calluses, wear comfortable shoes with cushioning, avoid bathing with hot water, and take analgesics, if necessary, to mitigate and alleviate the symptoms associated with HFSR [809]. An open randomized controlled study reported that urea-containing cream significantly decreased the incidence of HFSR in sorafenib-treated patients [811]; however, another randomized placebo-controlled trial failed to reach statistical significance [812].
Lenvatinib
Lenvatinib is an oral multi-kinase inhibitor targeting VEGFR-1/2/3, fibroblast growth factor receptor (FGFR)-1/2/3/4, PDGFRα, RET, and C-kit. In a global randomized controlled non-inferiority phase 3 trial (REFLECT trial), lenvatinib demonstrated non-inferior OS to sorafenib in advanced HCC patients with a tumor occupying less than 50% of the liver and no bile duct or main portal vein invasion, who had preserved liver function (Child-Pugh class A) and ECOG performance status of 0 or 1 (HR, 0.92; 95% CI, 0.79–1.06) [796]. It was the first drug in 10 years since sorafenib to be approved for the treatment of advanced HCC. Median OS was 13.6 months (95% CI, 12.1–14.9 months) for patients taking lenvatinib (12 mg [weight ≥60 kg] or 8 mg [weight <60 kg] once daily) and 12.3 months (95% CI, 10.4–13.9 months) for patients taking sorafenib. PFS and TTP, both secondary endpoints, were significantly longer in the lenvatinib group than in the sorafenib group (PFS: 7.4 vs. 3.7 months; HR, 0.66; 95% CI, 0.57–0.77; P<0.00001; TTP: 8.9 vs. 3.7 months; HR, 0.63; 95% CI, 0.53– 0.73; P<0.0001). In the masked independent imaging review according to RECIST 1.1, the ORR was significantly higher in the lenvatinib group (18.8%; CR, <1%; PR, 18%) than in the sorafenib group (6.5%; CR, <1%, PR, 6%) (OR, 3.34; 95% CI, 2.17–5.14; P<0.0001).
SAEs were significantly more frequent in the lenvatinib group than in the sorafenib group (43% vs. 30%) [796]. HFSR was less frequent in the lenvatinib group (27%) than in the sorafenib group (54%), and hypertension was more frequent in the lenvatinib group (42%) than in the sorafenib group (30%). Other adverse events frequently observed in the lenvatinib group were diarrhea (39%), anorexia (34%), weight loss (31%), fatigue (30%), proteinuria (25%), and hypothyroidism (16%). It is recommended to interrupt lenvatinib if 24-hour urinary protein is ≥2 g. If a dipstick proteinuria result of 2+ or more is detected, a random urinary protein to creatinine ratio can be used to monitor proteinuria before further testing with the 24-hour urinary protein [813,814]. Thyroid stimulating hormone (TSH) levels should be monitored. If the TSH level is higher than 10 mIU/L or higher than 5 mIU/L on two separate occasions, consultation with an endocrinologist should be considered [814,815]. Hypertension or HFSR has been reported as a predictor of better prognosis, and the OS in patients who discontinued lenvatinib due to SAEs was significantly shorter than those who continuously received treatment [816]. When patients were divided into those with objective response and those without, relative dose intensity was significantly higher in patients showing objective response to lenvatinib [817]. Patients with low relative dose intensity (≤70%) demonstrated significantly shorter PFS [818]; therefore, proper management of adverse events is important to continue systemic therapy.
Real-world studies included patients who did not meet the REFLECT criteria, and PFS or ORRs were comparable between patients who met the REFLECT criteria and those who did not [819-822]. No significant differences were observed in the PFS or ORRs for patients receiving lenvatinib as a first-line or a later-line therapy [819,823]. Meanwhile, in another study, ORRs were lower in patients with Child-Pugh class B, and patients with Child-Pugh class B or beyond the REFLECT criteria showed shorter OS regardless of objective response [823,824]. Some studies reported comparable incidence of adverse events in those patients [820-822]; however, others reported that adverse events, such as liver-related adverse events, were more frequent in patients with Child-Pugh class B [819,824]. Collectively, lenvatinib can be considered for patients who do not meet the REFLECT criteria (Child-Pugh class B, tumor occupying >50% of liver, invasion of main portal vein or bile duct, history of prior systemic therapy, etc.); however, careful monitoring of Child-Pugh class B patients is required. Further studies are warranted.
Atezolizumab plus bevacizumab
Atezolizumab is an immune checkpoint inhibitor and a humanized IgG1 monoclonal antibody binding to PD-L1 that can be administered intravenously. Bevacizumab is a molecular targeted agent, an intravenous IgG1 monoclonal antibody binding to VEGF. In a global phase 3 RCT (IMbrave150) comparing atezolizumab plus bevacizumab (atezolizumab 1,200 mg + bevacizumab 15 mg/kg every 3 weeks) and sorafenib in patients with advanced HCC, atezolizumab plus bevacizumab significantly improved the OS and PFS [797]. The IMbrave150 study enrolled patients with treatment-naïve advanced HCC who had Child-Pugh class A and ECOG performance status 0 or 1; however, it excluded patients with autoimmune diseases (except autoimmune-related hypothyroidism on thyroid-replacement hormone, type 1 diabetes mellitus on insulin therapy, and autoimmune-related skin diseases with dermatologic manifestations only), treatment with immunosuppressive medication, history of organ or allogeneic stem cell transplantation, inadequately controlled hypertension, gastroesophageal varices incompletely treated or with high-risk for bleeding, and current or recent use of anti-platelet agents, anti-coagulants, or thrombolytic agents for therapeutic purpose.
The median PFS, a co-primary endpoint, was significantly longer with atezolizumab plus bevacizumab (6.8 months; 95% CI, 5.7–8.3) than sorafenib (4.3 months; 95% CI, 4.0–5.6; HR, 0.59; 95% CI, 0.47–0.76; P<0.001) [797]. The median OS, another co-primary endpoint, was also significantly improved by atezolizumab plus bevacizumab (not evaluable) compared to sorafenib (13.2 months; 95% CI, 10.4 to not evaluable; HR, 0.58; 95% CI, 0.42–0.79; P<0.001). The median OS of the atezolizumab plus bevacizumab group was not reached at the time of publication. The ORR, a secondary endpoint, was 27.3% (CR, 5.5%; PR, 21.8%) in the atezolizumab plus bevacizumab group, significantly higher than that in the sorafenib group (11.9%; CR, 0%; PR, 11.9%). The disease control rate (DCR) was 73.6% and 55.3% in the atezolizumab plus bevacizumab group and the sorafenib group, respectively [797].
The most frequent adverse event of the atezolizumab plus bevacizumab group was hypertension (29.8% vs. 24.4% in the sorafenib group). Fatigue (20.4% vs. 18.6%), proteinuria (20.1% vs. 18.6%), elevated AST (19.5% vs. 16.7%), and pruritus (19.5% vs. 9.5%) were more frequently observed in the atezolizumab plus bevacizumab group than in the sorafenib group, while diarrhea (18.8% vs. 49.4%) and anorexia (17.6% vs. 24.4%) were less frequently observed in the atezolizumab plus bevacizumab group than in the sorafenib group [797]. Hypothyroidism (10.9%) and pneumonitis (1.2%) were also reported. Although patients at high risk for bleeding were excluded from the IMbrave150 trial, the incidence of upper gastrointestinal bleeding was high in the atezolizumab plus bevacizumab group (7% vs. 4.5%) [797]. Therefore, patients at high risk for bleeding should be evaluated for gastroesophageal varices by esophagogastroduodenoscopy and be managed before initiating atezolizumab plus bevacizumab therapy.
SAEs occurred more frequently in the atezolizumab plus bevacizumab group than in the sorafenib group (38.0% vs. 30.8%); however, treatment-related grade 5 adverse events were less frequent in the atezolizumab plus bevacizumab group (4.6% vs. 5.8%).
A recent real-world study reported that a history of prior systemic therapy did not have a significant effect on the incidence of adverse events; however, additional studies are warranted since there are conflicting results on the treatment response [825,826].
Durvalumab plus tremelimumab
Tremelimumab is an immune checkpoint inhibitor and an intravenous fully human IgG2 monoclonal antibody that binds to CTLA-4 expressed on T cells. Durvalumab is another immune checkpoint inhibitor, a fully human IgG1 monoclonal antibody binding to PD-L1 that can be administered intravenously. A global, multicenter, open-label phase 1/2 trial evaluated the safety and efficacy of tremelimumab plus durvalumab, tremelimumab monotherapy, and durvalumab monotherapy. The ORRs were relatively high, 24.0% in patients receiving tremelimumab (300 mg, one dose) plus durvalumab (1,500 mg every 4 weeks) and 10.6% in patients receiving durvalumab monotherapy (1,500 mg every 4 weeks), respectively [827]. Dermatologic adverse events, such as pruritus and rash, were frequently observed (pruritus, 32.4% in the tremelimumab plus durvalumab group and 10.9% in the durvalumab monotherapy group; rash, 32.4% in the tremelimumab plus durvalumab group and 6.9% in the durvalumab monotherapy group) [827].
In a global multicenter phase 3 RCT (HIMALAYA), the primary endpoint was met, and it was demonstrated that tremelimumab (300 mg, one dose) plus durvalumab (1,500 mg every 4 weeks) significantly improved the OS over sorafenib (median, 16.43 vs. 13.77 months; HR, 0.78; 96% CI, 0.65–0.92; P=0.0035). OS with durvalumab monotherapy (1,500 mg every 4 weeks) was noninferior to sorafenib (median, 16.56 vs. 13.77 months; HR, 0.86; 96% CI, 0.73–1.03). The median PFS was not significantly different between the groups: 3.78 months in the tremelimumab plus durvalumab group, 3.65 months in the durvalumab monotherapy group, and 4.07 months in the sorafenib group. The ORRs were 20.1% in the tremelimumab plus durvalumab group, 17.0% in the durvalumab monotherapy group, and 5.1% in the sorafenib group. The DCRs were 60.1% in the tremelimumab plus durvalumab group, 54.8% in the durvalumab monotherapy group, and 60.7% in the sorafenib group. Treatment-related grade 3/4 adverse events occurred in 17.5% of the tremelimumab plus durvalumab group, 8.2% of the durvalumab monotherapy group, and 9.4% of the sorafenib group. Adverse events, such as esophageal variceal bleeding, did not occur [828].
Others
Nivolumab is an immune checkpoint inhibitor, a human IgG4 monoclonal antibody binding to programmed cell death protein-1 (PD-1) receptor expressed on T cells that can be intravenously administered and restore impaired anti-cancer activity. In a global phase 3 RCT comparing nivolumab and sorafenib (CheckMate 459) in patients with advanced HCC, the primary endpoint was not met with the median OS of 16.4 months (95% CI, 13.9–18.4) in the nivolumab group and 14.7 months (95% CI, 11.9–17.2) in the sorafenib group (HR, 0.85; 95% CI, 0.72–1.02; P=0.075) [798]. Nivolumab monotherapy can be considered for patients with contraindications for tyrosine kinase inhibitor, high-risk of bleeding, or anticoagulant users; however, with the success of tremelimumab plus durvalumab therapy, nivolumab monotherapy is expected to play a very limited role.
