Are there differences in risk factors, microbial aspects, and prognosis of cellulitis between compensated and decompensated hepatitis C virus-related cirrhosis?
Article information
Abstract
Background/Aims
Cellulitis is a common infection in patients with liver cirrhosis. We aimed to compare risk factors, microbial aspects, and outcomes of cellulitis in compensated and decompensated hepatitis C virus (HCV)-related cirrhosis.
Methods
Six hundred twenty consecutive HCV-related cirrhotic patients were evaluated for cellulitis. Demographic and clinical data were evaluated, along with blood and skin cultures. Severity of cirrhosis was assessed using Child-Pugh score. In-hospital mortality was assessed.
Results
Seventy-seven (12.4%) cirrhotic patients had cellulitis (25 with compensated and 52 with decompensated disease). Smoking and venous insufficiency were risk factors of cellulitis in compensated cirrhosis. Leg edema, ascites, hyperbilrubinemia and hypoalbuminemia were risk factors in decompensated cirrhosis. Gram-positive bacteria (Staphylococcus spp. and Streptococcus pyogenes) were the infective organisms in compensated patients, while gram negative bacteria (Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa) were the predominant organisms in decompensated cirrhosis. Fungi (Candida albicans and Aspergillus niger) were detected in 3 decompensated cases. In-hospital mortality in patients with cellulitis was 27.3%, approaching 100% in decompensated patients with gram-negative cellulitis. Prolonged hospitalization, higher model for end-stage liver disease (MELD)-Na score, septic shock, local complication, and recurrent cellulitis were predictors of mortality.
Conclusions
Cellulitis in compensated cirrhosis is different from that of decompensated patients regarding microorganisms, pathogenesis, and prognosis. Cellulitis has a poor prognosis, with mortality rates approaching 100% in decompensated patients with gram-negative cellulitis. Stratifying patients according to severity of cirrhosis is important to identify the proper empirical antibiotic and to decide the proper means of care.
INTRODUCTION
Cellulitis is a common infectious disease in cirrhosis that develops in 10.5–12.5% [1,2]. It is responsible for significant morbidity and mortality that may require recurrent hospital admissions for early recognition and appropriate treatment [3]. Moreover, it may carry a socioeconomic burden including duration of hospitalization and high financial costs [4]. Recently, the improvement in patient management, including a high index of suspicion together with a proper use of safer prophylactic antibiotics, have significantly improved the short-term prognosis, decrease in the rate of recurrence, repeated hospitalizations and hence in-hospital mortality [5]. Several studies had discussed cellulitis in cirrhotic patients which declared that causative microorganisms, pathogenesis and prognosis were quite different from that of the general population [5].
In this study, we tried to answer some questions. First, is there a change in the causative microorganisms as an emerging of resistant or new organisms in cirrhotic patients? Second, are the microbial aspects, risk factors and clinical judgement changed with the severity of liver cirrhosis; compensated or decompensated? Third, can cellulitis affect the clinical outcomes of cirrhosis? So, we aimed to investigate the microbial aspects and the risk factors for developing cellulitis in hospitalized cirrhotic patients and their relation to the severity of cirrhosis and highlight a spot on the prognosis of cellulitis including complications and in-hospital mortality in those patients. Particularly, the shortage of data concerns these aspects of cellulitis and its sequelae in hepatitis C virus (HCV)-related liver cirrhosis.
PATIENTS AND METHODS
Study design
This prospective study was carried out at Assiut University Hospital; a tertiary care teaching hospital, Assiut, Egypt, from January 2018 to June 2018. The study was approved by the Local Ethics Committee of Assiut University Hospital and was conducted in accordance with the previsions of the Declaration of Helsinki. Informed consent was obtained from all the participants or from their relatives for patients with hepatic encephalopathy (HE) before enrollment.
Patients
Adult patients with HCV-related cirrhosis admitted to the Department of Gastroenterology and Tropical Medicine, Al-Rajhi Liver Center, Assiut University Hospital, Assiut, Egypt between January 2018 and June 2018 were consecutively included in the study and evaluated for the presence of cellulitis. The diagnosis of cirrhosis was based on clinical, laboratory, and imaging findings [6,7]. The severity of liver cirrhosis was assessed according to the Child–Pugh classification and model for end-stage liver disease (MELD) and MELD-Na scores [8-10]. Cellulitis was diagnosed by the presence of redness, warmth and swelling of the affected area [11]. According to Child–Pugh classification[8], patients were classified into a compensated (Child A) and a decompensated group (Child B and C) at diagnosis of cirrhosis.
