Prediction of fibrosis progression in chronic viral hepatitis
Article information
Abstract
Prediction of liver fibrosis progression has a key role in the management of chronic viral hepatitis, as it will be translated into the future risk of cirrhosis and its various complications including hepatocellular carcinoma. Both hepatitis B and C viruses mainly lead to fibrogenesis induced by chronic inflammation and a continuous wound healing response. At the same time direct and indirect profibrogenic responses are also elicited by the viral infection. There are a handful of well-established risk factors for fibrosis progression including older age, male gender, alcohol use, high viral load and co-infection with other viruses. Metabolic syndrome is an evolving risk factor of fibrosis progression. The new notion of regression of advanced fibrosis or even cirrhosis is now strongly supported various clinical studies. Even liver biopsy retains its important role in the assessment of fibrosis progression, various non-invasive assessments have been adopted widely because of their non-invasiveness, which facilitates serial applications in large cohorts of subjects. Transient elastography is one of the most validated tools which has both diagnostic and prognostic role. As there is no single perfect test for liver fibrosis assessment, algorithms combining the most validated noninvasive methods should be considered as initial screening tools.
INTRODUCTION
Liver fibrosis represents a pervasive wound-healing response, driven primarily by the development of inflammation in response to parenchymal acute or chronic injury.1 Liver fibrosis may be represented by variable clinical manifestations, which are determined by the type and extent of liver damage, the underlying liver disease and the capacity of the whole body to respond. Cirrhosis, the end stage of liver fibrosis, is characterized by architectural disruption, aberrant hepatocyte regeneration, nodule formation and vascular changes.2 Cirrhosis substantially increases the risk of hepatocellular carcinoma, cirrhotic complications and death.3,4 Therefore it is important to accurately predict the rate of liver fibrosis progression in patients with chronic viral hepatitis, which has important clinical significance in terms of prognostic and treatment implications. On the other hand, with effective antiviral agents that potentially reverse liver fibrosis,5,6 methods of assessing fibrosis is essential to monitor disease progression, clinical outcomes, and response to treatment are warranted.
Risks of complications and liver fibrosis stage
There is no doubt that the risks of various complications increase dramatically if patients reached the stage of cirrhosis.7 In fact the risk starts to increase as early as F2 fibrosis. In a cohort of 188 Korean CHB patients followed up for nearly 10 years, the cumulative probability of developing cirrhosis for patients with Metavir stage F0 or F1 fibrosis at baseline was 0%, 11% and 11% at 5 years, 10 years and 15 years respectively. The probabilities were increased significantly with baseline fibrosis at stage F2 (12%, 33% and 47% at 5 years, 10 years and 15 years respectively) and stage F3 (22%, 47% and 65% at 5 years, 10 years and 15 years respectively).8 In another cohort of 2,215 patients with chronic viral hepatitis, the relative risk of developing cirrhosis and HCC in patients with F3 fibrosis was 6.3 (95% confidence interval [CI] 3.9-10.1) and 4.4 (95% CI, 2.4-7.8) compared with those with F1 and F2 fibrosis.9
Fibrogenic activities of HBV and HCV
The presence of HBV and HCV mainly lead to fibrogenesis induced by chronic inflammation and a continuous wound healing response. Additionally, direct and indirect profibrogenic responses are also elicited by the viral infection. HBV X protein induces paracrine activation of human hepatic stellate cells (HSCs).10 In vitro experiments indicate that HBV affects the proliferation and expression of collagen I in HSCs.11 Hepatitis B e antigen (HBeAg) was recently found to induce the activation and proliferation of HSCs, mainly mediated by transforming growth factor beta (TGF-β), and HBeAg protein purified from cell medium can directly activate HSCs.12