Donafenib is a multikinase inhibitor and a modified sorafenib derivative. In an open-label phase 2/3 RCT, donafenib significantly improved the OS, the primary endpoint, over sorafenib (12.1 vs. 10.3 months; HR, 0.831; 95% CI, 0.699–0.988; P=0.0245); however, there was no significant difference between donafenib and sorafenib in the PFS (3.7 vs. 3.6 months, P=0.0570) and ORR (4.6% vs. 2.7%, P=0.2448) [829]. Drug-related grade 3 or more adverse events occurred in significantly fewer patients who received donafenib than in patients who received sorafenib (38% vs. 50%, P=0.0018); however, this trial was limited as it was conducted in a single country.
Another randomized, open-label, multicenter, phase 2–3 study demonstrated that sintilimab (PD-1 inhibitor) plus bevacizumab biosimilar (IBI305) significantly improved the median PFS (4.6 vs. 2.3 months; HR, 0.56; 95% CI, 0.46–0.70; P<0.0001) and OS (median not reached; HR, 0.57; 95% CI, 0.43–0.75; P<0.0001) compared to sorafenib. However, the trial was also limited in that it was conducted in a single country [829].
An interim analysis of a global multicenter phase 3 RCT comparing atezolizumab plus cabozantinib and sorafenib reported that PFS, the primary endpoint, was significantly longer with atezolizumab plus cabozantinib (6.8 vs. 4.2 months; HR, 0.64; 95% CI, 0.44-0.91; P=0.0012) compared to sorafenib; however, there was no statistically significant difference in the OS between the two groups (15.4 vs. 15.5 months; HR, 0.90; 95% CI, 0.69-1.18; P=0.438). Results of the final analysis are awaited [830].
Considerations in first-line therapies
Atezolizumab plus bevacizumab is recommended as a preferred first-line option since it proved superior efficacy over sorafenib. However, atezolizumab is an immune checkpoint inhibitor and patients with a history of stem cell or solid organ transplantation, and autoimmune diseases were excluded from the IMbrave150 trial [797,831]. Therefore there is no evidence for its use in such patients. Considering the adverse events of bevacizumab, a VEGF inhibitor, high-risk varices and inadequately controlled hypertension should be managed before initiating atezolizumab plus bevacizumab. Other first-line systemic agents should be considered for patients who are not adequately managed for varices, current or recent use of anti-platelet agents, anti-coagulants, or thrombolytic agents for therapeutic purposes. Durvalumab and tremelimumab are also immune checkpoint inhibitors, and caution should be taken for patients with a history of transplantation or autoimmune diseases as rejection occurred in 37.5% of LT recipients who were treated with immune checkpoint inhibitors, 75% of whom progressed to end-stage organ failure [832-834]. However, durvalumab plus tremelimumab appears to be safe, as it did not increase the risk of bleeding in the phase 3 RCT.
All phase 3 RCTs of first-line systemic therapy have been conducted in patients with Child-Pugh class A. Evidence is lacking for systemic therapy in patients with Child-Pugh class B; however, TTP or safety profiles have been reported to be comparable between patients with Child-Pugh class A and B in real-world studies [800-806,808]. Sorafenib can be considered for patients with Child-Pugh class B, and liver-related adverse events should be closely monitored for patients with Child-Pugh class B8–9.
HCC can be generally divided into virus-related and non-virus-related types, according to the etiology. A meta-analysis of three randomized controlled phase 3 clinical trials on immune checkpoint inhibitors found that patients with non-viral HCC did not benefit from immune checkpoint inhibitor therapy [797,798,835,836]. On the contrary, the response to molecular targeted therapy did not differ between patients with viral HCC and non-viral HCC [835]. The results of this meta-analysis may support the stratification of patients according to the etiology for systemic therapy; however, it was derived from a post-hoc analysis, and the survival benefit was also observed in patients with non-viral HCC in phase 3 clinical trial of durvalumab plus tremelimumab. Further prospective studies are warranted to confirm these findings. Sorafenib improved the OS in patients with HCV-related HCC [661,837]. Although the survival benefit was not observed in patients with HBV-related HCC who received sorafenib treatment, it should be taken into consideration that baseline HBV DNA titer was not investigated and antiviral therapy was not mandatory in those studies. Lenvatinib demonstrated longer PFS in patients with HBV-related HCC; however, the results of the post-hoc analysis should be carefully interpreted [796].
[Recommendations]
1. Atezolizumab plus bevacizumab or durvalumab plus tremelimumab is recommended for systemic treatmentnaïve patients with locally advanced unresectable or metastatic HCC not amenable to curative or loco-regional therapy who have Child-Pugh class A and ECOG performance status 0–1 (A1). If these two combination therapies cannot be applied, sorafenib or lenvatinib is recommended (A1).
2. Sorafenib is considered for patients with HCC who have Child-Pugh class B7 (B1) or B8–9 (B2) if other conditions listed in Recommendation 1 are met.
Second-line or subsequent systemic therapy after failure of first-line treatment (Table 9)
It has been approximately 15 years since sorafenib first demonstrated survival benefits over placebo in patients with unresectable HCC in 2007. Since then, there have been several prospective studies on the second-line or third-line treatments after sorafenib failure; and regorafenib, nivolumab plus ipilimumab, cabozantinib, ramucirumab, and pembrolizumab obtained the final approval, conditional approval, or prior authorization from the U.S. Food and Drug Administration (FDA) or the Korean Ministry of Food and Drug Safety. Meanwhile, there have been few studies on effective second-line treatment after the failure of lenvatinib, and atezolizumab plus bevacizumab, as these first-line treatments were approved more recently. Also, as the superiority of durvalumab plus tremelimumab treatment compared to sorafenib was reported very recently, there has been no study on the second-line treatment after durvalumab plus tremelimumab failure. Herein, second-line treatments after failure of first-line treatments, including sorafenib, lenvatinib, atezolizumab plus bevacizumab, and durvalumab plus tremelimumab, are described (Fig. 9).
Second-line systemic therapies after sorafenib failure
Sorafenib failure is generally defined as a progression of the pre-existing disease or an appearance of a new intrahepatic or extrahepatic lesion during sorafenib treatment, and various patterns of disease progression after sorafenib failure are associated with the prognosis [838]. As long-term administration of sorafenib is often limited by disease progression, adverse events, or deterioration in liver function, the median duration of sorafenib administration is reportedly as short as 12 weeks [800,839].
To develop a second-line systemic therapy for HCC patients who stopped sorafenib due to disease progression or adverse events, several phase 3 clinical trials have been conducted using targeted agents, such as brivanib, which inhibits FGF and VEGF [840]; everolimus, which is an mTORi [841]; ramucirumab, which blocks VEGF-2 [842]; and tivantinib, which is a non-selective c-Met inhibitor [843]. However, all of these new agents failed to show improved survival compared to placebo. Recently, several agents, including regorafenib, cabozantinib, pembrolizumab, and ramucirumab (only in patients with serum AFP ≥400 ng/mL), have shown survival benefits over placebo after sorafenib-failure [844-849].
Regorafenib
Regorafenib is an oral multikinase inhibitor that blocks the activity of protein kinases involved in angiogenesis, oncogenesis, metastasis, and tumor immunity. Although regorafenib has a similar molecular structure to sorafenib, it has a distinct molecular target profile [850-852]. An international phase 3 RCT was conducted to validate the efficacy and safety of regorafenib as a second-line therapy for HCC patients with Child-Pugh A liver function and an ECOG score 0–1 who progressed after sorafenib treatment. Only the participants who had tolerated sorafenib (≥400 mg/day for ≥20 days of last 28 days of treatment) were enrolled. They were randomly assigned to receive either regorafenib or placebo at a 2:1 ratio. Regorafenib improved OS with an HR of 0.63 (95% CI, 0.50–0.79; P<0.0001); median survival was 10.6 months (95% CI, 9.1–12.1 months) for regorafenib vs. 7.8 months (6.3–8.8 months) for placebo. Based on this result, regorafenib was the first drug to show an improvement in survival as a second-line systemic therapy [844]. The regorafenib group showed significantly longer median PFS by mRECIST compared to the placebo group (3.1 months [95% CI, 2.8–4.2 months] vs. 1.5 months [95% CI 1.4–1.6 months]; P<0.001). Median TTP by mRECIST was also significantly longer in the regorafenib group (3.2 months; 95% CI, 2.9–4.2 months) than in the placebo group (1.5 months; 95% CI, 1.4–1.6 months; P<0.001). The mean duration of regorafenib administration was 5.9 months, and that of sorafenib was 3.3 months. Grade 3 or 4 adverse events associated with regorafenib were hypertension (15%), HFSR (13%), fatigue (9%), and diarrhea (3%) [844].
Cabozantinib
Cabozantinib is an oral, molecular targeted agent which blocks MET, VEGFR-2, and RET. An international phase 3 RCT was conducted to validate the efficacy and safety of cabozantinib as a second- or third-line therapy in patients with advanced HCC who progressed on sorafenib treatment and had Child-Pugh A liver function and ECOG score 0–1. The enrolled patients had shown progressive diseases (PDs) despite undergoing one or two systemic therapies including sorafenib, prior to participating in the study. The primary endpoint was OS, and the secondary endpoint was PFS and ORR according to RECIST v1.1. Among all participants, 27% received two systemic therapies including sorafenib. The median OS in the cabozantinib group was 10.2 months, which was significantly longer than the 8.0 months in the control group (HR, 0.76; 95% CI, 0.63–0.92; P=0.0049). Thus, the clinical trial met the primary endpoint [845]. In subgroup analysis, among patients who experienced sorafenib only, the median OS in the cabozantinib group was 11.3 months, which was also significantly longer than the 7.2 months in the control group (stratified HR, 0.70; 95% CI, 0.55–0.88). According to RECIST v.1.1 criteria, the median PFS was longer in the cabozantinib group (5.2 months) than in the control group (1.9 months) (HR, 0.44; 95% CI, 0.36–0.52; P<0.001), and ORR was also higher in the cabozantinib group than in the control group (4% vs. 0.4%, P=0.009) [845]. The median duration of cabozantinib therapy was 3.8 months. The grade 3 or 4 adverse events observed were HFSR (17%), hypertension (16%), elevation of transaminase levels (12%), fatigue (10%), and diarrhea (10%) [845].