Non-cirrhotic patients with cellulitis, cirrhotic patients with orbital cellulitis, cellulitis complicating diabetic foot ulcers, postoperative wound infection were excluded.
Methods
At study entry, a thorough medical history and physical examination were taken for data collection e.g., age, sex, co-morbidities like diabetes, peripheral edema, ascites, severity of disease and cirrhosis-related complications. Laboratory investigation including liver function tests, serum creatinine, complete blood count and serum sodium were done. Doppler ultrasound was used to diagnose deep vein thrombosis in suspicious cases. Cellulitis was assessed for its site, nature, severity, and complication and specimens of aspirate or swab from the skin lesion and blood were collected before starting empirical antibiotic therapy. In-hospital mortality was assessed.
All recruited patients were treated empirically with cefotaxime (2 g i.v./12 h) or amoxicillin–clavulanic acid (1.2 g i.v./12 h) according to the decision of their physicians and shifted to adjusted antibiotic therapy according to results of antimicrobial susceptibility testing.
Microbiologic studies
Blood samples and culture
Samples were collected from cirrhotic patients, transported and processed in the Microbiology Laboratory Unit of Department of Clinical Pathology, Assiut University Hospital, Egypt. The infective organisms were identified by the conventional and the automated methods under universal safety precautions and standard laboratory protocols [12].
Blood samples collection: Five to 10 ml of blood was collected aseptically from each patient. Two blood culture bottles aerobic and anaerobic were incubated in BacT/Alert 3D system (BioMérieux, Marcy l’Etoile, France) according to its manufacture and the specimen was considered negative after 5 days of incubation.
Gram staining was done for the positive blood culture bottles and then inoculated onto Blood agar, MacConkey agar, chocolate media, Bile Esculin Azide agar (incubated at 37o C for 24-48 hours), two plates of saboroud’s agar (one incubated at 37o C and the other at 25o C up to 14 days), all under aerobic condition. Blood agar incubated at 37o C in an anaerobic jar for 3 days, the growth was observed in the next day.
Gram staining was done for the positive growth cultures, the identification and antimicrobial susceptibility testing were performed with the VITEK 2 COMPACT-15 automated system (BioMerieux, Marcy l’Etoile, France) based on its manufacturer.
For filamentous fungal diagnosis, the visible colonies are inspected macroscopically for shape, texture and color and identified microscopically by examining the shape and the arrangement of the conidia using lactophenol cotton blue stain.
ID-GNB and AST-N223 cards were used for gram negative bacilli, ID-GP and AST-P592 cards used for gram positive cocci, IDYST and AST-Yeast07 cards for yeasts and the ID-ANC card for anaerobes. Outcomes were interpreted according to the Clinical and Laboratory Standards Institute (CLSI), 2016.
Skin samples and culture
The skin was cleaned with an alcohol for a closed lesion and with saline for opened one, epidermal scales scraped and tacked from the active edge. Swab samples inoculated on different media for isolation of the organism then identification of gram positive or negative organisms by VITEK 2 COMPACT-15 (BioMérieux) as previous.
Statistical analysis
Statistical analyses were conducted using SPSS for windows version 16 (IBM Corp., Armonk, NY, USA). The continuous data was expressed as means±standard deviation and was compared using Student’s t test or Mann-Whitney U test and one way analysis of variance. Categorical variables were expressed as a percentage and compared using chi-squared (χ2 ) or Fisher’s exact probability test. Significant factors on univariate analysis were considered for inclusion in multiple regression analysis. For all analyses, P-value<0.05 was considered statistically significant.
RESULTS
Characteristics of the studied patients
A total of 620 patients with HCV-related liver cirrhosis admitted to Department of Gastroenterology and Tropical Medicine, Al-Rajhi Liver Center, Assiut University Hospital, Assiut, Egypt, between January 2018 and June 2018 were enrolled in the study. Cellulitis was diagnosed in 12.4% (77/620) of patients (48 males and 29 females with mean age of 57.7±7.5 years). The majority of patients with cellulitis had decompensated cirrhosis “Child classes B and C (52/77, 67.5%)”, and the remaining 25 patients had compensated cirrhosis “Child class A (32.5%)”. Pain at site of cellulitis was a most common symptom (90.9%). The most common site of cellulitis was in the lower extremities which were found in 74 cases (96.1%), while the upper extremities were less frequently involved (3.9%). More than one area of cellulitis was involved in seven cases (9.1%) while nine (11.7%) cases had abscesses. In addition, six (7.8%) cases were complicated with gangrene and surgical debridement was required in four of them, while one case had hemorrhagic bullae.
