| Clin Mol Hepatol > Volume 29(Suppl); 2023 > Article |
|
ABSTRACT
Nonalcoholic fatty liver disease (NAFLD) is a leading cause of liver disease worldwide. The estimated global incidence of NAFLD is 47 cases per 1,000 population and is higher among males than females. The estimated global prevalence of NAFLD among adults is 32% and is higher among males (40%) compared to females (26%). The global prevalence of NAFLD has increased over time, from 26% in studies from 2005 or earlier to 38% in studies from 2016 or beyond. The prevalence of NAFLD varies substantially by world region, contributed by differing rates of obesity, and genetic and socioeconomic factors. The prevalence of NAFLD exceeds 40% in the Americas and South-East Asia. The prevalence of NAFLD is projected to increase significantly in multiple world regions by 2030 if current trends are left unchecked. In this review, we discuss trends in the global incidence and prevalence of NAFLD and discuss future projections.
Nonalcoholic fatty liver disease (NAFLD) is a leading cause of chronic liver disease globally [1]. It encompasses a spectrum ranging from simple hepatic steatosis to nonalcoholic steatohepatitis (NASH), which can progress to liver fibrosis and cirrhosis [2]. The global prevalence of NAFLD has been increasing over time, with a recent meta-analysis estimating that 32% of the adult population is afflicted by NAFLD [3]. This has occurred in tandem with the global obesity and diabetes epidemics [4,5]. NASH is now the fastest-rising cause of hepatocellular carcinoma worldwide [6,7] and is also the fastest-rising indication for liver transplantation in the United States [8].
A recent meta-analysis by Riazi et al. [3] estimated the incidence of NAFLD at 46.9 cases per 1,000 person-years. The incidence of NAFLD was higher in males (70.8 cases per 1,000 person-years) vs. females (26.9 cases per 1,000 person-years, P<0.0001). However, all included studies were conducted in Asia, hence it is unclear whether these data are generalizable to other parts of the world. A previous meta-analysis published in 2016 had estimated the NAFLD incidence at 52.34 per 1,000 person-years in Asia and 28.01 per 1,000 personyears in Israel [9]. Another meta-analysis focused on NAFLD in Asia reported an incidence of 50.9 per 1,000 person-years, with the highest incidence of 63 per 1,000 person-years in mainland China and the lowest incidence of 29 per 1,000 person-years in Japan (Fig. 1) [10]. The NAFLD incidence in South Korea was around 45 cases per 1,000 person-years [10,11]. Taken together, the estimates for NAFLD incidence in Asia remain consistent across several meta-analyses (Table 1).
Riazi et al. [3] pooled data from 72 studies (1,030,160 individuals) and estimated that the global prevalence of NAFLD in adults was 32% (Table 2). The prevalence was higher in males than females (40% vs. 26%, P<0.0001). The prevalence of NAFLD increased from 26% in studies from 2005 or earlier to 38% in studies from 2016 or beyond. However, data from this study by Riazi et al. [3] requires cautious interpretation, as data were available from only 17 countries, hence it is unclear if the estimates from this study are a true reflection of ŌĆśglobalŌĆÖ prevalence. The relative lack of studies emphasizes the need to improve data collection from regions such as Africa, Oceania, and South America, where data was lacking. Le et al. [12] also pooled data from 245 studies (2,699,627 individuals) and estimated the global prevalence of NAFLD at 29.8%, which is consistent with RiaziŌĆÖs findings. Likewise, in this study, there was limited or no data from Africa, Oceania, and North and South America.
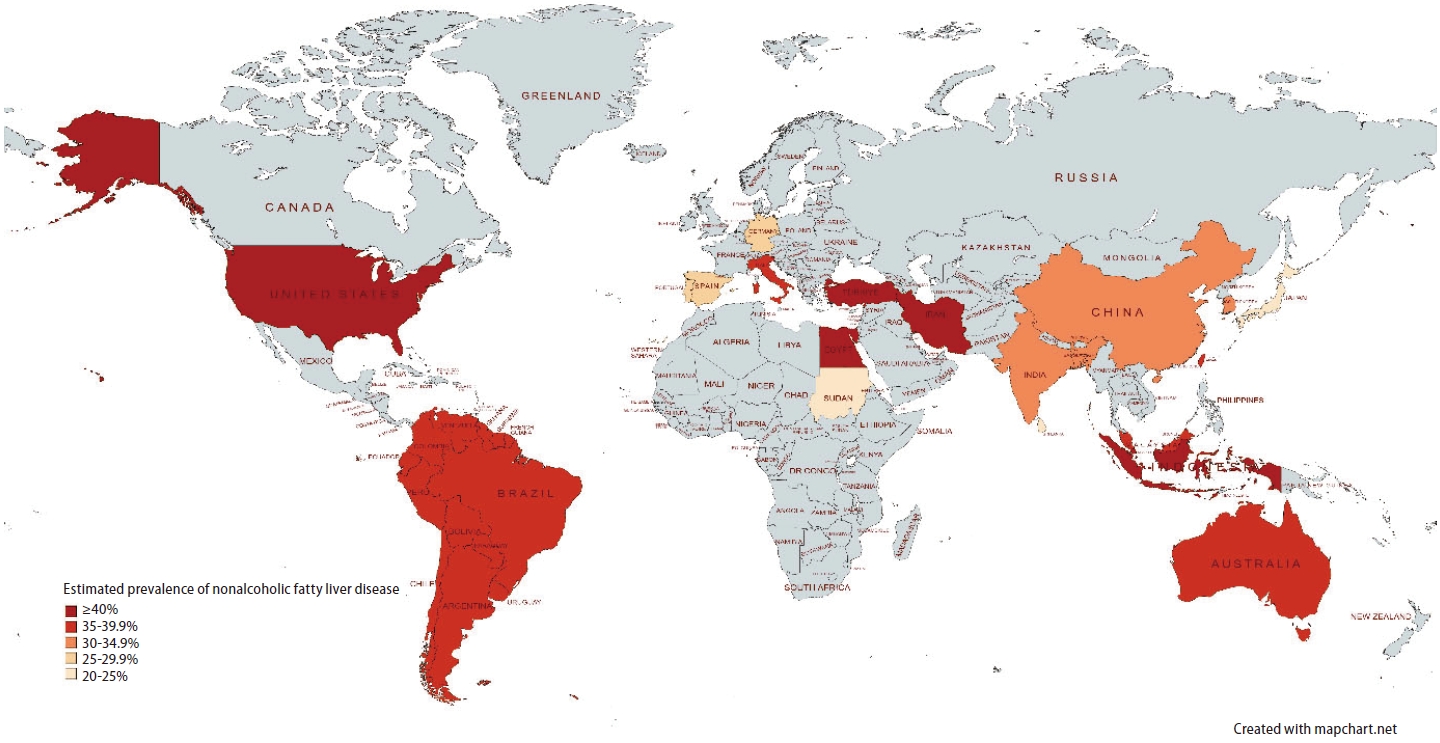
The prevalence of NAFLD varies substantially by region (Fig. 2). The overall prevalence of NAFLD in Asia is approximately 30%. A meta-analysis by Le et al. [12] conducted a literature search in 2019 (182 studies with 2,385,999 individuals) and estimated NAFLD prevalence in Asia at 30.5%. A recent meta-analysis by Riazi et al. [3] which included 63 studies (1,000,681 individuals) found that NAFLD prevalence in Asia was 31.6%. This is consistent with a previous meta-analysis by Li et al. [10] which reported NAFLD prevalence in Asia to be 29.62%.