Several earlier studies described the pro-apoptotic, steatosis-inducing and cancerogenic effects of HCV core protein and nonstructural protein 5A (NS5A).13 Direct profibrogenic effects of HCV are demonstrated in HuH7 hepatoma cells which propagate the NS3-NS5 replicon, release profibrogenic factors, mainly active TGF-β1 that induces profibrogenic and suppresses fibrolytic genes and proteins in HSC and myofibroblasts.14 HCVE2 protein has been implicated in fibrogenesis, since it induces profibrogenic matrix metalloproteinase (MMP)-2 in HSC.15
Factors associated with fibrosis progression
Chronic hepatitis B
Chronic hepatitis B (CHB) patients may have variable disease course with outcomes ranging from inactive carrier state, active hepatitis, liver fibrosis to cirrhosis.16 The well-established risk factors for progression from mild to advanced liver fibrosis in CHB include older age, male gender, alcohol use, co-infection with hepatitis C virus, hepatitis D virus, or human immunodeficiency virus, elevated alanine aminotransferase (ALT) levels, and high hepatitis B virus (HBV) DNA level (Table 1).17 Ongoing HBV replication or presence of HBeAg may accelerate the progression of chronic hepatitis to advanced fibrosis cirrhosis.18 Delayed HBeAg seroconversion (over 40 years of age) and HBeAg seroreversion after spontaneous HBeAg seroconversion, indicating a prolonged period of viral replication and necroinflammation, were associated with increased risk of cirrhosis.19 Genotype C HBV was associated with more severe liver fibrosis than genotype B HBV, probably because of delayed HBeAg seroconversion and prolonged active disease.20
Two recent studies made use of serial liver stiffness measurements (LSM) with transient elastography to assess the change in liver fibrosis in large cohorts of asymptomatic CHB patients. Liver fibrosis progression was defined as an increase in LSM by 30% or more.21,22 The study of 361 patients with inactive HBeAg-negative CHB demonstrated that liver fibrosis progression is rare in if their serum HBV DNA <20,000 IU/ml and normal ALT.21 Nonetheless around 24.8% of patients with HBV DNA between 2,000IU/ml and 20,000 IU/ml developed treatment indications during follow-up.21 The study of 247 HBeAg-positive CHB patients revealed that 4.1% and 6.6% patients in immune-tolerant and immune-reactive phase had liver fibrosis progression, whereas and 12.2% and 67.2% of them received antiviral therapy respectively.22 These observations provided indirect evidence that antiviral therapy aborts liver fibrosis progression.
Studies conducted before the introduction of the highly active anti-retroviral therapy (HAART) have shown that human immunodeficiency virus (HIV)-related immune deficiency modifies the natural history of CHB with higher levels of HBV replication and a lower rate of spontaneous HBeAg seroconversion, leading to a more rapid liver fibrosis progression towards cirrhosis.23 Chronic HDV infection leads to more severe liver disease than chronic HBV mono-infection with an accelerated course of fibrosis progression, an increased risk of hepatocellular carcinoma and early decompensation in the setting of established cirrhosis.24 Recipients with graft occult HBV infection (O-HBV) and no O-HBV in the native liver who received their grafts from donors aged above 40 years.25
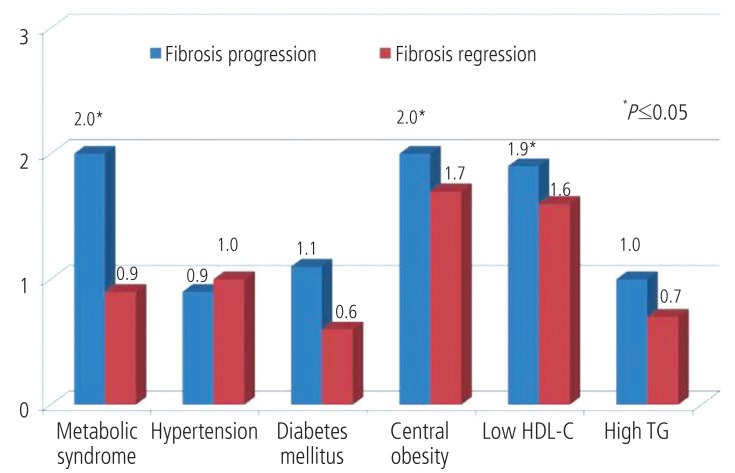
Recent data from Chinese and Korean cohorts established that metabolic syndrome is a risk factor of advanced liver fibrosis and cirrhosis independent of viral factors in CHB.26,27 In a recent prospective cohort study of 663 CHB patients, new-onset metabolic syndrome and some of its components (namely central obesity and low high-density lipoprotein cholesterol) were found associated with liver fibrosis progression (Fig.).28 Even the effect of such coincident metabolic syndrome was most apparent in the immune tolerant phase; its effect was independent of change in viral load and ALT level.28 This is supported by the observation from a survey in general population that CHB is associated with a lower prevalence of fatty liver, hypertriglyceridemia and metabolic syndrome.29
Chronic hepatitis C