In patients with compensated cirrhosis, smoking and venous insufficiency were significantly higher compared to patients with decompensated cirrhosis and those without cellulitis. Exposure to trauma was higher in compensated patients but without statistical significance. On the other hand, about 28% (7/25) of compensated patients with cellulitis did not have obvious lesions on the body surface that allow microbial invasion. However, ascites and peripheral edema were the commonest predisposing factors for cellulitis in patients with decompensated cirrhosis. In addition, patients with decompensated cirrhosis had significantly higher serum bilirubin and lower serum albumin compared to those without decompensation and cellulitis. In addition, frequencies of local complications, recurrence and septic shock were higher in patients with decompensated cirrhosis but without statistical significance (Table 1).
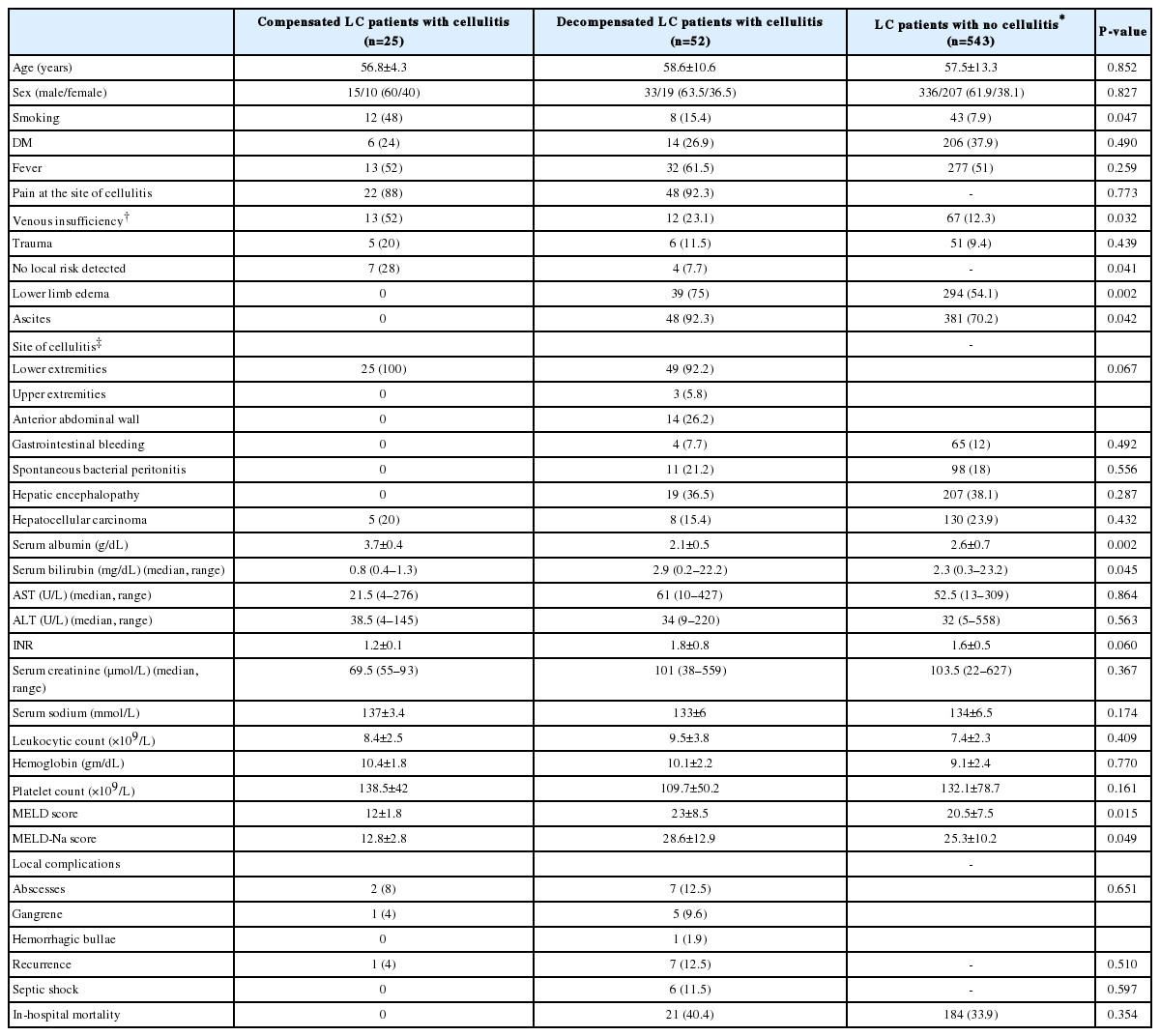
Characteristics and risk factors of cellulitis in patients with hepatitis C virus-related cirrhosis (compensated and decompensated)
Further clinical and laboratory data of the studied patients and their subgroups at and during admission were summarized in Table 1.