The prevalence of NAFLD within Asia is highly variable as it encompasses countries with a wide spectrum of ethnicities and socioeconomic factors. Among Asian subregions, Southeast Asia had the highest NAFLD prevalence of 42%. Among Asian countries with more than 3 studies available, Li et al. [10] determined that the highest pooled NAFLD prevalence was in Iran (38.07%), and the lowest pooled NAFLD prevalence was in Japan (22.28%). Riazi et al. [3] determined similar results and found that Iran had the highest NAFLD prevalence (40.8%), followed by Taiwan (36.1%), South Korea (34.6%), and China (32.5%). On the other hand, Japan had a strikingly low NAFLD prevalence of 22.3%, which may be related to a low prevalence of obesity.
In China, a meta-analysis by Wu et al. [13] estimated a NAFLD prevalence of 29.88%, and another study by Zhou et al. [14] estimated that NAFLD prevalence was 29.2%. NAFLD prevalence in South Korea is also approximately 30%ŌĆöa meta-analysis by Im et al. [15] reported a NAFLD prevalence of 30.3%, and Li et al. [10] reported a similar prevalence of 32.9% [11]. A large cross-sectional study of 571,872 Korean males in their early 20s found that even among young adult males, NAFLD prevalence was 13.47%, with an increase from 10.66% in 2015 to 16.44% in 2021. There was a higher prevalence of metabolic risk factors such as hypertension, hypercholesterolemia, and hyperglycemia during the same period [16]. Another study utilizing data from Korea National Health and Nutrition Examination Survey found that NAFLD prevalence increased from 18.6% in 1998ŌĆō2001 to 21.5% in 2016ŌĆō2017, and there was a higher prevalence of obesity and diabetes over the same period [17]. These suggest that the increasing NAFLD prevalence may be driven by an increase in metabolic risk factors. Ito et al. [18] reported a comparatively lower NAFLD prevalence of 25.5% in Japan, in line with the findings by Li and Riazi. This could be attributed to a lower prevalence of obesity and diabetes in Japan compared to other countries [19,20], and may be related to a diet that is traditionally lower in fat and red meat [21].
In South Asia, India had a NAFLD prevalence of 25.7ŌĆō32.74%, Bangladesh had a NAFLD prevalence of 26.2ŌĆō33.86%, and Sri Lanka had a NAFLD prevalence of 24.74% [3,10]. In Southeast Asia, Li et al. [10] reported that NAFLD prevalence was 38.5% in Malaysia, 40.43% in Singapore, and 51.04% in Indonesia. Data from Central Asia is lacking, but the Global Burden of Disease Study (GBD) 2019 reported NAFLD prevalence in Central Asia increased from 12.4% in 1990 to 19.7% in 2019, although these estimates require cautious interpretation as the Global Burden of Disease Study relied on complex modeling and past trends when data was limited [22].
A distinct feature of the NAFLD epidemic in Asia is the high prevalence of lean NAFLD (body mass index [BMI] <23) and non-obese NAFLD (BMI <25) [23]. Up to 19% of non-obese Asians have NAFLD [24], which may be contributed to a higher percentage of visceral adiposity in Asians compared to other ethnicities [25]. Visceral adiposity plays an important role in atherogenic dyslipidemia and insulin resistance. It is a major risk factor for type 2 diabetes and has been implicated in the development and progression of NAFLD [26]. Asians also tend to develop diabetes at a younger age and lower BMI level, resulting in a longer duration of disease and increased likelihood of complications [27-29]. Worryingly, emerging data suggest that individuals with lean NAFLD may be at a higher risk of progressive liver disease, but this hypothesis requires validation [30].
Meta-analyses by Le and Riazi had similar estimates of the prevalence of NAFLD in Europe at 30.9% (11 studies with 15,062 individuals) [12] and 32.6% (7 studies with 14,111 individuals) [3], respectively. Another meta-analysis by Cholongitas et al. [31] pooled data from 17 studies (85,203 individuals) and estimated NAFLD prevalence in Europe to be 26.9%. Cholongitas also found that NAFLD prevalence in Mediterranean countries at 23.9% compared to non-Mediterranean countries at 28.5%, although the difference was not statistically significant.
