INTRODUCTION
As the human life span has been extended with the development of medicine, chronic diseases rather than acute ones have been increasing. Because it is hard to cure chronic liver disease completely and it should be controlled well for life, patients and their family members bear various burdens. Liver disease, one of the most representative chronic diseases, has showed a high prevalence rate in the East including South Korea and it includes chronic hepatitis, hepatic cirrhosis and hepatocellular carcinoma (HCC).
Liver disease ranked the eighth among causes of death in South Korea in 2009, and 6,868 died of liver disease for the one year.
1 It recorded adds the cause of fifth in males and did third in persons in their 40s. Moreover, the mortality rate of HCC showed the second highest level by following lung cancer and it did the highest in persons in their 40s and 50s.
1 In particular, a study estimating socioeconomic costs of major cause of death in South Korea revealed that the loss of productivity caused by premature death due to chronic liver disease ranked second next to that of cancer.
2 The high mortality of liver disease in economically active persons in their 40s and 50s means that the importance of liver disease management should be recognized by considering that chronic liver disease influences not only individuals or families but also the productivity of a society.
3
The cost of illness is one of the most initial economic evaluation methods in the healthcare and it aims to measure the economic burden of illness in a society in terms of the consumption of healthcare resources and the loss of productivity.
4 In addition, studies on the cost of illness suggest the negative influence of illness and injury by using a monetary unit which is a universal language of decision-makers and policy-makers. However, their results can provoke a considerable difference by countries, a base year for estimation, types of disease, cost items, formulas for estimation and data for analysis among researchers and can have problem relating to validity or reliability.
5,
6 Nonetheless, studies on the cost of illness have been utilized as important indexes to prioritize the economic burdens of specific diseases, to determine the priority of research and development in National Institutes of Health, Institute of Medicine, the national assembly and others.
6
Most previous studies on the cost of illness have dealt with major health risks like specific diseases
2,
7,
8 or smoking,
9-
12 alcohol-drinking
13-
15 and obesity
16-
18 and their relevant diseases. But, even though liver disease exerts not a few negative effect in South Korea with recording a high mortality rate especially in economically active age groups as one of major death causes, there has been nearly no study analyzing the socioeconomic burden of liver disease precisely in the country. Therefore, this study aims to estimate the socioeconomic costs of major liver diseases (viral infection, liver cirrhosis and others and HCC) for the last five years (2004-2008) to provide basic data for the public awareness of the importance of prevention and management of liver disease.
DISCUSSION
Liver disease is one of major death causes in South Korea and the number of deaths caused by it tends to be high in economically active age groups as a representative disease provoking a significant loss of productivity due to premature death. In 2001, liver disease ranked fifth among death causes in South Korea but its loss of productivity due to premature death was found to be the highest except cancer which is the number one death cause. Although liver disease leads to a considerable socioeconomic loss in the country like this, basic studies to establish liver disease-related health insurance policies are insufficient. Therefore, this study was conducted to provide basic data for policy making for the prevention and the management of liver disease in the future by estimating the socioeconomic costs of major liver diseases for the last five years from a societal perspective.