Ramucirumab
Ramucirumab is an intravenous monoclonal antibody targeting VEGFR-2. A phase 3 REACH RCT of ramucirumab as a second-line therapy for patients with advanced HCC who progressed on sorafenib treatment was conducted, but it failed to meet the primary endpoint of improvement in OS compared with control [842]. However, in a post-hoc subgroup analysis, the OS in patients with a serum AFP level ≥400 ng/mL was 7.8 months, which was significantly longer than the 4.2 months in the placebo group (HR, 0.67; 95% CI, 0.51–0.90). Based on this result, a subsequent phase 3 REACH-2 RCT with 2:1 assignment to ramucirumab or placebo for patients with serum AFP levels of ≥400 ng/mL was conducted [847]. The enrolled patients had progressive HCC even after sorafenib, or had stopped sorafenib due to adverse events. All patients had Child-Pugh class A liver function, ECOG score of 0-1, and serum AFP level of ≥400 ng/mL. The primary endpoint of the study was OS. The OS in patients who received 8 mg/kg of ramucirumab every 2 weeks was 8.5 months, which was significantly longer than the 7.3 months in the placebo group (HR, 0.71; 95% CI, 0.531–0.949; P=0.0199). Therefore, the trial met the primary endpoint. By RECIST v.1.1 criteria, the median PFS in the ramucirumab group was 2.8 months, which was also significantly longer than the 1.6 months in the control group (HR, 0.452; 95% CI, 0.339–0.603; P<0.0001). The DCR in the ramucirumab and control group was 59.9% and 38.9%, respectively (P=0.0006); however, there was no difference in ORR between the two groups. The median duration of ramucirumab administration was 12 weeks, and the most common grade 3 or 4 adverse event was hypertension (12.2%). Other adverse events included hyponatremia (5.6%). Gastrointestinal bleeding occurred in 6% of the ramucirumab group, but it did not significantly differ from the placebo group (5%).
Nivolumab/ipilimumab
Nivolumab, a checkpoint inhibitor, is a fully human IgG4-type, monoclonal inhibitory antibody against PD-1. An international phase 1/2 uncontrolled trial on nivolumab for advanced HCC (CheckMate-040) involved patients with histologically confirmed HCC, compensated liver function (i.e., Child-Pugh score ≤6 for the dose expansion study and Child-Pugh score ≤7 for dose-escalation study), ECOG 0–1, and low serum HBV DNA level below 100 IU/mL (in case of HBV-related HCC) [853]. CheckMate-040 trial included a cohort, in which the primary endpoint was ORR (by RECIST v.1.1) and secondary endpoint included OS and DCR during intravenous nivolumab treatment (3 mg/kg, every 2 weeks) to 145 patients with either sorafenib failure or intolerance (132 patients with sorafenib failure and 12 patients with sorafenib intolerance). In this cohort, ORR was 20% (95% CI, 15–26%), median duration of response (DOR) was 9.9 months, and 12-month survival rate was 60% (95% CI, 51.4–67.5%). Grade 3 or 4 AEs, including fatigue, pruritis, rash, and diarrhea, occurred in less than 2% of the patients [853]. In another cohort (cohort 5) of CheckMate-040 trial, when a fixed dose (240 mg every 2 weeks) of nivolumab was administered to 49 patients (25 sorafenib-naïve and 24 sorafenib-experienced patients) with advanced HCC and Child-Pugh class B7–8, ORR was 12% (6 of 49; 95% CI, 5–25%) and DCR was 55% (95% CI, 40–69%). Twenty-five patients (51%) reported treatment-related adverse event (TRAE) and two (4%) discontinued treatment owing to TRAE, which were comparable results to those in Child-Pugh class A patients [854].
Another cohort of CheckMate-040 trial evaluated the efficacy of nivolumab in combination with ipilimumab, an inhibitor of CTLA-4, as a second-line treatment for patients with Child-Pugh class A liver function and ECOG 0–1 status who progressed on sorafenib treatment. In group A (n=49) to whom intravenous nivolumab 1 mg/kg and ipilimumab 3 mg/kg were administered every 3 weeks for four times and then nivolumab 240 mg was administered every 2 weeks, ORR by RECIST v.1.1 was 33% (n=16; 95% CI, 20–48%), median DOR (95% CI, 8.3 months–longer than 33.7 months) was not reached, and rates of TRAE was 94%, including one death by pneumonia [855]. Based on these results, the U.S. FDA conditionally approved the combination therapy with nivolumab 1 mg/kg and ipilimumab 3 mg/kg every 3 weeks for four times followed by nivolumab 240 mg every 2 weeks as the second-line treatment after sorafenib.
Pembrolizumab
Pembrolizumab is a humanized IgG4 anti-PD-1 monoclonal antibody that inhibits interaction between PD-1 and PD-L1/PD-L2. A phase 3 multicenter RCT (KEYNOTE-240) compared the OS and PFS between intravenous pembrolizumab (200 mg every 3 weeks), and placebo. This trial included 413 Child-Pugh class A and ECOG 0–1 patients who had previously underwent sorafenib treatment for advanced HCC. Patients were randomly assigned to the pembrolizumab or placebo group in a 2:1 ratio. Pembrolizumab treatment improved both the median OS (13.9 vs. 10.6 months; HR, 0.781; 95% CI, 0.611–0.998; P=0.0238) and PFS by RECIST v.1.1 (3.0 vs. 2.8 months; HR, 0.718; 95% CI, 0.570–0.904; P=0.0022) compared to the placebo, which, however, failed to reach the prespecified superiority margin (P=0.002 in the final analysis). ORR was significantly higher in the pembrolizumab group than in the placebo group (18.3% vs 4.4%, P=0.00007). Grade 3/4 AEs occurred in 52.7% in the pembrolizumab group and 46.3% in the placebo group. Common grade 3/4 AEs in the pembrolizumab group included elevations of AST (13.3%), bilirubin (7.5%), and ALT (6.1%), which occurred in 7.5%, 5.2%, and 3.0% of the placebo group, respectively [836]. In a post hoc analysis of KEYNOTE-240 trial including Asian patients, the pembrolizumab group showed significantly longer OS (median, 13.8 vs. 8.3 months; HR, 0.55; 95% CI, 0.37–0.88; P=0.0009) and PFS (median, 2.8 vs. 1.4 months; HR, 0.48; 95% CI, 0.32–0.72; P<0.0001). ORR was significantly higher in the pembrolizumab group (20.6% vs. 2.0%; P=0.0014) [854]. The U.S. FDA conditionally approved pembrolizumab as a second-line treatment for HCC.
Recently, the abstract of KEYNOTE-394 trial, which investigated the efficacy and safety of intravenous pembrolizumab (300 mg every 3 weeks, n=300) versus placebo (n=153) in 453 Asian patients was presented. The indication criteria of this trial were patients who had baseline Child-Pugh A liver function and ECOG score 0–1, and progression on oxaliplatinbased cytotoxic chemotherapy or sorafenib treatment for BCLC stage C HCC, HCC ineligible for curative treatment or HCC ineligible or refractory to local treatment. The primary endpoint was OS, and pembrolizumab treatment significantly improved OS (median, 14.6 vs. 13.0 months; HR, 0.79; 95% CI, 0.63–0.99; P=0.018). TTP by RECIST v.1.1 was significantly longer in the pembrolizumab group (median, 2.7 vs. 1.7 months; HR, 0.72; 95% CI, 0.58–0.90). ORR was 13.7% in the pembrolizumab group and 1.3% in the placebo group. The median DOR was 23.9 months in the pembrolizumab group and 5.6 months in the placebo group [846].
Miscellaneous agents: apatinib and camrelizumab
Apatinib is a tyrosine kinase inhibitor that inhibits VEGFR-2. In a Chinese phase 3 RCT (AHELP trial), 400 HCC patients who failed one or more systemic therapies (including oxaliplatinbased cytotoxic chemotherapy as well as molecularly targeted agent, such as sorafenib) were assigned to the apatinib group (oral apatinib 750 mg everyday) or placebo group in a 2:1 ratio. As patients were stratified according to sorafenib treatment, the proportions of patients who had experienced sorafenib were identical (41%) between the two groups. Both OS (median, 8.7 vs. 6.8 months; HR, 0.785; 95% CI, 0.617–0.998; P=0.048) and PFS (median, 4.5 vs. 1.9 months; HR, 0.471; 95% CI, 0.369–0.601; P<0.0001) were significantly longer in the apatinib group. ORR was 11% in the apatinib group and 2% in the placebo group. The most common grade 3/4 AEs were hypertension (28%), HFSR (18%), and thrombocytopenia (13%) in the apatinib group, which developed in 2%, 0%, and 1%, respectively, in the placebo group [856]. In this trial, 9% of the apatinib group and 10% of the placebo group died of AEs, although the investigators regarded all deaths as being unrelated to treatment.
Camrelizumab is a humanized anti-PD-1 monoclonal antibody. In a multicenter phase 2 open-label RCT, 220 Chinese patients who failed previous systemic treatment were assigned to intravenous camrelizumab 3 mg/kg every 2 weeks or every 3 weeks in a 1:1 ratio. ORR was 14.7% (95% CI, 10.3–20.2%), and the 6-month survival rate was 74.4% (95% CI, 68.0–79.7 months) [857].
Selection of second-line treatment
There has been no head-to-head comparison of the efficacy among second-line treatments after sorafenib failure. Instead, a network meta-analysis of previous phase 3 trials indirectly compared the efficacy of four second-line agents (regorafenib, cabozantinib, pembrolizumab, and ramucirumab). In the network meta-analysis, all of the included agents showed significantly longer PFS compared to the placebo (for regorafenib: HR, 0.46 [95% CI, 0.37–0.57]; for cabozantinib: HR, 0.44 [95% CI, 0.37–0.53]; for pembrolizumab: HR, 0.72 [95% CI, 0.57–0.90]; and for ramucirumab: HR, 0.62 [95% CI, 0.52–0.74]). However, only regorafenib (HR, 0.62; 95% CI, 0.51–0.75) and cabozantinib (HR, 0.76; 95% CI, 0.63–0.92) significantly prolonged OS [848]. In comparison of each of the agents, regorafenib had significantly longer PFS than either pembrolizumab (HR, 0.64; 95% CI, 0.47–0.87) or ramucirumab (HR, 0.74; 95% CI, 0.56–0.98). Cabozantinib showed significantly longer PFS than either pembrolizumab (HR, 0.61; 95% CI, 0.46–0.82) or ramucirumab (HR, 0.71; 95% CI, 0.55–0.92) [848]. There was no significant difference in PFS between the other agents. In terms of OS, regorafenib was superior to ramucirumab (HR, 0.71; 95% CI, 0.54–0.93). There was no significant difference in OS between the other agents. However, among patients with serum AFP ≥400 ng/mL, in whom ramucirumab is indicated, either regorafenib or cabozantinib was not superior to ramucirumab in terms of both PFS and OS [848].
Several retrospective studies comparing the efficacy of second-line treatments after sorafenib failure were conducted in South Korea. A single-center study involving 102 patients treated with regorafenib and 48 patients with nivolumab as a second-line treatment after sorafenib failure reported that nivolumab treatment was an independent prognostic factor for longer survival (aHR, 0.54; 95% CI, 0.30–0.96; P=0.04) in multivariable analysis, although there was no significant difference in OS (6.9 vs. 5.9 months, log-rank P=0.88) in univariable analysis [858]. In contrast, another single-center retrospective study involving 223 patients treated with regorafenib and 150 with nivolumab as a second-line treatment after sorafenib failure reported that there was no difference in both PFS (HR, 0.85; 95% CI, 0.69–1.06; P=0.15) and OS (HR, 0.83; 95% CI, 0.64–1.07; P=0.15) between the two treatments. The results were consistent in multivariable analysis, propensity score-matching analysis, and inverse probability treatment weighting analysis [859].