Within Europe, Turkey had the highest NAFLD prevalence at 48.4%, followed by Italy at 38.2%. Germany, Portugal, and Spain had NAFLD prevalence between 25ŌĆō27% [3]. A cross-sectional study utilizing data from a large population-based cohort in France found that NAFLD prevalence in France was 18.2% [32]. A study involving individuals from population-based studies in Russia reported that NAFLD prevalence was 40% in the Ural Eye and Medical Study (UEMS) (5,852 individuals), and 69.8% in the Ural Very Old Study (UVOS) (1,130 individuals) [33]. However, it should be noted that in the UVOS, individuals were older with minimum age of 85 years, and methods for diagnosis of NAFLD differed between studies as well.
Based on subgroup data from 4 studies (18,356 individuals), Le et al. [12] estimated that the prevalence of NAFLD in North America was 35.3%. More recently, NAFLD prevalence was reported at 47.8% in the meta-analysis by Riazi which included 2 large studies with 15,178 individuals from the USA [3]. This is driven by a high prevalence of obesity in the USA. In North America, Hispanics have the highest NAFLD prevalence, followed by non-Hispanic Whites and non-Hispanic blacks [34-39]. Based on data from National Health and Nutrition Examination Surveys (NHANES) 2017ŌĆō2018, NAFLD prevalence was estimated at 63.7% in Hispanics, 56.8% in non-Hispanic whites, and 46.2% in non-Hispanic blacks [37]. This could be attributed to genetic factors like the patatin-like phospholipase domain-containing protein 3 (PNPLA3) mutation, which is associated with elevated risk for hepatic steatosis and NASH, occurring more frequently in Hispanics [40,41]. This could also be related to metabolic factors like the higher prevalence of central adiposity and insulin resistance in Hispanics compared to non-Hispanic whites [34,42]. Lower serum triglyceride levels in African-Americans may also contribute to reduced NAFLD prevalence [38].
A meta-analysis comprising 19 studies (5,626 individuals) by Rojas et al. estimated the prevalence of NAFLD in South America at up to 59% [43]. Notably, the majority of the studies included in this meta-analysis were hospital-based studies and included patients with risk factors for NAFLD, hence the results may not have been fully representative of the general population. Le et al. [12] pooled data from 3 studies (5,716 individuals) and determined that South America had the greatest estimated NAFLD prevalence among the continents at 35.7%. This may be due to a combination of genetic susceptibility and a greater prevalence of metabolic risk factors [44]. There is a high prevalence of PNPLA3 genetic polymorphism in the general population, especially among individuals with Native American ancestry [45-47]. Furthermore, obesity is extremely common in the regionŌĆöa cross-sectional study across 4 geographical regions found that central obesity was highest in South America [48]. Type 2 diabetes has also been rising in prevalence in South America [49]. Data from the meta-analysis by Le showed that compared to other regions, NAFLD individuals in South America had a higher likelihood of having diabetes and higher mean cholesterol levels [12]. In addition, physical activity is often inadequateŌĆöLatin America was ranked as the top region for physical inactivity, with a third of the population experiencing a lack of physical activity [50].
There is a paucity of data from Africa on the epidemiology of NAFLD. A meta-analysis estimated the prevalence of NAFLD in Africa at 13.5%, ranging from 9% in Nigeria to 20% in Sudan [51]. More recently, NAFLD prevalence was reported at 28.2% in the meta-analysis by Le, and 56.8% in the meta-analysis by Riazi [3,12]. Of note, the meta-analysis by Riazi only included 1 study from Egypt. The wide variation in estimates of NAFLD prevalence is likely related to a lack of reliable data from Africa [52,53].
Likewise, there is scarce data from Oceania on the incidence and prevalence of NAFLD. Population-based studies using fatty liver index have demonstrated NAFLD prevalence of 35.7ŌĆō38% in Australia [54,55]. There are no population-based studies on NAFLD prevalence using imaging modalities such as ultrasound [56].
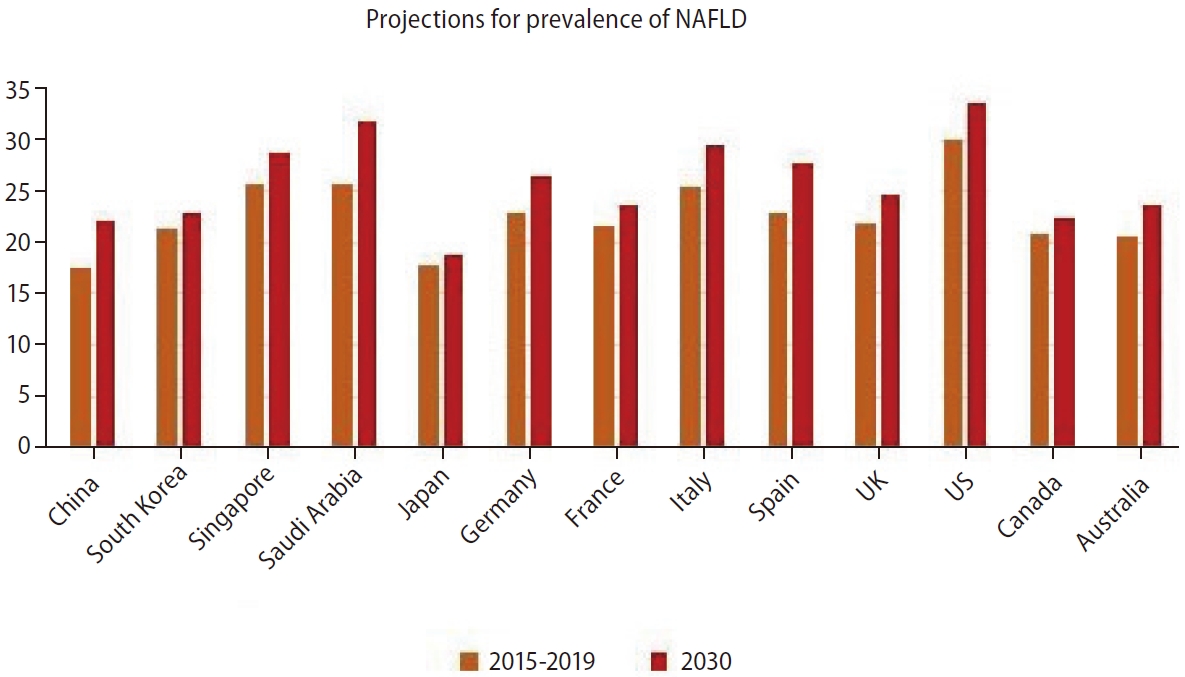