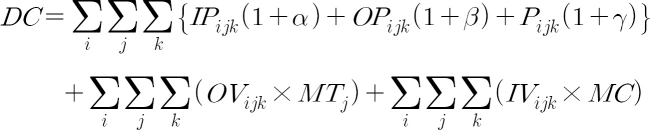
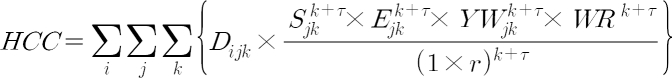
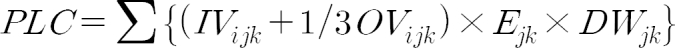
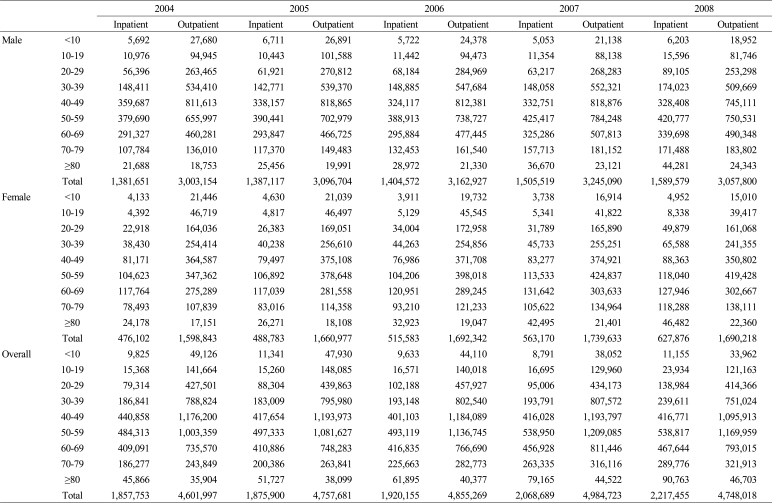
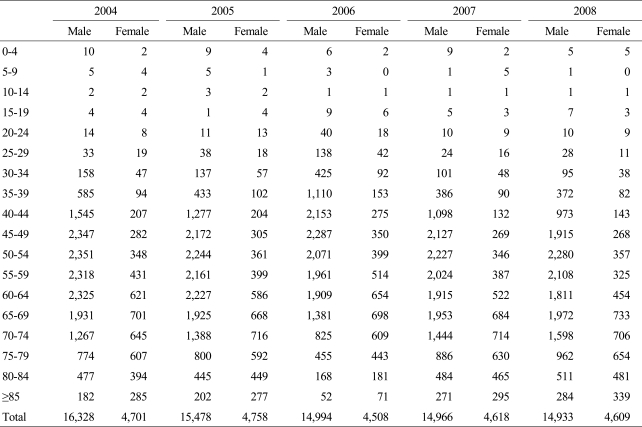
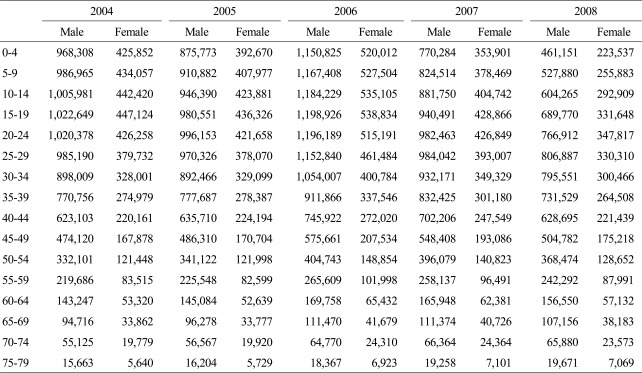
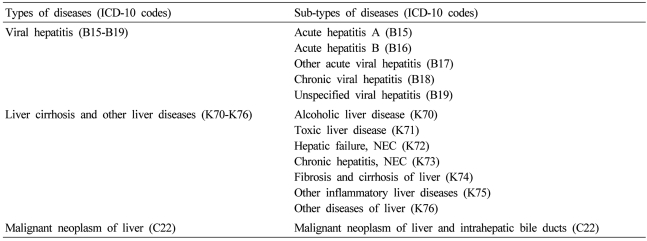
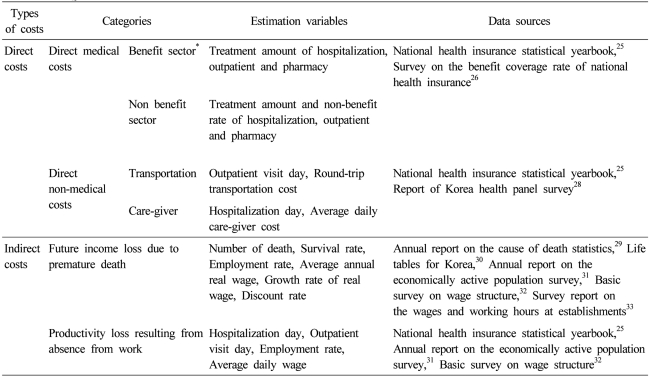
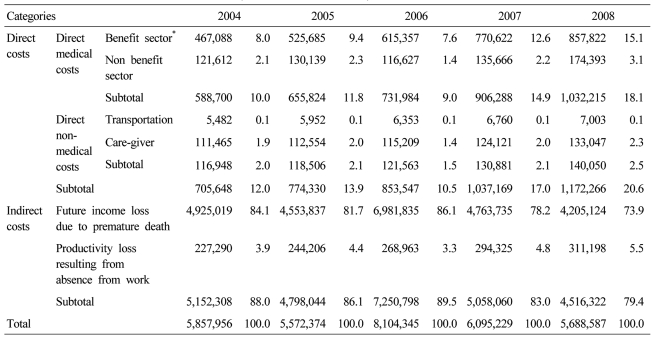
Liver diseases analyzed in this study were viral hepatitis (B15-B19), liver cirrhosis and other liver disease (K70-K76) and HCC (C22) and the costs of them were estimated by dividing them largely into direct and indirect costs. The directs costs contained the treatment amount covered and not covered by health insurance for inpatients and outpatients at medical institutions and at pharmacies, the traffic costs to visit medical institutions and the personnel expenses of caregivers or the opportunity costs of guardians for inpatients. The indirect costs did the lost earnings caused by liver disease-related premature death and the loss of productivity following absences from work to visit medical institutions.