Chronic hepatitis C (CHC) is associated with variable rates of fibrosis progression. Established cofactors for fibrosis progression include older age at infection, male gender, chronic alcohol consumption, obesity, insulin resistance and type 2 diabetes, and immunosuppression therapy.30 In spite of slow disease progression over the initial 20 years of infection, advancing age may accelerate fibrosis progression.31 Recent studies suggest an association between hepatitis C virus (HCV) genotype 3 and accelerated liver disease progression.32
After liver transplantation, fibrosis progression is highly accelerated in patients with recurrent hepatitis C with development of bridging fibrosis and cirrhosis in 20-54% at 5 years and 32-51% at 7 years.33 HIV co-infection is an important contributor to progression of chronic hepatitis C. HIV envelope protein gp120 blocks insulin signaling and via induction of oxidative stress increases profibrogenic tissue inhibitor of metalloproteinase-1 (TIMP-1) in HCV-replicon cells, and also directly induces procollagen synthesis in cultured hepatic stellate cells (HSC).34 The more rapid liver fibrosis progression to F4 was observed for men with alcoholic fatty liver disease, and the slower for women with non-alcoholic fatty liver disease (NAFLD).35
Antiviral therapy and fibrosis regression
Chronic hepatitis B
There is ample evidence to support the fact that effective antiviral therapy potentially reverses liver fibrosis in CHB patients.6,36 The first solid evidence came from a cohort of 57 patients who received at least 3 years of cumulative entecavir therapy, among whom 88% had ≥1-point improvement in the Ishak fibrosis score, including all 10 patients with advanced fibrosis or cirrhosis.36 This notion was further consolidated by a larger cohort of 348 patients who tenofovir disoproxil fumarate, in which 176 (51%) had regression of fibrosis at week 240.6 More impressively, of the 96 (28%) patients with cirrhosis (Ishak score 5 or 6) at baseline, 71 (74%) had regression of cirrhosis (≥1 unit decrease in the score). Data from the same trial revealed that steatosis at baseline correlated with decreased regression of cirrhosis at week 240; 73% of ≥grade 1 patients had regression of cirrhosis vs. 88% of grade 0 patients; nonetheless body mass index remained the only significant factor in multivariate analysis.37
Chronic hepatitis C
Data has been available since early this century to illustrate the fact that interferon therapy regress liver fibrosis in CHC patients with SVR.38 Similar findings have been reported in sustained responders to pegylated interferon.39,40 Regression of liver fibrosis, which occurred in 82% of patients, was sustained at 5 years after SVR; more impressively recovery of normal or nearly normal liver architecture is possible.5
It is a big challenge to use interferon-based antiviral therapy in post-transplantation recurrent HCV infection because of its side effects and concern on triggering rejection.41 Therefore its effects on fibrosis progression have been little investigated. Antiviral therapy is commonly started when fibrosis reaches F2 or above; stabilization or even improvement of fibrosis may be seen in patients with or without sustained virologic response (SVR).42,43 The data from a randomized controlled illustrated that antiviral therapy slows fibrosis progression provided it is started early (F0-2).44
Assessments of fibrosis progression
In the treatment guidelines issued by different authorities of liver diseases, severity of liver fibrosis, together with ALT and HBV DNA level, has a central and important role on the decision-making process of CHB.45,46,47 Improvement and even regression of liver fibrosis and cirrhosis following successful antiviral treatment are questioning the need for a follow-up liver biopsy.5 Longitudinal measurements using noninvasive methods could allow an effective monitoring of the dynamic changes of liver fibrosis, as shown in the liver transplant setting.48
Liver biopsy