Based on mathematical modeling studies, the burden of NAFLD and NASH will continue to increase over the next 10 years worldwide (Fig. 3). The global prevalence of NAFLD is forecasted to reach 55.4% by 2040 [57]. It was estimated by Estes et al. [58] that China would have the greatest overall and relative increase in NAFLD prevalence, with the estimated number of individuals afflicted by NAFLD increasing from 243.67 million in 2016 to 314.58 million in 2030. Comparatively, Japan was forecasted to have the lowest increment in NAFLD population from 22.67 million in 2016 to 22.74 million in 2030, with an estimated prevalence of 18.8% in 2030 [58]. A similar modeling study including 4 other Asian countries predicted that Singapore would have the highest relative increase of 20% in NAFLD cases, from 1.49 million in 2019 to 1.8 million in 2030, with an expected prevalence of 28.7% in 2030 [59]. South Korea was predicted to have the lowest relative increment of 6% from 10.95 million in 2019 to 11.64 million in 2030, with an expected prevalence of 22.8% in 2030 [59]. These models were based on data on obesity prevalence and were predicated on the assumption that changes in NAFLD prevalence would occur in concordance with changes in obesity prevalence. In the Middle East, it was projected that in Saudi Arabia, NAFLD cases would increase from 8.45 million in 2017 to 12.53 million in 2030, with an expected prevalence of 31.7% by 2030; in the United Arab Emirates (UAE), NAFLD cases were projected to increase from 0.255 million in 2017 to 0.372 million in 2030, with an expected prevalence of 30.2% by 2030 [60].
In Europe, a modeling study found that between 2016 to 2030, the number of NAFLD cases could potentially increase from 13.98 million to 16.05 million in France; 18.45 million to 20.95 million in Germany; 15.22 million to 17.42 million in Italy; 10.53 million to 12.65 million in Spain; and 14.08 million to 16.92 million in the United Kingdom (UK). By 2030, the estimated prevalence of NAFLD was forecasted to be highest in Italy (29.5%), followed by Spain (27.6%), Germany (26.4%), the UK (24.7%), and France (23.6%) [58].
This trend of increasing NAFLD prevalence has also been predicted to occur in North America and Australia. A modeling study based on data from the US predicted that the number of individuals with NAFLD would increase by 21% from 83.1 million in 2015 to 100.9 million in 2030, reaching an expected prevalence of 33.5% in 2030 [61]. A separate modeling study from Canada projected that NAFLD individuals would rise by 20% from an estimated 7.76 million in 2019 to 9.31 million in 2030 [62]. A similar study from Australia estimated that NAFLD cases would increase by 25% from 5.55 million in 2019 to 7.02 million in 2030, and NAFLD prevalence was expected to rise from 22% to 23.6% in 2030 [63]. Taken together, these data suggest that the prevalence and burden of NAFLD is likely to increase across multiple world regions if current trends are left unchecked. This serves as a call to action for greater political will and resources directed toward combating metabolic risk factors for NAFLD, at a regional and global level [64,65].
In summary, the global burden of NAFLD is substantial and is projected to increase. It is important to maintain and increase data collection from all world regions to improve the understanding of the burden of disease associated with NAFLD and NASH worldwide. Improving our understanding of the burden of NAFLD can facilitate the development of healthcare policies and strategies to slow this epidemic.
FOOTNOTES
AuthorsŌĆÖ contribution
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript. The manuscript, including related data, figures and tables has not been previously published and that the manuscript is not under consideration elsewhere.
All authors approve the final version of the manuscript, including the authorship list and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Figure┬Ā2.
Estimated prevalence of nonalcoholic fatty liver disease (NAFLD). Data for Iran, China, Taiwan, South Korea, Europe (Turkey, Italy, Germany, Portugal, Spain), North America (USA), and Egypt was obtained from Riazi et al. [3]. Data for South America was obtained from Le et al. [12]. Data for South Asia (India, Bangladesh, Sri Lanka) and Southeast Asia (Indonesia, Malaysia, Singapore) was obtained from Li et al. [10]. Data for Japan was obtained from Li et al. [10] and Riazi et al. [3]. Data for Sudan was obtained from Younossi et al. [9]. Data for Australia was obtained from population-based studies by Farrell et al. [55] and Roberts et al. [54].
