Systemic therapy in advanced hepatocellular carcinoma
Article information
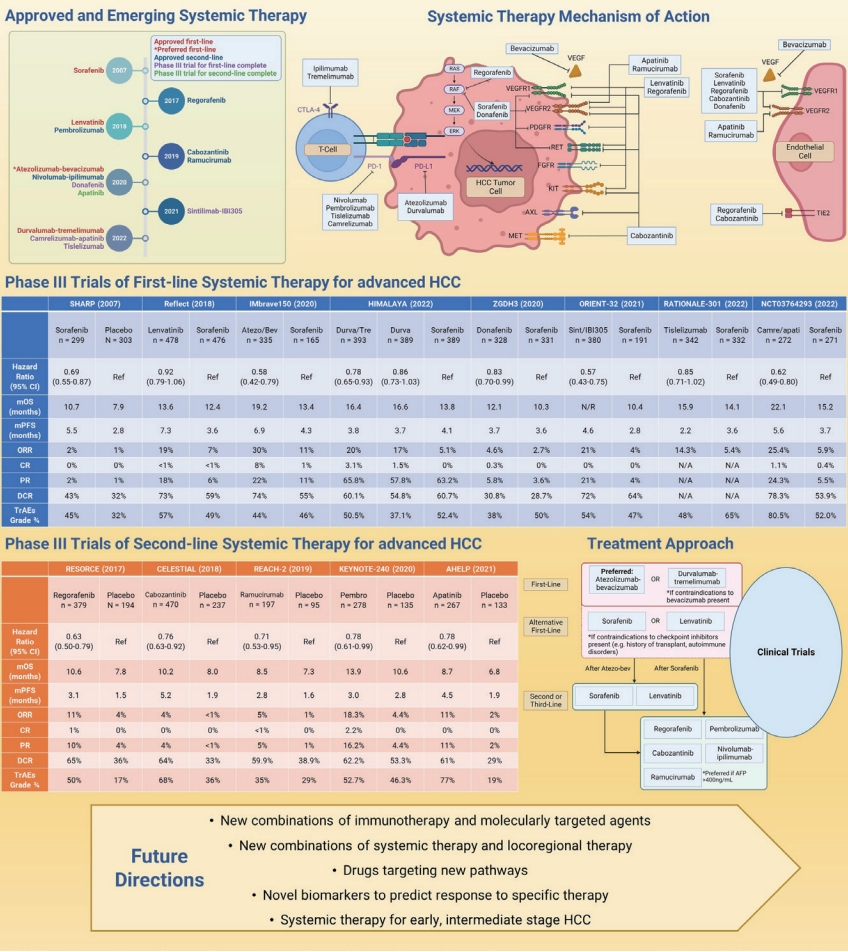
While advanced hepatocellular carcinoma (HCC) is an incurable disease, decades of research and clinical trials have led to substantial progress in treatment for advanced HCC [1]. In the 20th century, patients with advanced HCC were treated with conventional chemotherapy which offered little to no benefit with significant adverse effects [2]. The first breakthrough came with the molecularly targeted agents in the family of oral multi-tyrosine kinase inhibitors. In 2007, the multi-target kinase inhibitor sorafenib became the first-line systemic therapy for advanced HCC [3]. Since 2017, multiple positive phase III clinical trials have led to the approval of several additional molecularly targeted agents—lenvatinib [4] as a first-line, and regorafenib [5], cabozantinib [6], and ramucirumab [7] as second-line options. Additional multikinase inhibitors such as donafenib [8] and apatinib [9] have shown promising results in phase III trials conducted in China.
A dramatic therapeutic paradigm shift was driven by the advent of immune checkpoint inhibitors targeting programmed cell death protein-1 (PD-1), programmed death-ligand 1 (PD-L1), and cytotoxic T lymphocyte-associated protein 4 (CTLA-4). The first studied immunotherapy agents in HCC were the anti-PD-1 antibodies, nivolumab and pembrolizumab, which demonstrated clinical benefit and pembrolizumab has received accelerated approval as second-line agents following sorafenib [10,11]. More recently, tislelizumab (anti-PD-1 monoclonal antibody) demonstrated non-inferior overall survival (OS) compared to sorafenib (median OS: 15.9 months vs. 14.1 months; stratified hazard ratio [HR] 0.85 [95.003% CI 0.712–1.019]) in first-line setting phase 3 trial [12].