To select second-line or subsequent systemic treatments, physicians may refer to the aforementioned studies. However, further studies are warranted.
Second-line treatment after lenvatinib failure
As lenvatinib has been used as a first-line treatment for unresectable HCC in clinical practice from late 2018, only a few small-scale retrospective studies on the second-line treatment after lenvatinib failure are available.
A post hoc analysis of phase 3 REFLECT study reported that, at the time of discontinuation of lenvatinib in 451 patients, 36.6%, 48.8%, 9.3%, and 4.9% were ECOG 0, 1, 2, and 3 or 4, respectively, and 75.2%, 21.5%, and 2.9% were Child-Pugh class A, B, and C, respectively. In 156 patients who underwent any subsequent systemic therapy after lenvatinib treatment, the median OS was 20.8 months. Among them, 43 responders to lenvatinib showed a median OS of 25.7 months. Subsequent anticancer medications included sorafenib (32.6%), fluorouracil (4.2%), cisplatin (3.8%), investigational immunotherapies (3.1%), and oxaliplatin (2.9%). In contrast, in 332 patients who underwent no systemic treatment or were not able to receive any systemic treatment, the median OS was merely 11.5 months. These findings support that subsequent systemic treatment may be associated with longer OS [860].
In a retrospective study, among 105 patients who received lenvatinib treatment as a first-line treatment for HCC, 28 patients underwent second-line treatment. In this study, subsequent treatment with molecular targeted agent was an independent prognostic factor for longer OS (aHR, 0.299; 95% CI, 0.120–0.746; P=0.012) [861]. In another Japanese multicenter retrospective study involving 69 patients who underwent second-line treatment after lenvatinib failure, 53 patients (76.8%) received sorafenib and 22 patients received regorafenib as a second- or third-line treatment. In sorafenibtreated patients, the median PFS was 1.8 months and the ORR was 1.8%. In regorafenib-treated patients, the median PFS was 3.2 months and the ORR was 13.6% [862]. In a retrospective study, 28 patients who underwent ramucirumab treatment after lenvatinib failure in 16 centers in Japan were included. Among them, 14, 9, and 5 patients utilized ramucirumab as a second-, third-, and fourth-line treatment, retrospectively. Their median PFS was 2.0 months, ORR was 3.8% and, DCR was 42.3% [863].
Based on the results of aforementioned retrospective studies, for patients with lenvatinib failure, sorafenib and some second-line agents approved for sorafenib failure (i.e., regorafenib, cabozantinib, and ramucirumab [for patients with serum AFP ≥400 ng/mL]) can be considered. Although further studies are required, theoretically, treatments including immune checkpoint inhibitors (i.e., atezolizumab plus bevacizumab, nivolumab plus ipilimumab, nivolumab, and pembrolizumab) can also be considered. In addition, participation in the clinical trials on second-line treatment after lenvatinib failure may be considered.
Second-line treatment after atezolizumab/bevacizumab failure
As combination therapy with atezolizumab and bevacizumab has been used as a first-line treatment for unresectable HCC in clinical practice from early 2020, only a few small-scale retrospective studies on second-line treatment after atezolizumab/bevacizumab failure are available.
A recent multinational retrospective study involved 49 patients who underwent second-line treatment after atezolizumab/bevacizumab combination therapy. All the included patients received multikinase inhibitors: 29 patients, 19 patients, and one patient received sorafenib, lenvatinib, and cabozantinib, respectively. Their median PFS was 3.4 months, and the median OS was 14.7 months. The lenvatinib group had significantly longer PFS compared to the sorafenib group (6.1 vs. 2.5 months, P=0.004), but showed comparable OS (16.6 vs. 11.2 months, P=0.347) [784].
For patients with atezolizumab/bevacizumab failure, sorafenib, lenvatinib, some second-line agents approved for sorafenib failure (i.e., regorafenib and cabozantinib), and immune checkpoint inhibitors with different targets (i.e., combination therapies with nivolumab plus ipilimumab and durvalumab plus tremelimumab) can be considered, although further studies are required. Regorafenib and cabozantinib, which demonstrated survival benefits as a second- or third-line treatment in patients previously exposed to VEGF inhibitors (e.g., sorafenib), may be theoretically preferred after atezolizumab/bevacizumab failure over sorafenib and lenvatinib, which are proven first-line systemic therapies in patients who are VEGF inhibitors-naïve. However, further studies are warranted [848]. In addition, participation in the clinical trials on second-line treatment after atezolizumab/bevacizumab failure may be considered.
Second-line treatment after durvalumab/tremelimumab failure
As a recent phase 3 RCT reported that the combination therapy with durvalumab plus tremelimumab resulted in a longer OS compared to sorafenib as a first-line treatment for unresectable HCC [828], approval by the U.S. FDA for commercial use is expected. Although there has been no report so far, sorafenib, lenvatinib, regorafenib, cabozantinib, ramucirumab (patients with serum AFP ≥400 ng/mL), and atezolizumab/bevacizumab can be considered as a second-line treatment for patients with durvalumab/tremelimumab failure. In addition, participation in the clinical trials on second-line treatment after durvalumab/tremelimumab failure may be considered.
[Recommendations]
1. Regorafenib is recommended for patients with progressive HCC after at least 3 weeks of sorafenib (≥400 mg/day) treatment and with Child-Pugh class A and good performance status (ECOG score 0–1) (A1).
2. Cabozantinib is recommended for patients with progressive HCC after first-line sorafenib or second-line systemic treatment and with Child-Pugh class A and good performance status (ECOG score 0–1) (A1).
3. Ramucirumab is recommended for patients with progressive HCC after sorafenib or intolerance to sorafenib and with Child-Pugh class A, good performance status (ECOG score 0–1), and serum AFP level ≥400 ng/mL (A1).
4. Pembrolizumab is recommended for patients with progressive HCC after sorafenib or intolerance to sorafenib and with Child-Pugh class A and good performance status (ECOG score 0–1) (B1).
5. Either nivolumab plus ipilimumab combination therapy (B1) or nivolumab monotherapy (C1) can be considered for patients with progressive HCC after sorafenib or intolerance to sorafenib and with Child-Pugh class A and good performance status (ECOG score 0–1).
6. Sorafenib, regorafenib, cabozantinib, ramucirumab (if serum AFP level ≥400 ng/mL), atezolizumab-bevacizumab, durvalumab-tremelimumab, pembrolizumab, nivolumab-ipilimumab, or nivolumab treatment can be tried for patients with progressive HCC after lenvatinib (D1).
7. Sorafenib, lenvatinib, regorafenib, cabozantinib, durvalumab-tremelimumab, or nivolumab-ipilimumab can be tried for patients with progressive HCC after combination therapy with atezolizumab plus bevacizumab (D1).
8. Sorafenib, lenvatinib, regorafenib, cabozantinib, ramucirumab (if serum AFP level ≥400 ng/mL), or atezolizumab-bevacizumab can be tried for patients with progressive HCC after combination therapy with durvalumab plus tremelimumab (D1).
Cytotoxic chemotherapy and hepatic arterial infusion chemotherapy
Cytotoxic chemotherapy can be considered for patients with HCC [864-866]. However, in most cases, HCC is accompanied by liver cirrhosis, which affects the absorption and metabolism of anticancer drugs, making it impossible to administer a therapeutic dose, and resulting in an increased risk of cytotoxic chemotherapy-related toxicity [867,868]. Fluorouracil, leucovorin, and oxaliplatin (FOLFOX) combination therapy has been studied in a multicenter RCT (EACH study) including 317 Asian patients, but the control arm was doxorubicin monotherapy [869]. To date, there has been no cytotoxic chemotherapy regimen that showed superiority or non-inferiority to sorafenib, lenvatinib, or atezolizumab-bevacizumab combination therapy, which are the currently available options for first-line treatment. Cytotoxic chemotherapy has been studied as a rescue regimen for patients who progressed on first-line sorafenib treatment [870]; and yet, there has been no cytotoxic chemotherapy regimen that demonstrated superiority or non-inferiority to regorafenib or cabozantinib, which have shown benefits for patients who failed the first- or second-line systemic treatment in RCTs. Hence, cytotoxic chemotherapy should be considered for patients with preserved liver function and good performance status who failed or cannot use first- or second-line systemic treatments, such as sorafenib, lenvatinib, regorafenib, cabozantinib, ramucirumab, nivolumabipilimumab, or pembrolizumab after careful individualized assessment on the risk and benefit of cytotoxic chemotherapy. Care must be taken to avoid inadvertently worsening the patient’s quality of life.
HAIC is a type of cytotoxic chemotherapy that involves direct injection of the cytotoxic anticancer drugs into the hepatic artery, thereby causing fewer adverse systemic reactions, while exposing HCC to high concentrations of anticancer drugs. The most commonly used drug in HAIC therapy is 5-fluorouracil, which is used alone or in combination with cisplatin. The ORR of HAIC is 3.8–38.5%, with a PR of 7–81% and a median survival period of 5.0–19.5 months [871-875]. In observational studies that compared the efficacy of HAIC to sorafenib in advanced HCC, HAIC showed better outcomes compared to sorafenib in some studies [876-880], while other studies showed no difference between HAIC and sorafenib therapies [881]. In a RCT conducted in South Korea that directly compared HAIC and sorafenib in 58 patients with advanced HCC and major portal vein invasion (PVI), the OS was better in the HAIC group than in the sorafenib group (14.9 vs. 7.2 months; HR, 0.32; 95% CI, 0.15–071) [882]. However, the sample size was small and only advanced patients with major PVI were included. Recently, a RCT conduced in China was reported (FOHAIC-1), in which 262 patients with advanced HCC were assigned HAIC and sorafenib in a 1:1 ratio. In this RCT, HAIC showed better OS compared to sorafenib (13.9 vs. 8.2 months; HR, 0.408; 95% CI, 0.301–0.552) [883]. In a multicenter retrospective observational study conducted in South Korea, HAIC was compared to lenvatinib in 244 patients with advanced HCC, and the results showed no difference in the OS between the HAIC and lenvatinib group (9.4 vs. 9.3 months, P=0.489) [884].