Of 77 cirrhotic patients with cellulitis, 28 (36.4%) cases were confirmed bacteriologically either from blood or from skin aspirates (14 from blood, 7 from skin, and 7 from both). These cases were 13 females and 15 males, with a mean age of 59.7±10.8 years. The remaining 49 patients (16 females and 33 males with a mean age of 58.1±10.2 years) had negative cultures. Gram positive bacteria were isolated from 19 specimens (10 from blood and 9 from skin), Gram negative bacteria were isolated from 24 specimens (19 from blood and 5 from skin) and three fungi (2 from blood and 1 from skin). None of the patients had anaerobic bacterial infection. The most frequent gram positive bacteria causing cellulitis was Staphylococcus species (14/19, 73.7%) with Staphylococcus aureus being the commonest (9/19, 47.4%). The most common gram negative bacteria was Escherichia coli (11/24, 45.8%). The details of microbial infections among cirrhotic patients with cellulitis were shown in Table 2 where isolated organisms were gram positive in compensated cirrhosis while gram negative bacteria were causative organisms of cellulitis in most cases of decompensated cirrhosis. Fungi were isolated in decompensated patients.
Concerning antibiotic therapy in cirrhotic patients with cellulitis, the median duration of antibiotic therapy was 7 (3–25) days. All recruited patients received empirical antibiotics (70 patients [90.9%] received cefotaxime and 7 [9.1%] received amoxicillin– clavulanic acid therapy) then 19 cases of them received adjusted antibiotic therapy according to results of antimicrobial susceptibility testing.
Twenty-one patients with cellulitis (27.3%) died during hospitalization. We found that all non-survivors (11 cases) with positive cultures were of gram negative cellulitis per se or combined infection with gram positive bacteria. Details of characteristics of bacteriologically-proved cellulitis, risk factors and treatment among the deceased cirrhotic patients were summarized in Table 3.
Determination of risk factors for in-hospital mortality in cirrhotic patients with cellulitis
Univariate analysis showed that lower limb (LL) edema, serum creatinine, sodium, International Normalized Ratio (INR), Child-Pugh, MELD and MELD-Na scores were significantly associated with in-hospital mortality in cirrhotic patients with cellulitis. In addition, prolonged hospital stay and complications registered during hospitalization; recurrent, locally complicated cellulitis and septic shock were significantly higher in deceased cases than in survivors (Table 4).
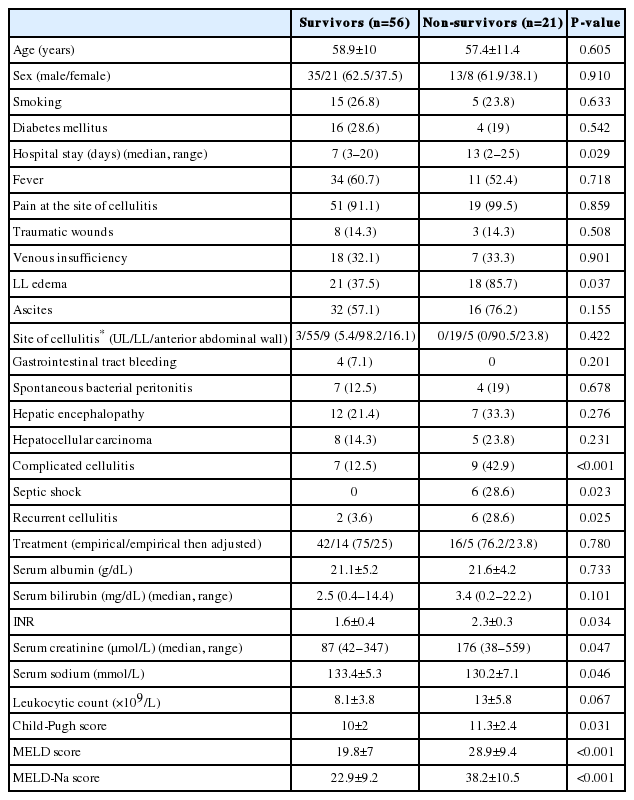
Demographic and clinical characteristics of cirrhotic patients with cellulitis (survivors and non-survivors)
In the multivariate analysis, we included the Child-Pugh and MELD-Na scores in place of INR, MELD, serum creatinine and sodium (which were the components of these scores) for prediction of in-hospital mortality in cirrhotic patients with cellulitis. As a result, prolonged hospital stay, recurrent, locally complicated cellulitis, septic shock and higher MELD-Na score were associated with in-hospital mortality (Table 5).