Figure┬Ā3.
Estimated projections for the prevalence of nonalcoholic fatty liver disease (NAFLD). Data was obtained from Estes et al. [58,59,61]. Data for Saudi Arabia was obtained from Alswat et al. [60], data for Canada was obtained from Swain et al. [62], and data for Australia was obtained from Adams et al. [63].
Table┬Ā1.
Selected meta-analyses providing data for the incidence of nonalcoholic fatty liver disease
| Study | No. of studies | No. of individuals | Study years | Regions/Countries included | Main findings | Comments |
|---|---|---|---|---|---|---|
| Riazi et al. [3] (2022) | 16 | 381,765 | 1994ŌĆō2018 | Asia (China, Japan, South Korea, Hong Kong, Israel) | Incidence 46.9 cases per 1,000 person-years; the incidence in men (70.8 cases per 1,000 person-years) was higher than in women (29.6 cases per 1,000 person-years) | The majority of included studies were from Asia hence data may not be generalizable |
| Substantial heterogeneity | ||||||
| Li et al. [10] (2019) | 18 | 416,988 | 2002ŌĆō2017 | Asia (China, Japan, South Korea, Hong Kong) | Incidence 50.9 cases per 1,000 person-years; incidence highest in China (63 per 1,000 person-years), lowest in Japan (29 per 1,000 person-years) | All studies were from Asia hence data may not be generalizable |
| Younossi et al. [9] (2016) | 5 | 4,895 | 1997ŌĆō2013 | Asia (China, Japan, Israel) | Incidence 52.34 cases per 1,000 person-years (China and Japan), 28.01 cases per 1,000 person-years (Israel) | A limited number of included studies |
| All studies were from 3 Asian countries |
Table┬Ā2.
Selected meta-analyses providing data for the prevalence of non-alcoholic fatty liver disease
| Study | No. of studies | No. of individuals | Study years | Regions/Countries included | Main findings | Comments |
|---|---|---|---|---|---|---|
| Riazi et al. [3] (2022) | 72 | 1,030,160 | 1994ŌĆō2019 | Asia (63 studies), Europe (7 studies), North America (USA only), Africa (Egypt only) | The estimated global prevalence was 32.4% | Limited data from North America and Africa; no data from South America |
| Prevalence was higher in men (39.7%) than in women (25.6%) | ||||||
| Prevalence increased over time, from 25.5% Ōēż2005 to 37.8% Ōēź2016 | ||||||
| Le et al. [12] (2021) | 245 | 5,399,254 | 1991ŌĆō2018 | Asia (182 studies), Europe (11 studies), North America (3 studies), South America (4 studies), Africa (2 studies) | Estimated global prevalence 29.8% | Limited data from North America, South America, and Africa |
| Prevalence highest in South America (35.7%) and North America (35.3%) | ||||||
| Prevalence increased from 21.9% in 1991 to 37.3% in 2019 (yearly increase 0.7%) | ||||||
| Younossi et al. [9] (2016) | 86 | 8,515,431 | 1989ŌĆō2015 | Asia (20 studies), Middle East (3 studies), Europe (21 studies), North America (35 studies), South America (3 studies), Africa (2 studies), Oceania (1 study) | Estimated global prevalence 25.2% | Limited data from South America and Africa Included case series and case-control studies |
| Prevalence highest in South America (30.5%) and the Middle East (31.8%); lowest in Africa (13.5%) | ||||||
| Rojas et al. [43] (2022) | 19 | 5,625 | South America only (Brazil, Mexico, Chile, Argentina, Peru) | Estimated overall prevalence 59%; prevalence in general and ŌĆścaptiveŌĆÖ population 24% | High heterogeneity | |
| A large proportion (2,948) were patients visiting healthcare facilities and hence susceptible to selection bias | ||||||
| Data applicable only to South America | ||||||
| Cholongitas et al. [31] (2021) | 17 | 85,203 | 2005ŌĆō2018 | Europe | Estimated overall prevalence 26.9% | Studies that used elevated aminotransferases alone as a method for diagnosis of NAFLD were included |
| Prevalence in Mediterranean countries 23.9%, non- Mediterranean countries 28.5% | ||||||
| Prevalence higher in men (32.8%) than women (19.6%) | Data are applicable only to Europe | |||||
| Li et al. [10] (2019) | 237 | 13,044,518 | 1994ŌĆō2017 | Asia | Estimated overall prevalence 29.6% | Data are applicable only to Asia |
| Prevalence increased over time ŌĆō 25.3% (1995ŌĆō2005), 28.5% (2006ŌĆō2011), 33.9% (2012ŌĆō2017) |
REFERENCES
1. Cheemerla S, Balakrishnan M. Global epidemiology of chronic liver disease. Clin Liver Dis (Hoboken) 2021;17:365-370.




2. Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018;67:328-357.



3. Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2022;7:851-861.


4. GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13-27.



5. Stefan N, Cusi K. A global view of the interplay between nonalcoholic fatty liver disease and diabetes. Lancet Diabetes Endocrinol 2022;10:284-296.


6. Tan DJH, Setiawan VW, Ng CH, Lim WH, Muthiah MD, Tan EX, et al. Global burden of liver cancer in males and females: changing etiological basis and the growing contribution of NASH. Hepatology 2022 Aug 29;doi: 10.1002/hep.32758.



7. Huang DQ, Singal AG, Kono Y, Tan DJ, El-Serag HB, Loomba R. Changing global epidemiology of liver cancer from 2010 to 2019: NASH is the fastest growing cause of liver cancer. Cell Metab 2022;34:969-977 e2.



8. Younossi ZM, Stepanova M, Ong J, Trimble G, AlQahtani S, Younossi I, et al. Nonalcoholic steatohepatitis is the most rapidly increasing indication for liver transplantation in the United States. Clin Gastroenterol Hepatol 2021;19:580-589 e5.


9. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-metaanalytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84.


10. Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999-2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2019;4:389-398.


11. Kang SH, Lee HW, Yoo JJ, Cho Y, Kim SU, Lee TH, et al. KASL clinical practice guidelines: management of nonalcoholic fatty liver disease. Clin Mol Hepatol 2021;27:363-401.




12. Le MH, Yeo YH, Li X, Li J, Zou B, Wu Y, et al. 2019 Global NAFLD prevalence: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2022;20:2809-2817 e28.


13. Wu Y, Zheng Q, Zou B, Yeo YH, Li X, Li J, et al. The epidemiology of NAFLD in Mainland China with analysis by adjusted gross regional domestic product: a meta-analysis. Hepatol Int 2020;14:259-269.



14. Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology 2019;70:1119-1133.



15. Im HJ, Ahn YC, Wang JH, Lee MM, Son CG. Systematic review on the prevalence of nonalcoholic fatty liver disease in South Korea. Clin Res Hepatol Gastroenterol 2021;45:101526.


16. Lee J, Kim T, Yang H, Bae SH. Prevalence trends of non-alcoholic fatty liver disease among young men in Korea: a Korean military population-based cross-sectional study. Clin Mol Hepatol 2022;28:196-206.