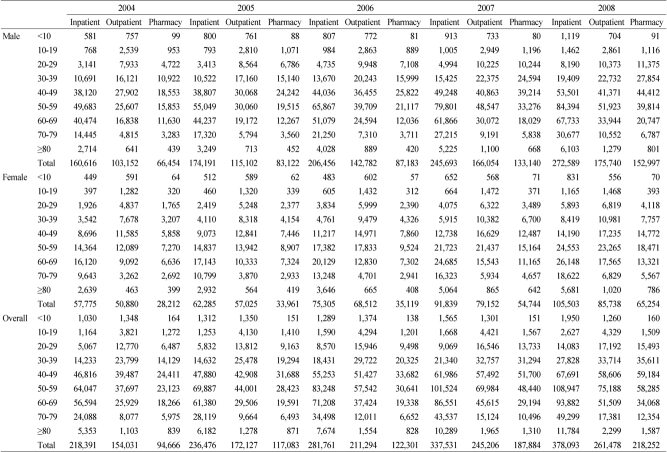
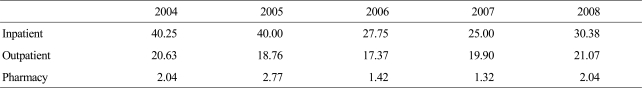
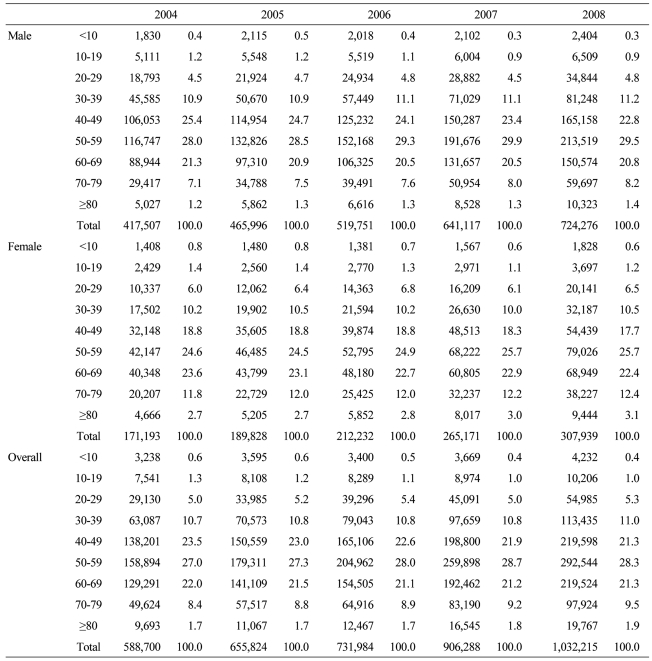
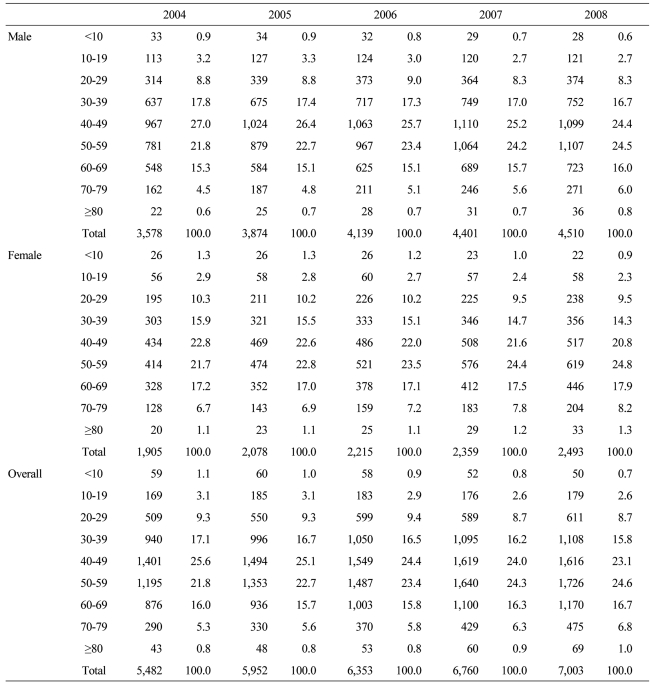
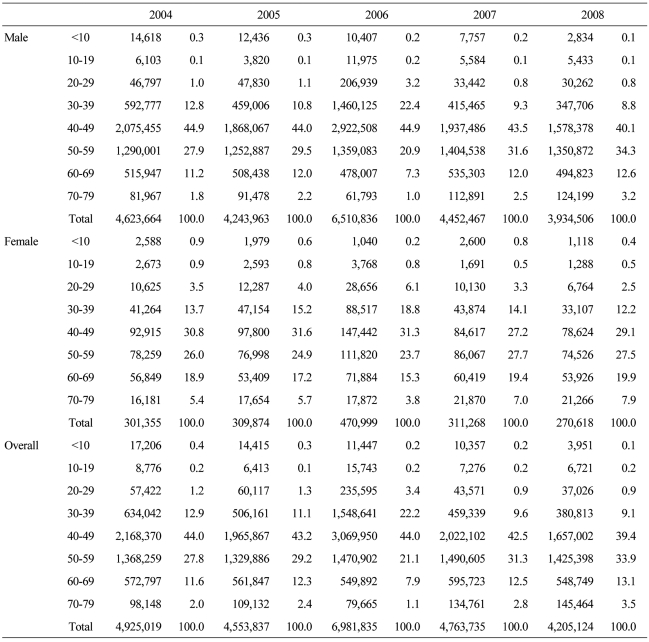
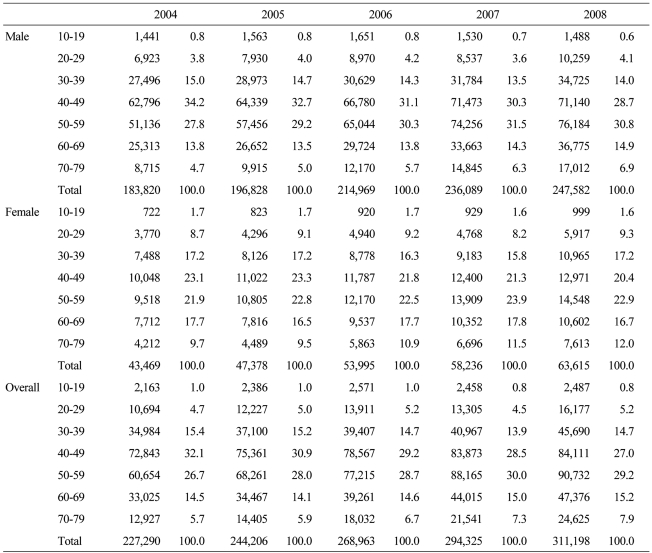
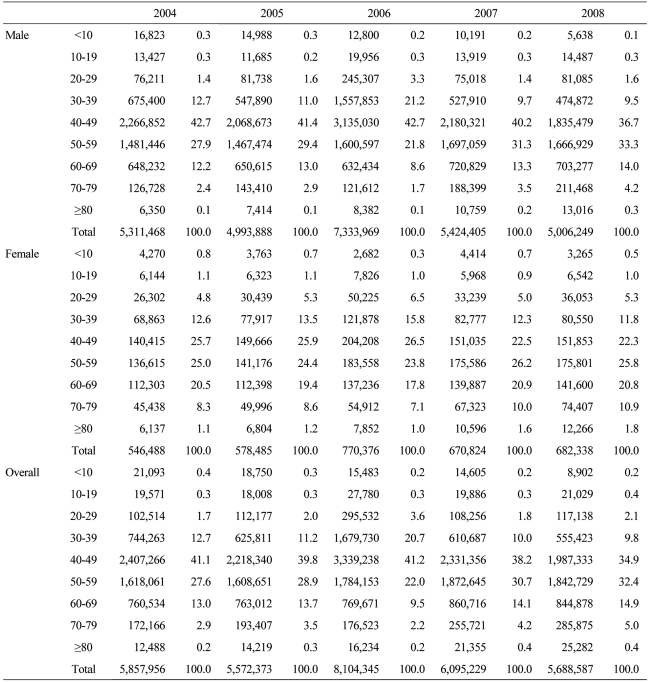
According to the results, the socioeconomic costs of liver disease were estimated to be KRW 5,858 billion, KRW 5,572.4 billion, KRW 8,104.3 billion, KRW 6,095.2 billion and KRW 5,688.6 billion from 2004 to 2008, respectively. By the cost items, the lost earnings caused by liver disease-related premature death accounted for the largest portion of the total costs or 73.9-86.1%, and the direct medical costs (9.0-18.1%), the loss of productivity following sick leave (3.3-5.5%) and the traffic costs and the costs of caregivers (1.5-2.5%) followed it in the order. Out of the total socioeconomic costs of liver disease, 88.0-90.7% were incurred in males, and the costs by age showed higher rate in the patients in their 40s (34.9-41.2%), 50s (22.0-32.4%) and 30s (9.8-20.7%) in the order.
A study of Jung and Ko
2 estimated the socioeconomic costs of the top five diseases for death causes in South Korea by classifying the costs into direct and indirect costs. In their study, the direct costs included medical expenditures, traffic costs and costs of guardians and the indirect costs did costs of lost workdays due to