There have been several RCTs on the treatment outcomes of combination treatment of HAIC with sorafenib in advanced HCC, but the findings were inconsistent. In a phase 2 RCT of 108 patients with advanced HCC, the HAIC and sorafenib combination treatment had a longer OS compared to sorafenib monotherapy (10.6 vs. 8.7 months; HR, 0.60; 95% CI, 0.38–0.96) [885]. Meanwhile, in a phase 3 RCT of 205 patients with advanced HCC (SILIUS study), there was no difference in the OS between the HAIC and sorafenib combination treatment and the sorafenib monotherapy group (11.8 vs. 11.5 months; HR, 1.009; 95% CI, 0.743–1.371) [886]. In another RCT of 68 patients with advanced HCC (SCOOP-2 study), there was no difference in the OS between the sequential HAIC followed by sorafenib group and the sorafenib monotherapy group (10.0 vs. 15.2 months; HR, 1.08; 95% CI, 0.63–1.86) [887]. In a RCT of 247 patients with advanced HCC with PVI, survival was better in the HAIC and sorafenib combination group compared to the sorafenib monotherapy group (13.4 vs. 7.1 months; HR, 0.35; 95% CI, 0.26–0.48) [888]. In another RCT of 64 patients with advanced HCC with PVI, survival was better in the HAIC and sorafenib combination group compared to the sorafenib monotherapy group (16.3 vs. 6.5 months; HR, 0.28; 95% CI 0.15–0.53) [889]. There has been no RCT comparing the efficacy and safety of HAIC combination therapy to other systemic therapies. In a retrospective analysis of 170 patients with PD-L1 expressing unresectable HCC, combined treatment with pembrolizumab-lenvatinib and HAIC showed better survival compared to pembrolizumab-lenvatinib therapy [890]; and in another retrospective study of 157 patients with advanced HCC, the OS was better with lenvatinib-toripalimab and HAIC combination therapy compared to lenvatinib monotherapy [891]. Although HAIC is mainly used for the treatment of advanced HCC, HAIC was also studied in a RCT involving 315 unresectable HCC with maximal tumor size >7 cm but without major vascular invasion or extrahepatic spread (BCLC stage A or B). In this RCT, HAIC using FOLFOX showed better OS compared to TACE (23.1 vs. 16.1 months; HR, 0.58; 95% CI, 0.45–0.75) [892]. Therefore, there may be a group of patients for whom HAIC can be considered as a treatment option [636]; however, studies comparing the efficacy or safety of HAIC to first- or second-line systemic option, such as atezolizumab-bevacizumab, durvalumab-tremelimumab, lenvatinib, regorafenib, cabozantinib, ramucirumab, nivolumab-ipilimumab, and pembrolizumab, are still lacking. Therefore, HAIC might be considered on an individual basis for advanced HCC patients with portal vein invasion, preserved liver function, and without extrahepatic spread for whom first-line or second-line systemic treatment have failed or cannot be used.
[Recommendations]
1. HAIC may be considered for advanced HCC patients with preserved liver function and portal vein invasion without extrahepatic spread for whom first-line or second-line systemic therapies, such as atezolizumab-bevacizumab, durvalumab-tremelimumab, sorafenib, lenvatinib, regorafenib, cabozantinib, ramucirumab, nivolumab-ipilimumab, or pembrolizumab, have failed or cannot be used (C2).
Combination of local and systemic treatment for advanced HCC
There have been several RCTs on whether combining local and systemic treatment can improve the outcome of patients with advanced HCC. In a RCT that compared TARE and sorafenib combination treatment to sorafenib in 424 patients with advanced HCC, there was no difference in the OS between the two groups (12.1 vs. 11.4 months; HR, 1.01; 95% CI, 0.81–1.25) [636]. In a multicenter phase 3 RCT conducted in South Korea involving 339 patients with advanced HCC (STAH trial), sorafenib with concurrent cTACE failed to prolong the OS of advanced HCC patients compared to sorafenib (12.8 vs. 10.8 months; HR, 0.91; 95% CI, 0.69–1.21) [893]. However, combination treatment with sorafenib and concurrent cTACE significantly improved the secondary outcomes such as PFS, TTP, and tumor response rate compared to sorafenib monotherapy. Post hoc analysis showed that the OS was longer in the combination treatment group than in the sorafenib group if the patients received more than two sessions of cTACE (18.6 vs. 10.8 months; HR, 0.58; 95% CI, 0.40–0.82; P=0.006) [893]. There may be a subgroup of advanced HCC patients in which the combination of local and systemic treatment may offer survival benefits compared to systemic treatment only. However, further studies are needed to identify candidates for combination therapy and decide what would be the best combination out of many systemic treatment options and local treatment modalities. Recently, a phase 3 RCT comparing lenvatinib plus cTACE and lenvatinib monotherapy for patients with advanced HCC was presented as a meeting abstract [894], and reported better OS, better PFS, and ORR in the combination group. The final announcement is awaited. To date, no final data from a RCT has been reported on the efficacy and safety of combination treatment of systemic agents, other than sorafenib, and various local treatment modalities (cTACE, TARE, EBRT).
Management of patients with CR after systemic treatment
Due to the development of systemic treatments, CR is often observed after systemic treatment for advanced HCC. In a global phase 3 trial (IMbrave150 study), 0% of patients in the sorafenib group and 5.5% in the atezolizumab-bevacizumab group achieved a CR by the RECIST 1.1 criteria, and 1.9% in the sorafenib group and 10.2% in the atezolizumabbevacizumab group achieved a CR by the mRECIST criteria [797]. In patients with malignant melanoma treated by immunotherapy, durable CR after discontinuation of immunotherapy have been reported [895,896]. This suggests that the discontinuation of immune checkpoint inhibitor-based treatment may be possible for patients achieving CR. However, to date, there is no study that reported whether systemic treatment can be discontinued after achieving CR in advanced HCC patients. Considering the medical resources related to systemic treatment, additional studies on the management of patients with CR after systemic treatment are required.
Adjuvant therapy
Adjuvant therapy usually refers to additional treatment after curative therapy to prevent recurrence. As the 5-year recurrence rate even after curative resection for HCC is as high as 50–70%, effective adjuvant therapy is urgently required [249,897,898]. Although TACE [898,899], iodine-131 infusion therapy via the hepatic artery [900], vitamin K2 [901], or vitamin A analogues [902] have been tested as adjuvant therapies after curative treatment for HCC, no therapy has been validated. Cytotoxic chemotherapy or sorafenib also has failed to provide clinical evidence for adjuvant therapy [903,904]. Recently, randomized controlled phase 3 studies on adjuvant therapies after curative treatment using immune checkpoint inhibitors are underway, and the results are awaited [905].
After a Japanese study reported that adjuvant therapy of cytokine induced killer (CIK) cells reduced the 3-year HCC recurrence rate by up to 15% compared with control [906], several prospective RCTs have been conducted [907-911]. In a Korean phase 3 RCT, adjuvant therapy with CIK cells significantly improved the RFS (HR, 0.63; 95% CI, 0.43–0.94) and OS (HR, 0.21; 95% CI, 0.06–0.75) in patients with AJCC stage I or II HCC after curative resection or local ablative therapy (RFA or PEI) [908]. A subgroup analysis demonstrated that RFS was significantly improved only in patients with AJCC stage I HCC. An extended follow-up study (median, 68.5 months; interquartile range, 45.0–82.2) also showed a sustained improvement in both RFS (HR, 0.67; 95% CI, 0.48–0.94; P=0.009) and OS (HR, 0.33; 95% CI, 0.15–0.76, P=0.006) [912]. In a Korean real-world study using propensity score analysis, CIK adjuvant therapy significantly improved RFS (HR, 0.42; 95% CI, 0.22–0.80, P=0.006) [913]. In a cost-effectiveness analysis study based on the results of the randomized controlled study and the realworld study, the incremental cost-effectiveness ratio were $33,077/QALY (quality-adjusted life-year) and $25,107/QALY, respectively [814]. In a Chinese randomized controlled phase 3 trial, CIK cell treatment significantly prolonged the time-to-recurrence (13.6 months in the CIK group and 7.8 months in the control group, P=0.01); however, in this study, no statistically significant differences were observed in either RFS or OS [907]. A meta-analysis of the RCTs reported that adjuvant CIK cell therapy significantly improved RFS and OS up to 3 years in patients after curative treatment [914].
Although TACE can be applied prior to resection as a neoadjuvant therapy in patients with resectable HCC, no robust evidence support that TACE followed by resection improves the OS or DFS compared to resection only [313].
[Recommendations]
1. Adjuvant immunotherapy with CIK cells can be considered after curative treatment (resection, RFA, or PEI) in patients with HCC ≤2 cm without lymph node or distant metastasis (A2).
2. Adjuvant therapy with TACE, sorafenib, or cytotoxic chemotherapy is not recommended for patients with HCC after curative treatment (B1).
PREVENTIVE ANTIVIRAL THERAPY
HBV-related HCC
The rate of HBV reactivation following cytotoxic chemotherapy for HCC ranges widely from 30% to 60% [915,916], and the subsequent mortality rate is reported to be approximately 30% after HBV reactivation. Therefore, the test for HBsAg must be performed in all patients with HCC before cytotoxic chemotherapy. In patients with positive HBsAg, preventive antiviral drug should be administered before cytotoxic chemotherapy and maintained for at least 6 months after the end of cancer treatment. Interferon is not recommended as a preventive therapy due to the risk of bone marrow suppression and transient aggravation of hepatitis, and oral antiviral drugs are recommended instead. HBV reactivation has been reported in patients with HCC who test negative for HBsAg but positive for anti-HBc [917]; however, there is no strong evidence to recommend uniform preventive therapy for such cases. Preventive antiviral therapy during tyrosine kinase inhibitor treatment is currently controversial. A Korean retrospective study reported no HBV reactivation during sorafenib treatment [800], while another study reported a higher risk of HBV reactivation [918], suggesting the need for additional research. Immune checkpoint inhibitors increase immune responses against HBV, and thus may cause acute aggravation of hepatitis. Therefore, to maintain low HBV viral load during immune checkpoint inhibitor treatment, an effective antiviral drug should be co-administered. For this reason, clinical trials on immune checkpoint inhibitors have only included patients with low serum levels of HBV DNA [797,836,853]. A recent retrospective study of 60 HBV-related HCC patients who received immune checkpoint inhibitor treatments reported HBV reactivation and hepatitis in one out of six patients who did not receive preventive antiviral drugs [919].
Many studies have evaluated HBV reactivation during TACE, and it has been reported to occur in 4.3–40.5% of patients [920-923]. In a RCT that compared preemptive lamivudine treatment to an untreated control group during TACE, significant differences were observed with respect to HBV reactivation (2.8% and 40.5%), as well as the consequent occurrence of hepatitis (2.8% and 29.7%) and liver failure (0.0% and 8.1%) [923]. Another randomized trial reported a higher rate of undetected HBV DNA in the preventive lamivudine group compared to that in the control (45.6% vs. 11.2%, P<0.001), as well as longer TTP (8.2 vs. 4.3 months, P=0.005) and OS (RR, 0.423; 95% CI, 0.248–0.721; P=0.002) in the preventive lamivudine group [924]. An observational study compared preventive entecavir therapy with an untreated group and showed significant differences in the rates of virus-related events (6.8% vs. 54.4%, P=0.001) and acute decompensation (0% vs. 11.6%, P=0.039) between the two groups [925]. A recent retrospective propensity score-matching study involving 1,547 patients reported 1-, 2-, and 3-year HBV reactivation rates of 28.6%, 37.9%, and 44.2%, respectively, after TACE in patients who did not receive preventive antiviral therapy, and a significantly higher 10-year survival rate in the preventive antiviral therapy group (26.5% vs. 12.8%, P<0.0001) [926]. Therefore, the preventive use of antiviral drugs is necessary for HBV-related HCC patients who receive TACE.