Liver biopsy has been the gold standard of liver fibrosis assessment in the last few decades. However it is often challenged for its diagnostic accuracy limited by the sampling variability as the average size of biopsy is 15 mm in length, which only represents 1/50,000 the size of the entire liver.49 There is significant variability in the histologic assessment of two readings of the same biopsy by the same pathologist, and between two pathologists, even among those who are highly specialized.50 Furthermore, all of histologic scoring systems are discontinuous and hence semi-quantitative.51 Pain is reported by one-third of the patients undergone liver biopsy, whereas a severe complication (which is life-threatening or prolongs hospitalization) occurs in 3 out of 1000 cases and death is reported in 3 out of 10,000 cases.52 Liver biopsy may also lead to selection bias towards more active disease such that the incidence of advanced fibrosis would be overestimated.53 All these problems make it impractical to perform serial biopsies to assess disease progression in routine clinical practice.54
Transient elastography
Reliable non-invasive methods for the assessment of liver fibrosis are increasingly being incorporated in the management of patients with chronic viral hepatitis, helping predict prognosis, guide treatment decisions, and stratify patients for antiviral therapy as well as emerging antifibrotic therapies.33
Transient elastography by Fibroscan (Echosens, Paris, France) has been developed as an accurate, reproducible and non-invasive test for the assessment of advanced liver fibrosis.7 It has been the most widely-validated tools in essentially all chronic liver diseases including CHB and CHC.55 The beauty of this tool is its non-invasiveness, which makes it possible to perform repeated liver fibrosis assessments on a large number of asymptomatic patients in a cross-sectional and serial fashion.21,22,56,57
The remaining controversies include the optimal cutoff values to diagnose advanced fibrosis and cirrhosis, which differ according to particular etiologies. The suggested diagnostic performance and cutoff values for histologic cirrhosis (F4) in CHB and CHC based on published studies are summarized in Table 2. Another issue is the definition of liver fibrosis progression based on LSM. One of the initial studies defined it an increase of LSM above 30%,58 mainly because an interquartile range (IQR) within 30% of LSM would reflect reliable results.59 Some investigators studied dynamic changes of LSM according to different strata of LSM.60,61
A 3rd generation transient elastography Fibrotouch (Wuxi Hisky Medical Technology Co Ltd, Beijing, China) has been available in clinical use since 2013. The potential advantage of Fibrotouch is it may overcome obesity, as the depth of measurement will be adjusted according the thickness subcutaneous fat in obese patients with the dynamic probe.62
Other imaging-based assessments
Magnetic resonance elastography (MRE) is probably one of the best non-invasive assessments of liver fibrosis in terms of diagnostic accuracy for different stages of liver fibrosis. MRE can discriminate between patients with moderate or more fibrosis (≥F2).63 The technical success rate of magnetic resonance elastography was high (94%), and the AUROCs of MRE were also impressive (0.994 for ≥F2; 0.985 for ≥F3; 0.998 for ≥F4).64 Even so, the major limitation of MRE is its availability, as MR machine may not be readily available in some centers. The long examination time also poses implication on the cost of the examination.65
Acoustic radiation force impulse imaging (ARFI) involves mechanical excitation of tissue using short duration acoustic pulses that propagate shear waves and generate localized, µ-scale displacements in tissue.66 The major constraints of ARFI is its narrow range of values (0.5-4.4 meters/sec), in contrast to LSM by transient elastography (1.0-75.0 kPa). This may limit the definitions of cutoff values to define various stage of fibrosis.67 Shear wave elastography (SWE, SuperSonic Imagine, Aix-en-Provence, France) is an absolute quantification of tissue stiffness in terms of pressure unit of kiloPascal (kPa) rather than producing semi-quantitative estimate corresponding to relative tissue strain.68 SWE was found more accurate than Fibroscan in liver fibrosis ≥F2.69 All these imaging techniques were mostly assessed in a cross-sectional fashion such that accuracy on applying them in longitudinal fashion remains uncertain.