DISCUSSION
The current study justified to answer several questions on risk factors, microorganisms and prognosis of cellulitis in patients with compensated and decompensated cirrhosis. Infections are common complications in cirrhosis where, patients with decompensated cirrhosis were more prone to infection than compensated cirrhosis. Among cirrhotic patients cellulitis was found in 12.4% which was within the range of the earlier estimates [1,2]. This study corroborates differences between compensated and decompensated cirrhosis as regarding risk factors, microbial aspects and sequelae of cellulitis.
In this study, similar to general population [13-15], cellulitis in compensated cirrhosis occurred independently in the absence of ascites and peripheral edema, where smoking, venous insufficiency and trauma may be the predisposing factors. In addition, it may occur due to disruption of mechanical defenses following a trivial injury as itching. In line with previous studies [16,17], we found that no obvious local lesions allowing bacterial invasion could be detected in 28% of those patients.
On the other hand, peripheral edema, ascites, hyperbilirubineamia, and hypoalbumineamia were associated with cellulitis in patients with decompensated cirrhosis. Several studies reported that low serum albumin (<2.5 g/dL) and high serum bilirubin (>3 mg/dL) were significantly associated with the development of cellulitis [2,5]. Poor liver function in decompensated patients may increase the risk of developing infection which may be due to defect in bactericidal activity of immunoglobulin, decreased opsonic and neutrophil functions, complement deficiency, or reduced number of Kupffer cells and fibronectin levels [18,19].
Compatible with previous studies [2,16,17,20], peripheral edema was significantly associated with cellulitis in decompensated patients that can be explained by seeding of the bacteria in the edematous soft tissue via the bloodstream through the intestinal portal route. Mohan et al. [2], reported that cirrhotic patients usually have chronic LL edema serving as the origin of infections.
As in non-cirrhotic patients’ series [21,22], the current work reported similarly that the main etiological organisms were gram positive bacteria in compensated patients, where, Staphylococcus aureus and Streptococcus pyogenes, were the most frequent causative organisms. However, gram negative bacteria as E. coli and Klebsiella pneumoniae were the most predominant organisms in decompensated patients [2,23].
Gram negative cellulitis were seen in decompensated cirrhosis possibly due to increased bacterial translocation and intestinal overgrowth which establishing gram negative bacteremia that result either in primary septicemia or localized infections like cellulitis [5,24]. In addition, defective bactericidal function of serum immunoglobulin M for E. coli may be accused [19]. However, the increased risk of colonization by methicillin-resistant Staphylococcus aureus and Pseudomonas may be due to recurrent hospitalization or empirical widespread use of antibiotics in those patients [4].
It was the first time to report fungal infection in decompensated patients with cellulitis; Candida albicans (one case) and Aspergillus niger (two cases) in skin and blood cultures, respectively. This finding may reflect that fungal pathogens are becoming increasingly common in those immune-compromised patients with different types of infections. Candida infection could be attributed to translocation of supercolonized fungi secondary to changes in the intestinal bacterial to the extraluminal areas or direct percutaneous inoculation of fungi or preceding recognized pulmonary disease as in Aspergillus infection [25,26].
The current study reported that in-hospital mortality rate among cirrhotic patients with cellulitis was (27.3%) that much higher than that shown in previous studies (19–22%) [2,24]. Moreover, this study failed to show any significant impact of cellulitis on survival of compensated patients. Earlier studies suggested that although infections frequently develop in compensated patients, they seem to independently affect survival predominantly in those diagnosed with decompensated disease [27,28]. So, it seems that advanced hepatic cirrhosis, its related complications and aggressive cellulitis sequelae that may progress to septic shock and death have major prognostic importance in this group of patients.