HBV reactivation rates after HAIC for HCC (24% to 67%) are reported to be higher than those after TACE, which is possibly due to the higher dose of chemotherapeutic agents, as HAIC is carried out in shorter intervals [916,927,928]. However, more research is needed to support the claim that HAIC has a higher reactivation rate compared to TACE, as only a few studies with a limited number of participants have been reported and no comparative study with TACE has been performed.
Following the hepatic resection of HCC, HBV reactivation with concomitant elevation in the HBV DNA level or an abnormal biochemical liver function test was observed in 14–32% of the patients [929]. In a RCT that compared preventive telbivudine administration to an untreated control group from the day of resection, the HBV reactivation rates were 2.5% and 31.8%, respectively. In this study, 57.1% of the reactivation developed within 1 week after hepatic resection [930]. Also, in a RCT that compared preventive adefovir therapy to a control group after R0 resection, the 1-, 3-, and 5-year RFS rates were superior in the adefovir group compared to the control group (85.0%, 50.3%, and 46.1% vs. 84.0%, 37.9%, and 27.1%, respectively) [931]. The corresponding OS rates were also superior in the adefovir group (96.0%, 77.6%, and 63.1% vs. 94.0%, 67.4%, and 41.5%, respectively). The RRs of recurrence and death for antiviral treatment were 0.65 and 0.42, respectively. Antiviral therapy was an independent predictive factor of late tumor recurrence.
A study that compared preventive lamivudine administration and an untreated control group following EBRT for HCC reported the HBV reactivation rates to be 0% and 21.8%, respectively; meanwhile, ALT elevation occurred in 2.3% and 12.5% of the patients, respectively [932]. It has also been reported that the rate of HBV reactivation increases two-fold if TACE is performed in conjunction with EBRT, compared to TACE [933]. A recent retrospective study involving 133 patients reported HBV reactivation rates of 12.7% and 0% in the untreated and preventive antiviral group, respectively, following EBRT and 50% and 16.7%, respectively, following TACE plus EBRT [934].
There are limited studies on HBV reactivation following PEI or RFA; nonetheless, the HBV reactivation rates after RFA have been reported to be 5.6–9.1% [935,936].
Even in patients with positive HBsAg and undetectable HBV DNA, a few retrospective studies have reported a significant increase in the HBV reactivation rates following hepatic resection and TACE, and reactivation was shown to be associated with HCC recurrence [937] and OS [938]. A recent systemic review on HBV reactivation following HCC treatment classified TACE (19%), hepatectomy (16%), and EBRT (14%) as high-risk procedures with HBV reactivation rates greater than 10%, and tyrosine kinase inhibitor or immune checkpoint inhibitor therapy (7%) and RFA (7%) as moderate-risk procedures [939].
In patients with HBV-related HCC, HBV reactivation frequently develops after cancer treatment, and preventive antiviral treatment has been shown to effectively reduce the risk of reactivation, hepatitis, decompensation, and death. Therefore, the preventive use of oral nucleos(t)ide analogues should be actively considered before HCC treatment in patients with HBV-related HCC.
HCV-related HCC
In the case of HCV-related HCC, HCV reactivation and the resultant hepatitis may occur after HCC treatment; however, liver failure and death due to HCV reactivation are extremely rare. In a retrospective observational study reporting on HCV- or HBV-related HCC, the rates of reactivation, hepatitis, and liver failure were 26.5%, 10.2%, and 0% in the HCV group and 32.6%, 34.8%, and 10.9% in the HBV group, respectively [940]. Although there was no difference in the reactivation rate after TACE between the two groups, the HCV group had significantly lower rates of hepatitis and liver failure compared to the HBV group. Therefore, it is necessary to monitor patients with HCV-related HCC for HCV reactivation and hepatitis. However, since no study has assessed the effectiveness of preventive antiviral therapy using DAA in patients with HCV-related HCC, there is no evidence yet to recommend preventive antiviral therapy.
[Recommendations]
1. HCC Patients should be tested for hepatitis B surface antigen before starting HCC treatment (A1).
2. In HCC patients with HBV, antiviral therapy should be initiated if serum HBV DNA is detected (A1).
3. In HBsAg-positive HCC patients with undetectable serum HBV DNA, preventive antiviral therapy is recommended before cytotoxic chemotherapy (A1), TACE (A2), HAIC (A2), hepatic resection (A2), EBRT (B1), RFA (C1), tyrosine kinase inhibitor, or immune checkpoint inhibitor (C1) treatment.
4. Antiviral agents for the prevention of HBV reactivation should be selected based on the KASL clinical practice guidelines for management of chronic hepatitis B (A1).
5. There is still no evidence to recommend preventive antiviral therapy with DAAs for HCC patients who are HCV RNA positive (C1).
DRUG TREATMENT FOR CANCER PAIN IN HCC
Types of pain
Patients with HCC who experience cancer pain have a poorer quality of life and prognosis compared to those without cancer pain [941]. Understanding pain caused by HCC is not only important for the patient’s quality of life but also the prognosis. There are three types of pain caused by HCC: parietal or visceral pain, pain caused by metastasis to bone, and pain that occurs after HCC treatment.
First, parietal, or visceral pain is caused by inflammation along the intestinal walls. It manifests as abdominal pain that occurs due to the infiltration of the primary or metastatic lesion to the intestinal wall. Although such pain is reported to be induced by the interactions between the immune system, central and peripheral nerves, and tumor cells, the relative contribution of this pathophysiology to cancer pain is unknown. Peripheral inflammation and recurrent acute pain contribute to visceral hypersensitivity, while recurrent acute pain also induces the formation of synaptic connections and reinforces existing connections in the brain regions associated with pain. These structural and functional changes in the peripheral and central nervous systems induce chronic abdominal pain [942].
Second, nociceptive pain occurs as cancer cells metastasize to the bones. Nociceptive pain is accompanied by the complicated characteristics of inflammatory and neuropathic pain [943]. Rather than damaging the bones, cancer cells induce osteoclastic activation. Osteoclasts and the acidic environment of bones activate sensory nerves through the acid-sensing ion channels and transient receptor potential vanilloid receptor 1, thereby inducing pain. Chemical substances released by cancer cells, such as prostaglandins, and nerve growth factors stimulate and sensitize pain receptors in the bones, and tumors directly pressurize sensory nerve fibers to induce pain.
Third, treatment-induced pain includes PES, which occurs after hepatic artery embolization, as well as pain that occurs during or after RFA.
The prevalence of cancer pain is reported to be 45–53% [944-946]. Active palliative care including pain management from an early stage improves the quality of life [947-949] and survival [943,950] of patients with cancer. Although research on pain caused by HCC is rare, the prevalence of pain among patients with HCC is reported at 22–66.8% [941,945,951], indicating the need to consider pain management as an important part of palliative care for HCC. As HCC is mostly accompanied by liver disease or cirrhosis, patients with HCC may experience changes in their drug metabolism and more serious side effects from pain analgesics depending on the severity of liver dysfunction [952]. However, there is a lack of research on pain management for patients with liver disease [953] or HCC. Therefore, standard cancer treatment principles should be followed [954-956], but it is necessary to select the appropriate medications, and adjust doses and administration intervals with considerations for the patient’s underlying liver disease.
Principles of pain management
The fundamental principles of the analgesic ladder for pain management proposed by the WHO are to give drugs “by the clock,” “by the mouth,” and “by the ladder.” The same principles are commonly followed to manage cancer pain; patients are initiated on nonopioid analgesics, followed by weak opioids and stronger opioids [954-956]. Nonopioid analgesics, such as acetaminophen and NSAIDs, are commonly prescribed for mild pain (numerical pain score: 1–3). Weak opioids, such as codeine, hydrocodone, and tramadol, are used for moderate pain (numerical pain score: 4–6). Strong opioids, such as morphine, oxycodone, hydromorphone, fentanyl, and their analogs, are used for severe pain (numerical pain score: 7–10). Patients with severe pain should not start from the bottom of the analgesic ladder; they may immediately start with strong opioids and then step down the ladder if the cause of pain is deemed resolved. By using these three steps of pain management, approximately 80–90% of pain can be managed with drugs.
Mild pain
Although acetaminophen can cause fulminant hepatic failure [957,958], amounts of less than 4 g per day are very unlikely to cause clinically significant hepatotoxicity [959]. However, when other analgesics are added as a fixed dose combination, the dose of acetaminophen should be limited to ≤325 mg per dosage unit (tablet, capsule) in order to reduce liver manage induced by acetaminophen [959]. Although acetaminophen-induced hepatic failure has been reported at doses ≤4 g in chronic alcohol users [960], a number of studies have reported no noticeable hepatotoxicity for a daily dose of 4 g [961,962], while one study reported a small but significant increase in ALT levels [963]. A daily dose of 2–3 g of acetaminophen was reported to have no association with decompensation in patients with liver cirrhosis [964]. Although the half-life of acetaminophen is increased several folds in patients with liver cirrhosis compared to that in healthy individuals [965], studies have reported that ≤4 g of acetaminophen did not cause meaningful side effects in patients with decompensated cirrhosis or chronic liver disease [965,966]. However, a daily dose of 2–3 g is generally recommended for acetaminophen, as patients with liver cirrhosis are at risk of metabolic disorder and prolonged half-life of acetaminophen [967,968].
NSAIDs prescribed to patients with liver disease have a higher concentration of free compounds and are, thus, more likely to cause side effects and toxicity [969]. They are responsible for 10% of cases of drug-induced hepatitis [970] and are reported to cause hepatotoxicity [957,971]. Furthermore, NSAIDs can cause side effects such as nephrotoxicity [972], gastric ulcers or bleeding [973,974], and decompensation [964] in patients with liver cirrhosis; therefore, their use must be avoided as much as possible. In patients with bone metastasis, COX-2 inhibitors (rofecoxib, celecoxib, valdecoxib) are used to alleviate pain by inhibiting prostaglandin synthesis.
Moderate pain
Drug options are limited for the management of moderate pain before patients move on to take strong opioids, such as morphine. Major drugs used for moderate pain are tramadol and codeine. Tramadol is a nonopioid analgesic that acts on the central nervous system. It alleviates pain by binding with µ-opioid receptors. However, since tramadol is mainly metabolized in the liver, its bioavailability may increase two to three-fold in patients with liver cirrhosis; for these patients, no more than 50 mg of tramadol should be administered within 12 hours [975]. Additionally, tramadol should not be used in conjunction with adjuvant medications that interact with it to affect serotonin metabolism and lower the seizure threshold (e.g., selective serotonin reuptake inhibitor, serotonin-norepinephrine reuptake inhibitor, tricyclic antidepressants, and anticonvulsants).