Serum markers
Serum markers for liver fibrosis are classified as direct (or class I) which represent extracellular matrix components (reflecting the pathophysiology of liver fibrogenesis); and indirect (or class II) which use routine laboratory data (reflecting the consequences of the liver damage). Direct and indirect markers may be used alone or, more commonly, in combination to produce composite scores.70 Serum markers generally have modest accuracy to diagnose advanced liver fibrosis.71 A non-invasive test independent of the serum ALT or AST levels may be a good supplementary test for LSM. Among various serum test formulae, Forns index72 and Hui index73 are composed of clinical parameters other than ALT or AST levels. We demonstrated that combined LSM-Forns or LSM-ELF algorithm improved the accuracy to predict advanced liver fibrosis in CHB patients.74,75
The Fibrotest (proprietary formula; Biopredictive, Paris, France) is the most widely validated indirect serum marker panel, most extensively studied in CHC.76 It is computed using five parameters, namely total bilirubin, haptoglobin, gamma-glutamyl-transpeptidase, a2-macroglobulin and apolipoprotein-A.77 In a systematic review including 9 studies (1,679 patients), an excellent discrimination was found for identifying cirrhosis, but a lesser ability to identify significant (≥F2) fibrosis.78 The combination of LSM and Fibrotest was found to have the best diagnostic performance compared to either test alone in patients with CHC.79
CONCLUSIONS AND FUTURE PERSPECTIVES
Serial monitoring of liver fibrosis with non-invasive tools becomes indispensable and is replacing serial liver biopsy examinations in clinical studies and practice. The issue left is that the validation of novel noninvasive tools is often based on liver biopsy, the imperfect gold standard of liver fibrosis assessment. Moreover, histological scores of liver fibrosis are ordinal categories with no quantitative relationship between them and therefore inappropriate to use as continuous variables.80 Noninvasive markers of liver fibrosis should be ideally validated against quantitative histological measures. In this setting, collagen proportionate area (CPA) defined as the proportion of the area of the biopsy occupied by collagen measured by computer-assisted morphometric analysis of digital images81 should be adopted to compare with noninvasive methods.82
As there is no single perfect test for liver fibrosis assessment, algorithms combining the most validated noninvasive methods, most likely one imaging-based and one serum-based marker, should be considered as initial screening tools. In cases of indeterminate or discordant results, liver biopsy can be performed to confirm the exact stage of fibrosis. Recently, the Asian Pacific Association for the Study of the Liver (APASL) consensus on liver fibrosis has recommended the use of a stepwise algorithm of using noninvasive markers, concluding that this approach may reduce the need for liver biopsy by 30%.83 Hence, integration of noninvasive assessments into clinical guidelines will become standard clinical practice shortly.
Notes
The authors have no conflicts to disclose.
Abbreviations
ALT
alanine aminotransferase
BMI
body mass index
CHB
chronic hepatitis B
CHC
chronic hepatitis C
CI
confidence intervals
HBeAg
hepatitis B e antigen
HBsAg
hepatitis B surface antigen
kPa
kilopascal
LSM
liver stiffness measurement
N.A.
not applicable
NAFLD
non-alcoholic fatty liver disease