illness and lost earnings due to premature death. They reported that the costs of cancer (malignant neoplasm) or number one death cause, cerebrovascular disease, heart disease, diabetes and liver disease were KRW 7,735.8 billion, KRW 2,313.8 billion, KRW 2,141.7 billion, KRW 1,158.8 billion and KRW 2,620.1 billion, respectively. For liver disease, the lost earnings due to premature death accounted for 88.3% of the total costs and rates of the medical expenditures of inpatients and outpatients, the costs of lost workdays, the costs of caregivers and the traffic costs recorded 7.7%, 2.4%, 1.1% and 0.5%, respectively.
In the comparison of the results between their study and this one, the study of Jung and Ko
2 showed that the socioeconomic costs of liver disease were estimated to be KRW 2,620.1 billion in 2001 while this study found that the costs were done to be KRW 5,858 billion in 2004, so the difference in the costs was significant. That is considered to result from not only the difference in the year of estimation and the methodologies but also the exclusion of the costs at pharmacies, which accounted for a considerable portion in the total costs, in the study of Jung and Ko.
2 But, the finding that the rate of lost earnings due to premature death recorded the highest level among the socioeconomic costs of liver disease and the lost earnings by age showed the highest rates in economically active persons in their 30s, 40s and 50s, tended to be similar in both of the two studies and it led to a large influence on the loss of productivity in the society at large.
In addition, studies estimating the socioeconomic costs of disease have been reported continuously in Canada since 1986. A study calculating the socioeconomic costs by classifying total disease into 20 groups such as cardiovascular disease, musculoskeletal disease and cancer with the data in 1998 was published.
34 The study in Canada
34 largely divided the costs of diseases into direct and indirect costs, and the direct costs included treatment amount at medical institutions, drug expenditures and doctor bills and the indirect costs contained death costs and costs of prevalence of short- and long-term disorder. According to its results, although it did not examine liver disease specifically, the direct and indirect costs of the digestive disease including liver disease accounted for 4.2% (USD 3.54 billion) and 3.1% (USD 2.31) of the costs of total diseases and their sum recorded 7.3% (USD 5.85 billion). As the study in Canada found that the weight of direct costs incurred by visiting medical institutions directly to treat digestive disease were estimated to be larger than that of indirect costs such as death costs, the finding was different from that of Korean studies investigating only liver disease.