In 2020, the results of the landmark IMbrave 150 study led to the largest change in the treatment landscape of advanced HCC [13]. In this global phase III trial of patients with untreated unresectable HCC, the combination of atezolizumab (anti-PD-L1 antibody) and bevacizumab (anti-vascular endothelial growth factor antibody) was significantly superior to sorafenib with an improved median overall survival (19.2 months vs. 13.4 months, HR 0.58, 95% CI 0.42–0.79) and comparable rates of grade 3 or 4 adverse events (43% vs. 46%) [13,14]. This has quickly led to the adoption of atezolizumab-bevacizumab as the standard first-line systemic therapy [15-17].
Immunotherapy doublets have shown promising results [2]. The addition of an anti-CTLA-4 antibody to an anti-PD-1 or PD-L1 antibody significantly enhances the antitumor response by increasing the intratumoral concentration of T lymphocytes [18]. The combination of nivolumab and CTLA-4 inhibitor ipilimumab was approved as second-line therapy based on the CheckMate 040 study that showed manageable safety, promising response rate, and durable responses [19]. Recently, the phase III HIMALAYA trial showed positive results for durvalumab (anti-PD-L1 antibody) as a monotherapy and in combination with tremelimumab (anti-CTLA-4 antibody) for first-line treatment of advanced HCC [20]. In this study, durvalumab monotherapy was non-inferior to sorafenib, and moreover the durvalumab-tremelimumab combination was superior to sorafenib (overall survival: 16.4 vs. 13.8 months) [20]. Based on the results of the HIMALAYA trial, durvalumab-tremelimumab combination recently obtained US Food and Drug Administration (FDA) approval as a firstline treatment for advanced HCC. Therefore, the durvalumabtremelimumab combination offers another promising firstline treatment especially among those who cannot receive bevacizumab due to its anti-angiogenic effects.
Combinations of immunotherapy with molecularly targeted agents have mixed results. In the phase III COSMIC-312 trial, combination of atezolizumab with cabozantinib significantly improved progression-free survival compared to sorafenib (HR 0.63, 95% CI 0.44–0.91), while it did not reach statistical significance for overall survival (HR 0.90, 95% CI 0.69–1.18) [21]. Similarly, treatment with pembrolizumab and lenvatinib appeared to result in some improvement in overall survival and progression-free survival compared with lenvatinib monotherapy, but it did not meet statistical significance [22]. In the phase III ORIENT-32 trial, the combination of sintilimab (anti-PD-1 antibody) and IBI305 (bevacizumab biosimilar) showed significantly improved overall survival and progression-free survival compared to sorafenib in an exclusively Chinese patient cohort with high proportion of hepatitis B infection [23]. In another phase III trial reported in 2022 (NCT03764293), the combination of camrelizumab (anti-PD-1 antibody) and apatinib was again superior to sorafenib (HR 0.62, 95% CI 0.49–0.80) and provided a median overall survival of 22.1 months, the longest overall survival observed to date in phase III trials of advanced HCC [24].
More recently, synergistic treatment efficacy of the combined locoregional treatment and immunotherapy have been reported and several phase 2 and 3 clinical trials are ongoing to determine the efficacy and safety of combined immunotherapy and locoregional treatment [25,26]. A phase III study comparing sorafenib vs. stereotactic body radiation therapy (SBRT) followed by sorafenib showed that compared to sorafenib alone, SBRT prior to sorafenib improved overall survival (HR 0.72, 95% CI 0.52–0.99), progression-free survival (HR 0.55, 95% CI 0.40–0.75), and time to progression (HR 0.69, 95% CI 0.48–0.99) with improved quality of life [27].
We are in an exciting era where the landscape of systemic therapy for advanced HCC is rapidly evolving. Additional firstand second-line regimens are expected to be available as we await the readouts of ongoing phase III trials investigating different combinations of immunotherapy, molecularly targeted agents with, and without concurrent locoregional treatment. As responses to systemic therapy can be highly heterogeneous, there is an unmet need for biomarkers that would predict treatment response and enable an individualized approach to therapy.
Notes
Authors’ contributions
Ju Dong Yang devised the project and the main conceptual ideas for the snapshot; Joseph C. Ahn conducted the literature search and identified relevant studies to be included in the review; Ahn JC drafted the manuscript and the figure; Ju Dong Yang and Nguyen H. Tran revised the manuscript critically for important intellectual content; and all authors approved the final version to be published.
Conflicts of Interest
Dr. Yang provides a consulting service for Exact Sciences and Gilead. Dr. Yang’s research is funded by National Institute of Health 1K08CA259534-01A1. Dr. Tran’s research is funded by National Institute of Health 1K23MD017217-01A1.
Abbreviations
HCC
hepatocellular carcinoma
PD-1
programmed cell death protein-1
PD-L1
programmed death-ligand 1
CTLA-4
cytotoxic T lymphocyte-associated protein 4
HR
hazard ratio
OS
overall survival
SBRT
stereotactic body radiation therapy