We documented that all deceased patients with bacteriologically proved cellulitis were of gram negative cellulitis per se or in combination with gram positive that was compatible with Horowitz et al. [23], who supported the early diagnosis and treatment of gram negative cellulitis to avoid serious consequences. Similar to Carratalà et al. [29], we revealed that all patients with Pseudomonas aeruginosa cellulitis developed septic shock and died. So, Carratalà and colleagues suggested that the initial empirical antibiotic therapy for patients with cellulitis presenting with shock should include anti-pseudomonal agents [29].
In this study, prolonged hospital stay, higher MELD-Na score, complicated cellulitis, septic shock and recurrence of cellulitis were risk factors of in-hospital mortality of cirrhotic patients with cellulitis. Carratalà et al. [29], reported that shock at presentation was related to in-hospital mortality in patients with cellulitis. This is strongly showed the need for the prompt institution of adequate empirical antibiotic therapy. Prolonged hospital stay may partly be explained by the presence of more co-morbidities leading to higher nosocomial infection and hence death [30]. In addition, prolonged hospitalization was associated with hypoalbuminemia and renal insufficiency that were independent predictors for inhospital mortality in cirrhotic patients [29].
This study has certain strengths and limitations. This study explored the difference in risk factors, causative microorganisms and prognosis of cellulitis in compensated and decompensated cirrhosis. This is one of the very few studies which investigated fungal infection as infective organisms for cellulitis and looked into complications and factors associated with in-hospital morality in cirrhotic patients with cellulitis. In addition, we mainly assessed cellulitis in patients with HCV-related liver disease; the most common cause of cirrhosis in Egypt. Unlike earlier studies, cellulitis had been assessed in cirrhotic patients with different etiologies.
On the other hand, there were several limitations of this study. Our study was a single-center study that occurred in Assiut University Hospital; a tertiary care center, where less severe stage of cirrhosis is less possible to be admitted so, the sample may not exactly represent the general population of cirrhotic patients. The high percentage of empirical use of antimicrobials in cirrhotic patients for different reasons e.g., HE, bleeding varices or spontaneous bacterial peritonitis prophylaxis may underestimate the results of cultures. Also, we could not investigate cases of recurrent cellulitis as their lower frequency (eight cases). Therefore, further multicenter prospective studies are required to identify risk factors of recurrent cellulitis in cirrhotic patients and to investigate antibiotic prophylaxis for cellulitis in those patients who have high-risk factors.
In conclusion, cellulitis in patients with compensated cirrhosis is different from that of the decompensated patients regarding microorganisms, pathogenesis and prognosis. Cellulitis has an impact on the course of decompensated cirrhosis with a potentially poor prognosis in whom a septic shock develops with mortality rates approaching 100% in gram negative cellulitis. Stratifying patients according to the severity of liver disease is important to identify the chosen empirical antibiotic and to decide the most proper means of care; either outpatient management or hospitalization. Prolonged hospitalization, higher MELD-Na score, septic shock, recurrent and complicated cellulitis were predictors of inhospital mortality. Early diagnosis and optimal treatment of cellulitis is a crucial step in the management of those high risk patients.
Notes
Authors’ contribution
E.A.H., M.O.A., A.O.A. and N.M.A. designed and carried out the study. A.O.A. and N.M.A collected the data. E.A.H., M.O.A., A.O.A., and A.S.E.A.R. analyzed the data. E.A.H. and M.O.A wrote the paper. A.S.E.A.R. and A.O.A. critically revised the article. All of the authors have read and approved the final version to be published.
Conflict of Interest
The authors declare no conflicts of interest.
Abbreviations
CLSI
Clinical and Laboratory Standards Institute
E. coli
Escherichia coli
HE
hepatic encephalopathy
INR
international normalized ratio
LL
lower limb
MELD
model for end-stage liver disease
References
Article information Continued
Notes
Study Highlights
Cellulitis in compensated patients seems to behave as in a non-cirrhotic population regarding risk factors; smoking, venous insufficiency, and causative microorganisms; and has no significant impact on survival. In decompensated cirrhosis, poor liver function is the main risk factor, and gram-negative bacteria are the predominant agents. Cellulitis has a potentially poor prognosis, with mortality rates approaching 100% in decompensated patients with gram-negative cellulitis. Stratifying patients according to severity of cirrhosis is important to identify the proper empirical antibiotic and to decide the most proper means of care, either outpatient management or hospitalization.