This study is meaningful as the latest study on estimation of the socioeconomic costs of liver disease for the longest period. Moreover, because it calculated the costs from a societal perspective, it included the extensive effect of liver disease on the society at large. In particular, all Koreans have been insured mandatorily and the country has established a single insurance claim system so that the total scale of healthcare utilization except uninsured items can be grasped when liver disease patients utilize medical institutions or pharmacies. As this study used these health insurance data to estimate direct medical costs, direct non-medical costs (traffic costs, costs of caregivers) and the loss of productivity following sick leave, the validity and the reliability of results of this study were expected to be enhanced. However, for direct medical costs, uninsured items not paid by the health insurance system needed to be included to calculate actual costs exactly but this study gained the uninsured medical costs by estimating them with the rate of uninsured out-of pocket payments
26 in South Korea published by National Health Insurance Corporation every year since 2004. But, the data had a limitation that they did not include those about packs of prepared herb medicine in the oriental medicine and health improving agents like vitamin supplements at pharmacies. Although this study utilized the best available data and methodology to enhance the reliability and the utilization of the results, it had some limitations as follows.
First, in the process of investigating the healthcare utilization with the health insurance data related to liver disease, the data were extracted with only principal diagnosis as a standard with excluding liver disease as additional diagnosis, so the directs costs and the loss of productivity following sick leave could be underestimated. Second, costs of driving cars to visit outpatient clinics due to liver disease were excluded from the mean traffic costs so that the average round-trip traffic costs per one visit to an outpatient clinic could be underestimated. Third, for costs of caregivers for inpatients with liver disease, the nursing of guardians or paid caregivers might be determined by the severity of disease and the costs of caregivers could be incurred at home as well as at medical institutions. However, because of no data about the rate of the care-giving at home and the correlation between the severity of disease and the utilization rate of care-giving service, this study limited cases to calculate the costs of caregivers to inpatients at medical institutions, so the costs of caregivers was estimated on the assumption that the inpatients needed full-time care-giving. Fourth, in the process of estimating the future income loss due to premature death caused by liver disease and the loss of productivity following sick leave, this study analyzed only employees with income except unemployed persons (job seekers) and economically inactive population (housewives, students and persons waiting to enter the army) among the working-age group aged over 15 years to calculate the scale of objective and valid income loss. So, the exclusion of unpaid productive activities of unemployed persons and economically inactive population could underestimate the loss of productivity following premature deaths and sick leave, but objective and valid data to investigate the rate of the population and the economic value of the unpaid activities were insufficient. Fifth, the loss of productivity following sick leave contained the decreased or lost income of employed liver disease patients due to hospitalization or visits to medical institutions. However, a simple rest at home or other places during sick leave by the severity of disease was excluded in this study because of no data about the population, so the loss of productivity following sick leave could be underestimated. Lastly, the health insurance data are collected based on claims submitted to National Health Insurance Corporation by healthcare providers to receive costs paid by the insurer among the total costs of patients. Therefore, validity issues related with diagnosis and the content of medical service in the health insurance data have been raised continuously and particularly up-coding of reporting wrong disease codes intentionally works as a factor hampering the reliability of studies using the data. However, despite these fundamental limitations of the health insurance data, this study is considered to have relatively less up-coding inducing factors by analyzing liver disease or one of comparatively severe diseases and some up-coding related errors within liver disease are thought not to influence the results of this study considerably because this study analyzed the total liver disease not a part of the disease.
In conclusion, the socioeconomic costs of liver disease, although they were slightly different by year, were as much as maximally KRW 8,104.3 billion in 2006. The lost earnings caused by liver disease-related premature deaths accounted for the largest portion or 73.9-86.1%. However, while the rate of lost earnings tended to reduce slightly from 2004 to 2008, the rate of direct medical costs paid by health insurance increased sharply. These findings meant that measures to improve the efficiency of the medical costs of liver disease are necessary.
Moreover, 88.0-90.7% out of the socioeconomic costs of liver disease were incurred in males, and the costs by age recorded the highest rate or 34.9-41.2% of the total costs in liver disease patients in their 40s and those in their 50s (22.0-32.4%) and 30s (9.8-20.7%) followed them in the order. That shows that liver disease provokes a significant loss in most economically active age groups, and if appropriate measures for the management of liver disease are not prepared, not only the loss of productivity in the society at large but also various potential loss are expected to be raised. Lastly, the results of this study are considered to be useful for promoting the public awareness of the urgency of the prevention and the management of liver disease and for prioritizing disease-related policies in various health projects.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