17. Park SH, Plank LD, Suk KT, Park YE, Lee J, Choi JH, et al. Trends in the prevalence of chronic liver disease in the Korean adult population, 1998-2017. Clin Mol Hepatol 2020;26:209-215.




18. Ito T, Ishigami M, Zou B, Tanaka T, Takahashi H, Kurosaki M, et al. The epidemiology of NAFLD and lean NAFLD in Japan: a metaanalysis with individual and forecasting analysis, 1995-2040. Hepatol Int 2021;15:366-379.



19. Organisation for Economic Co-operation and Development (OECD). Obesity update 2017. OECD web site, <https://www.oecd.org/health/health-systems/Obesity-Update-2017.pdf>. Accessed 22 Oct 2022.
20. International Diabetes Federation (IDF). IDF Diabetes Atlas Ninth edition 2019. IDF web site, <https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf>. Accessed 22 Oct 2022.
21. Ikeda N, Saito E, Kondo N, Inoue M, Ikeda S, Satoh T, et al. What has made the population of Japan healthy? Lancet 2011;378:1094-1105.


22. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) results. Global Health Data Exchange web site, <http://ghdx.healthdata.org/gbd-resultstool>. Accessed 22 Oct 2022.
23. Yoo JJ, Kim W, Kim MY, Jun DW, Kim SG, Yeon JE, et al. Recent research trends and updates on nonalcoholic fatty liver disease. Clin Mol Hepatol 2019;25:1-11.




25. Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/IntraAbdominal Adiposity. Am J Clin Nutr 2012;96:714-726.


26. Hanlon CL, Yuan L. Nonalcoholic fatty liver disease: the role of visceral adipose tissue. Clin Liver Dis (Hoboken) 2022;19:106-110.




27. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681-1688.


28. Huxley R, James WP, Barzi F, Patel JV, Lear SA, Suriyawongpaisal P, et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes Rev 2008;9 Suppl 1:53-61.


29. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129-2140.


30. Hagstr├Čm H, Nasr P, Ekstedt M, Hammar U, St├źl P, Hultcrantz R, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term followup study. Hepatol Commun 2018;2:48-57.




31. Cholongitas E, Pavlopoulou I, Papatheodoridi M, Markakis GE, Bouras E, Haidich AB, et al. Epidemiology of nonalcoholic fatty liver disease in Europe: a systematic review and meta-analysis. Ann Gastroenterol 2021;34:404-414.



32. Nabi O, Lacombe K, Boursier J, Mathurin P, Zins M, Serfaty L. Prevalence and risk factors of nonalcoholic fatty liver disease and advanced fibrosis in general population: the French Nationwide NASH-CO Study. Gastroenterology 2020;159:791-793.e2.


33. Bikbov MM, Gilmanshin TR, Zainullin RM, Kazakbaeva GM, Iakupova EM, Fakhretdinova AA, et al. Prevalence of non-alcoholic fatty liver disease in the Russian Ural Eye and Medical Study and the Ural Very Old Study. Sci Rep 2022;12:7842.




34. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 2004;40:1387-1395.


35. Lazo M, Hernaez R, Eberhardt MS, Bonekamp S, Kamel I, Guallar E, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol 2013;178:38-45.



36. Kim D, Kim W, Adejumo AC, Cholankeril G, Tighe SP, Wong RJ, et al. Race/ethnicity-based temporal changes in prevalence of NAFLD-related advanced fibrosis in the United States, 2005-2016. Hepatol Int 2019;13:205-213.



37. Zhang X, Heredia NI, Balakrishnan M, Thrift AP. Prevalence and factors associated with NAFLD detected by vibration controlled transient elastography among US adults: results from NHANES 2017-2018. PLoS One 2021;16:e0252164.



38. Sherif ZA, Saeed A, Ghavimi S, Nouraie SM, Laiyemo AO, Brim H, et al. Global epidemiology of nonalcoholic fatty liver disease and perspectives on US minority populations. Dig Dis Sci 2016;61:1214-1225.




39. Arshad T, Golabi P, Henry L, Younossi ZM. Epidemiology of nonalcoholic fatty liver disease in North America. Curr Pharm Des 2020;26:993-997.


40. Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 2008;40:1461-1465.




41. Wagenknecht LE, Palmer ND, Bowden DW, Rotter JI, Norris JM, Ziegler J, et al. Association of PNPLA3 with non-alcoholic fatty liver disease in a minority cohort: the Insulin Resistance Atherosclerosis Family Study. Liver Int 2011;31:412-416.



42. Guerrero R, Vega GL, Grundy SM, Browning JD. Ethnic differences in hepatic steatosis: an insulin resistance paradox? Hepatology 2009;49:791-801.



43. Rojas YAO, Cuellar CLV, Barr├│n KMA, Arab JP, Miranda AL. Nonalcoholic fatty liver disease prevalence in Latin America: a systematic review and meta-analysis. Ann Hepatol 2022;27:100706.