Codeine is a weak opioid analgesic with 1/10 the potency of morphine and is metabolized via the P450 pathway. The use of codeine must be avoided in patients with liver cirrhosis since its metabolites may accumulate in the liver, causing side effects such as respiratory depression.
Severe pain
Strong opioids are the main method of treatment for severe pain. Among the known strong opioids, morphine is the most widely used type. Although the effectiveness of strong opioids is acknowledged across many countries, the access to strong opioids is limited. Strong opioids used in hospitals include morphine, oxycodone, hydromorphone, and fentanyl. They are usually administered orally, and intravenously when faster analgesic effects are necessary. Long-acting opioids are administered every 8–12 hours, and short-acting opioids are administered every 3–4 hours for breakthrough pain. Table 10 summarizes the doses and durations of action of oral and intravenous opioids, and considerations for patients with liver cirrhosis [976]. It is difficult to manage cancer pain by a single type of drug as the pain may develop from many causes. At least two different drugs should be used in combination after considering the intensity, frequency, and location of the pain.
Considerations for patients with liver cirrhosis
As liver is the major organ responsible for the metabolism of opioids, HCC patients with liver dysfunction may experience increased side effects from opioids, which can be a major cause of hepatic encephalopathy [966]. For this reason, it is necessary to select drugs and adjust their doses and administration intervals according to the liver-related metabolic characteristics of each opioid [968,977]. Morphine has an analgesic effect of its own, and over 90% is excreted via the kidney after being metabolized by conjugation in the liver. Its half-life is increased by about two-fold in patients with liver cirrhosis [978,979], and its bioavailability is four-fold in patients with HCC (68%) compared to that in healthy individuals (17%) [980]. A study reported that oxycodone is metabolized into several metabolites including oxymorphone, which has an analgesic effect, and that estimating the analgesic effect of oxycodone may be difficult since the blood concentrations of its metabolites vary. Moreover, it has been reported that oxycodone has a longer half-life, lower clearance, and greater potency for respiratory depression before LT compared to after transplantation [981]. Hydromorphone has an analgesic effect of its own, and its half-life is reported to be stable even in patients with liver dysfunction as it is metabolized and excreted by conjugation [982]. Fentanyl is metabolized by cytochromes, but it does not produce toxic metabolites. Its blood concentration remains unchanged in patients with liver cirrhosis and is not dependent on renal function [968,977,983]. Recently, the EASL recommended the use of paracetamol, morphine, and hydromorphone for pain control, while NSAIDs, tramadol, codeine, and oxycodone were suggested to be avoided in patients with end-stage liver disease [984].
In addition to medications, there are procedures available for pain management. Radiation therapy is widely performed for pain resulting from bone or lymph node metastasis and is highly effective. It is recommended for managing pain from metastatic HCC, although the level of evidence is low [127]. Depending on the location of metastasis or the affected tissue, RFA or transarterial embolization may also be used to manage pain effectively [985,986].
A multidisciplinary approach involving experts in palliative care is needed to effectively manage acute, recurrent, and chronic pain. As HCC is often accompanied by liver cirrhosis, drug doses must be adjusted after considering the therapeutic and side effects. Further research on pain management is needed to improve the quality of life and increase the survival of patients with HCC.
[Recommendations]
1. In HCC patients, pain control using drugs requires a careful approach with consideration of the underlying liver disease, and type of the drug, dose, and interval of administration should be determined according to liver function (C1).
2. In patients with HCC accompanied by chronic liver disease, a reduced dose of acetaminophen should be considered (C1), and NSAIDs should be used with caution (B1).
3. In patients with HCC accompanied by chronic liver disease, the selection of opioid analgesics, and adjustments in the dosage and interval of administration should be carefully considered based on drug metabolism and liver function (C1).
ASSESSMENT OF TUMOR RESPONSE AND POST-TREATMENT FOLLOW-UP
Tumor response
The primary purpose of research on HCC treatment is to verify the superiority of a treatment based on the OS. However, tumor response and TTP have also been used as alternative measures of assessing the therapeutic effect. In the field of oncology, tumor response has been traditionally assessed using the criteria by the WHO in 1979 (Table 11) [987]. However, this criterion poses a few problems; discrepancies in the measurement of changes in tumor size between researchers especially the short-axis diameter of the tumor, the number of tumors, and the different definitions of tumor progression, resulted in a lack of uniformity. For instance, whereas some researchers defined tumor progression based on change in the size of a single tumor, others defined it as the sum of the changes in all tumors. Additionally, the criteria do not account for the recent advances in imaging technologies, such as CT and MRI, which have enabled three-dimensional examination of changes in tumor size. To overcome these limitations, the RECIST and RECIST v1.1 were proposed in 2000 and 2009, respectively, which recommend assessing the overall response based on the treatment responses of both target and non-target lesions [988,989]. However, these criteria were designed to assess the outcome of cytotoxic chemotherapy and, thus, had limitations in assessing responses to treatments that do not affect the tumor size. Additionally, the RECIST criteria had some ambiguities regarding the assessment of treatment responses in cases where the best outcome was SD. Especially for molecular targeted therapy and TACE, which do not affect the tumor size, the RECIST is unsuitable to assess the treatment response [990]. Several studies have found that the RECIST does not appropriately account for tumor necrosis resulting from an intervention or a novel molecular targeted drug [790,991]. Theoretically, a viable tumor should be assessed by CT or MRI, and tumor viability should be defined according to the uptake of contrast agent in the arterial phase of dynamic imaging studies. Since the extent of tumor necrosis that occurs after local treatment of HCC is not proportional to a decrease in the diameter of the lesion, the EASL proposed a new definition of treatment response for HCC that considers the extent of tumor necrosis [992], and it was followed by the release of mRECIST criteria [990,993]. These proposals were based on the consensus that the diameter of a remnant tumor at the target site should be used to assess the treatment response. The assessment criteria for vascular invasion, lymph nodes, ascites, and pleural effusions were additionally revised in the mRECIST with a summary of the changes from the previous versions. However, since the mRECIST may be affected by the quality of CT and MRI used to locate tumors and the subjective judgment of the physician interpreting the imaging results, phase 3 clinical trials assessing the treatment response to molecular targeted therapy or immunotherapy tend to use the RECIST rather than the mRECIST.
When assessing treatment responses to recently introduced immunotherapy, pseudo-progression should be considered, which refers to a temporary increase in tumor size before showing a response to immunotherapy. A tumor undergoing pseudo-progression may be misdiagnosed as PD by the RECIST, resulting in a patient not being able to continue with the appropriate treatment. Pseudo-progression is a phenomenon in which tumor size temporarily increases due to inflammatory reactions such as inflammatory cell infiltration, swelling, and necrosis. It is also a phenomenon in which a delayed decrease in tumor size is observed as a result of the delayed immune response [994]. Pseudo-progression was first observed in melanomas. Approximately 2.8–11% of patients were reported to experience pseudo-progression following immunotherapy [995]. The iRECIST for assessing the responses to immunotherapy has been recently revised. It differs from the RECIST in that it divides PDs into unconfirmed PDs (UPDs) and confirmed PDs (CPDs). A PD that is suspected for the first time is classified as a UPD, and cases in which a tumor shows a consistent increase in size in follow-up tests or cases in which new lesions persistently emerge are classified as CPDs. A recent study that retrospectively analyzed patients with HCC who underwent nivolumab treatment reported that, of the 22 patients classified as having UPDs in the initial response assessment, 21 (95.5%) were classified as having CPDs in the second response assessment, while UPD was maintained in only one patient; in other words, pseudo-progression was not observed in any case in this study [996]. If the rate of pseudo-progression turns out to be very low for HCC [997], it may be more advantageous and cost-effective to switch patients with HCC over to new drugs immediately when PD is observed after immunotherapy. However, a large-scale prospective study is necessary and the new response assessment criteria must be continuously verified and revised for the new immunotherapy drugs [998].
Assessing radiologic responses and disease progression is important for maintaining objectivity in the interpretation of clinical research results on HCC as new drugs are being developed. A recent meta-analysis reported a clear correlation between the mRECIST criteria and PFS and OS, and reported ORR as an independent predictor of survival [999-1002]. Although several retrospective studies have shown that the results of these tumor response assessment methods reflect the prognoses of patients with HCC, the efficacies of these criteria for patients with advanced HCC are yet to be assessed through prospective research. Since it is not yet clear as to which response assessment methods are superior, treatment decisions should be made based on appropriate methods according to the stage of HCC and the treatment modality. Serum tumor markers can assist in assessing treatment responses when it is difficult to measure the tumor size. When there are no increase in AST/ALT levels, without positive radiologic findings of recurrence, an elevated AFP could support diagnosing recurrence [256]. However, serum tumor markers alone should not be used to assess the treatment response [1003].
Follow-up interval for tumor response
After the RECIST v1.1 was published in 2009, follow-up assessment of treatment response in solid tumors were recommended every 6–8 weeks in clinical studies [989]. Most of the recent phase 3 clinical trials on target therapies followed the 6–8 week interval. However, some of the recent studies on immune checkpoint inhibitors or immunotherapy had CT or MRI examinations performed every 8–12 weeks to assess the treatment response [853,1004]. A possible theoretical explanation is that there are more delayed responses to immunotherapy compared to targeted molecular therapy, and albeit rare, pseudo-progression may be misinterpreted as disease progression [1005]. To prevent such errors, a second imaging test is suggested to be performed 4 weeks after a lesion is initially classified as an UPD to determine whether the lesion is a CPD [998,1000,1006].
[Recommendations]
1. Assessment of tumor response to treatment should be done using the RECIST v.1.1 according to the change in tumor size and the mRECIST according to the change in viable tumor by dynamic contrast-enhanced CT or MRI (B1).
Follow-up after CR
There are only few studies on the follow-up evaluation after CR to HCC treatment. Complete response to curative treatment such as hepatic resection, LT, and percutaneous local ablation should be monitored with dynamic contrast-enhanced CT or MRI, serum tumor markers, and biochemical tests. Appropriate follow-up intervals are to be determined based on the pretreatment risk factors and the treatment-specific risk of recurrence.
Recurrence usually develops within 2 years after potentially curative treatments. Since early detection of recurrence increases the possibility of reapplication of curative treatment, posttreatment monitoring should be performed frequently enough to detect recurrence as early as possible [1008]. However, as the risk of recurrence varies depending on the stage of HCC, underlying risk factors, and the patient’s remnant liver function, it is difficult to suggest a uniform recommendation. In general, it is recommended to perform a follow-up assessment with dynamic contrast-enhanced CT or MRI, or MRI using liver-specific contrast agents in conjunction with serum tumor markers every 2–6 months for the first 2 years and every 6 months thereafter if no recurrence develops for 2 years [105,114,1009]. It is also important to note that patients may experience simultaneous or sequential metastases to other organs even after a curative treatment if the initial stage was advanced, vascular invasion was present, or serum AFP level was high [1010]. The lungs, lymph nodes, bones, and adrenal glands are common sites of extrahepatic metastasis. Although restriction of radiation dose for follow-up CTs is not recommended, patients who are expected to have a long survival period should avoid unnecessary CT exams, and alternative tests should also be considered. In addition, the monitoring interval should be individualized on the basis of patient-specific risk factors according to the tumor biology and the underlying liver diseases [1011-1013].