44. Pinto Marques Souza de Oliveira C, Pinchemel Cotrim H, Arrese M. Nonalcoholic fatty liver disease risk factors in Latin American populations: current scenario and perspectives. Clin Liver Dis (Hoboken) 2019;13:39-42.




45. Arrese M, Arab JP, Riquelme A, Ben├Łtez CE, Barrera F, Soza A, et al. High prevalence of PNPLA3 rs738409 (I148M) polymorphism in Chilean latino population and its association to nonalcoholic fatty liver disease risk and histological disease severity. Hepatology 2015;62 Suppl 1:1285A.
46. Pontoriero AC, Trinks J, Hulaniuk ML, Caputo M, Fortuny L, Pratx LB, et al. Influence of ethnicity on the distribution of genetic polymorphisms associated with risk of chronic liver disease in South American populations. BMC Genet 2015;16:93.




47. Chinchilla-L├│pez P, Ram├Łrez-P├®rez O, Cruz-Ram├│n V, CanizalesQuinteros S, Dom├Łnguez-L├│pez A, Ponciano-Rodr├Łguez G, et al. More evidence for the genetic susceptibility of Mexican population to nonalcoholic fatty liver disease through PNPLA3. Ann Hepatol 2018;17:250-255.


48. Patel SA, Ali MK, Alam D, Yan LL, Levitt NS, Bernabe-Ortiz A, et al. Obesity and its relation with diabetes and hypertension: a cross-sectional study across 4 geographical regions. Glob Heart 2016;11:71-79.e4.



49. Gallardo-Rinc├│n H, Cantoral A, Arrieta A, Espinal C, Magnus MH, Palacios C, et al. Review: type 2 diabetes in Latin America and the Caribbean: regional and country comparison on prevalence, trends, costs and expanded prevention. Prim Care Diabetes 2021;15:352-359.


50. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1┬Ę9 million participants. Lancet Glob Health 2018;6:e1077-e1086. Erratum in: Lancet Glob Health 2019;7:e36.
51. Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15:11-20.



52. Spearman CW, Afihene M, Betiku O, Bobat B, Cunha L, Kassianides C, et al. Epidemiology, risk factors, social determinants of health, and current management for non-alcoholic fatty liver disease in sub-Saharan Africa. Lancet Gastroenterol Hepatol 2021;6:1036-1046.


53. Ge X, Zheng L, Wang M, Du Y, Jiang J. Prevalence trends in nonalcoholic fatty liver disease at the global, regional and national levels, 1990-2017: a population-based observational study. BMJ Open 2020;10:e036663.



54. Roberts SK, Majeed A, Glenister K, Magliano D, Lubel JS, Bourke L, et al. Prevalence of non-alcoholic fatty liver disease in regional Victoria: a prospective population-based study. Med J Aust 2021;215:77-82.



55. Farrell AM, Magliano DJ, Shaw JE, Thompson AJ, Croagh C, Ryan MC, et al. A problem of proportions: estimates of metabolic associated fatty liver disease and liver fibrosis in Australian adults in the nationwide 2012 AusDiab Study. Sci Rep 2022;12:1956.




56. Mahady SE, Adams LA. Burden of non-alcoholic fatty liver disease in Australia. J Gastroenterol Hepatol 2018;33 Suppl 1:1-11.



57. Le MH, Yeo YH, Zou B, Barnet S, Henry L, Cheung R, et al. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical bayesian approach. Clin Mol Hepatol 2022;28:841-850.




58. Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol 2018;69:896-904.


59. Estes C, Chan HL, Chien RN, Chuang WL, Fung J, Goh GB, et al. Modelling NAFLD disease burden in four Asian regions-2019-2030. Aliment Pharmacol Ther 2020;51:801-811.




60. Alswat K, Aljumah AA, Sanai FM, Abaalkhail F, Alghamdi M, Al Hamoudi WK, et al. Nonalcoholic fatty liver disease burden - Saudi Arabia and United Arab Emirates, 2017-2030. Saudi J Gastroenterol 2018;24:211-219. Erratum in: Saudi J Gastroenterol 2018;24:255.
61. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018;67:123-133.




62. Swain MG, Ramji A, Patel K, Sebastiani G, Shaheen AA, Tam E, et al. Burden of nonalcoholic fatty liver disease in Canada, 2019-2030: a modelling study. CMAJ Open 2020;8:E429-E436.



63. Adams LA, Roberts SK, Strasser SI, Mahady SE, Powell E, Estes C, et al. Nonalcoholic fatty liver disease burden: Australia, 2019-2030. J Gastroenterol Hepatol 2020;35:1628-1635.




-
METRICS

- ORCID iDs
-
Daniel Q. Huang

https://orcid.org/0000-0002-5165-5061Mark D. Muthiah

https://orcid.org/0000-0002-9724-4743 - Related articles
-
Recent updates on pharmacologic therapy in non-alcoholic fatty liver disease2024 January;30(1)
Letter regarding ŌĆ£Risk factors in nonalcoholic fatty liver diseaseŌĆØ2023 October;29(4)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