[Recommendations]
1. HCC patients with a CR after treatment should be followed up with imaging studies (i.e., dynamic contrast-enhanced CT/MRI or MRI with liver-specific contrast agents) and serum tumor markers every 2 to 6 months in the first
2 years; after that, patients should be followed via regular checkups at individualized intervals (B1).
MANAGEMENT OF PATIENTS WITH HCC DURING COVID-19 PANDEMIC
The COVID-19 pandemic situation that began in early 2020, caused by infection with a type of SARS-CoV2 virus, currently continues, and it is unclear when it will end. Thus, we aimed to provide brief information on treating patients with HCC during the COVID-19 pandemic. Considering that most patients diagnosed with HCC have underlying liver diseases, the treatment of HCC during a pandemic should take into account both the recommendations for the treatment of underlying liver disease and the general principles for other solid malignancies.
Prognosis of COVID-19 in patients with chronic liver disease and HCC
In meta-analyses, chronic liver disease was reported to increase the severity (OR, 1.48–1.52) as well as the mortality (OR, 1.36–1.78) of COVID-19, although it did not affect the probability of hospitalizations due to COVID-19 [1014,1015]. Patients with HCC were also shown to have an increased mortality risk from COVID-19 [1016,1017]. Specifically, COVID-19-related deaths in advanced liver disease were strongly associated with decompensated cirrhosis [1017]. In short, both underlying chronic liver disease and HCC are risk factors that increase the severity and mortality of COVID-19 compared to the general population. This suggests that the treatment and surveillance of chronic liver disease and HCC are still crucial and should be maintained during the COVID-19 pandemic.
Prevention
COVID-19 vaccination
Although the effectiveness of the COVID-19 vaccine varies depending on the type of SARS-CoV2 mutation, clinical trials have reported that mRNA vaccines are effective in preventing infection in up to 94.1–95.0% of cases [1018,1019]. Real-world clinical data showed that more than 80% of the overall infection and 90% of the symptomatic infection have been prevented by vaccination [1020]. Anaphylaxis, one of the serious adverse effects of mRNA vaccine, occurred in 2.5–4.5 cases per million doses, which was similar to influenza vaccines (1.4 cases per million doses), pneumococcal vaccines (2.5 cases per million doses), and shingles vaccines (9.6 cases per million doses) [1021]. Meanwhile, the incidence of myocarditis or pericarditis after the second jab of mRNA vaccine was estimated to be 10.6 cases per million doses. However, despite these adverse events, the Advisory Committee on Immunization Practices of US CDC still recommends vaccination, as the benefits outweigh the risks [1021].
The NCCN recommends patients with solid malignancies, such as HCC, to receive the COVID-19 vaccination as soon as possible, unless they have contraindications to the vaccine’s component [1022]. It has been demonstrated that cytotoxic chemotherapy-induced granulocytopenia does not affect the effectiveness of vaccines. Theoretically, immunotherapy including immune checkpoint inhibitors, could increase the risk of immune-related adverse events, but early studies have shown that the immune-related adverse events were not significantly higher in patients undergoing immunotherapy [1023]. However, an interval of at least 2–3 days between surgery and vaccination is recommended in order to determine which of them is responsible for symptoms, such as fever; and in the case of surgery, such as splenectomy, which causes a loss of immune function, vaccination should be delayed for approximately 2 weeks [1024]. The CDC recommends the use of mRNA vaccines, such as Pfizer-BioNtech BNT162b2 and Moderna mRNA-1273 [1020].
Although there have been no comparative studies of COVID-19 vaccines in patients with chronic liver disease, a phase 2/3 study with the Pfizer BNT162b2 vaccine included approximately 20.5% of patients with underlying conditions, including liver disease, and it showed no difference in the effectiveness of vaccine between healthy subjects and patients with underlying diseases (95.3% vs. 94.7%) [1019]. In a phase 3 study of the mRNA-1273 vaccine involving 196 patients with liver disease (0.6%), 100 of whom received the vaccination and 96 of whom received a placebo, no patient was infected with COVID-19, making it impossible to compare the two groups [1024]. As described above, it is still unclear whether the effectiveness of the COVID-19 vaccine varies depending on the presence of underlying liver disease, but the frequency of adverse reactions is not expected to differ significantly [1025]. Meanwhile, there have been several reports of occurrence and activation of autoimmune hepatitis in South Korea and other countries following COVID-19 vaccination, and further research is warranted since the causal relationship has not been established [1025,1026]. Vaccination should be decided based on the history of adverse events after vaccination and the underlying liver disease of the patient.
In moderate to severe immunocompromised patients, including those who have received treatment for cancer, the FDA and NCCN recommend administering a booster shot using mRNA vaccine within 3 months of COVID-19 vaccination [1024].
Adherence to precautionary measures for infection prevention
As patients with chronic liver disease and HCC have a higher risk of COVID-19 infection due to compromised immunity, they should adhere to routine infection control precautionary measures, such as wearing a face mask that fits properly [1027] and washing their hands frequently, even after being vaccinated [19,1028].
[Recommendations]
1. Even during the COVID-19 pandemic, the management of chronic liver disease, the surveillance of at-risk patients, and the treatment of HCC should be continued (D1).
2. COVID-19 vaccination is recommended in patients with HCC, as the benefits of vaccination outweigh the risks (C1). Meanwhile, it is necessary to monitor the occurrence of adverse events after vaccination.
3. Patients with chronic liver disease and HCC should strictly adhere to the infection precautionary measures even after COVID-19 vaccination since they may have a low antibody titer (D1).
Acknowledgements
The authors would like to thank Dr. Sung Won Lee (Catholic Univ. of Korea, Internal Medicine) and Dr. Yuri Cho (NCC Korea, Internal Medicine) for proofreading and revising the English-version manuscript, and Suhyun Chae for improving the images of staging. All required funding was provided by the NCC Korea (grant number. 2112570-2).
Abbreviations
90Y
Yttrium-90
AASLD
American Association for the Study of Liver Diseases
ABCR
AFP
ABRAS score
utilizing ALBI score
AFP
alpha-fetoprotein
aHR
adjusted HR
AJCC
American Joint Committee on Cancer
ALPPS
Associated Liver Partition and Portal vein Ligation for Staged hepatectomy
ALT
alanine aminotransferase
anti-HBc
HBV core antibody
anti-HBs
HBV surface antibody
APHE
arterial phase hyperenhancement
ART
Assessment for Retreatment with TACE
AST
aspartate aminotransferase
BCLC
Barcelona Clinic Liver Cancer
CCA
cholangiocarcinoma
CDC
Centers for Disease Control and Prevention
CEA
carcinoembryonic antigen
CEUS
contrast-enhanced US
CI
confidence interval
CIK
cytokine induced killer
combined HCC-CCA
combined hepatocellular-cholangiocarcinoma
CPD
confirmed PD
CR
complete response
CT
computed tomography
cTACE
conventional TACE
CTCAE
Common Terminology Criteria of Adverse Event
CTLA-4
cytotoxic T lymphocyte-associated antigen-4
DAA
direct-acting antiviral
DCR
disease control rate
DDLT
deceased donor liver transplantation
DEB
drug-eluting bead
DFS
disease-free survival
DOR
duration of response
EASL
European Association for the Study of the Liver
EBRT
external beam radiation therapy
ECOG
Eastern Cooperative Oncology Group
EORTC
European Organization for Research and Treatment of Cancer
FDA
Food and Drug Administration
FDG
fluorodeoxyglucose
FGFR
fibroblast growth factor receptor
FOLFOX
fluorouracil
Gd-EOB-DTPA
gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid
GRADE
Grading of Recommendations
HAIC
hepatic artery infusion chemotherapy
HBsAg
HBV surface antigen
HBV
hepatitis B virus
HCC
hepatocellular carcinoma
HCV
hepatitis C virus
HFSR
hand-foot skin reaction
HIMALAYA
FULL NAME
HKLC
Hong Kong Liver Cancer
HR
hazard ratio
ICG-R15
indocyanine green 15-minute retention rate
ICRP
International Commission on Radiological Protection
Ig
immunoglobulin
INR
international normalized ratio
ITT
intention-to-treat
KASL
Korean Association for the Study of Liver
KCCR
Korean Central Cancer Registry
KLCA
Korean Liver Cancer Association
KLCSG
Korean Liver Cancer Study Group
KONOS
Korean Network for Organ Sharing
KPGRC
Korea Practice Guideline Revision Committee
LDLT
living donor liver transplantation
LI-RADS
Liver Imaging Reporting and Data System
LLR
laparoscopic liver resection
LSM
liver stiffness measurement
LT
liver transplantation
LTP
local tumor progression
MELD
model for end-stage liver disease
mRECIST
modified Response Evaluation Criteria in Solid Tumors
MRI
magnetic resonance imaging
mTORi
mammalian target of rapamycin inhibitors
mUICC
modified UICC
NCC
National Cancer Center
NCCN
National Comprehensive Cancer Network
NSAID
nonsteroidal anti-inflammatory drug
OLR
open liver resection
OPTN
Organ Procurement and TransplantationNetwork
OR
odds ratio
ORR
objective response rate
OS
overall survival
PBT
proton beam radiotherapy
PCR
polymerase chain reaction
PES
postembolization syndrome
PD-1
programmed cell death protein-1
PD-L1
programmed cell death-ligand 1
PD
progressive disease
PDGFR
platelet-derived growth factor receptor
PEI
percutaneous ethanol injection
PET
positron emission tomography
PFS
progression-free survival
PIVKA-II
prothrombin induced by vitamin K absence II
PR
partial response
PVI
portal vein invasion
QALY
quality-adjusted life-year
RCT
randomized controlled trial
REILD
radioembolization-induced liver disease
RFA
radiofrequency ablation
RFS
recurrence-free survival
RR
relative risk
SAE
serious adverse event
SBRT
stereotactic body radiotherapy
SD
stable disease
SRTR
Scientific Registry of Transplant Recipients
SVR
sustained virologic response
TACE
transarterial chemoembolization
TAF
tenofovir alafenamide
TARE
transarterial radioembolization
TDF
tenofovir disoproxil fumarate
TNM
tumor-node-metastasis
TSH
thyroid stimulating hormone
TTP
time to progression
UCSF
University of California San Francisco
UICC
Union for International Cancer Control
UPD
unconfirmed PD
US
ultrasonography
VEGFR-2
vascular endothelial growth factor receptor-2
VETC
vessel encapsulating tumor cluster
WHO
World Health Organization
References
Appendices
Appendix 1.
2022 KLCA-NCC Korea Practice Guideline Revision committee (KPGRC)
cmh-2022-0294-app1.pdfAppendix 4.
Delphi round agreement on the recommendations of systemic therapy
cmh-2022-0294-app4.pdfAppendix 5.
Revision timeline of 2022 KLCA-NCC Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
cmh-2022-0294-app5.pdf