1. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-394.


2. Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401-406.


4. Andrews J, Guyatt G, Oxman AD, Alderson P, Dahm P, Falck-Ytter Y, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol 2013;66:719-725.


7. Grønbæk L, Vilstrup H, Jepsen P. Autoimmune hepatitis in Denmark: incidence, prevalence, prognosis, and causes of death. A nationwide registry-based cohort study. J Hepatol 2014;60:612-617.


8. Danielsson Borssén Å, Marschall HU, Bergquist A, Rorsman F, Weiland O, Kechagias S, et al. Epidemiology and causes of death in a Swedish cohort of patients with autoimmune hepatitis. Scand J Gastroenterol 2017;52:1022-1028.

9. Lamba M, Ngu JH, Stedman CAM. Trends in incidence of autoimmune liver diseases and increasing incidence of autoimmune hepatitis. Clin Gastroenterol Hepatol 2021;19:573-579.e1.


11. Tunio NA, Mansoor E, Sheriff MZ, Cooper GS, Sclair SN, Cohen SM. Epidemiology of autoimmune hepatitis (AIH) in the United States between 2014 and 2019: A population-based national study. J Clin Gastroenterol 2021;55:903-910.


13. Czaja AJ, Strettell MD, Thomson LJ, Santrach PJ, Moore SB, Donaldson PT, et al. Associations between alleles of the major histocompatibility complex and type 1 autoimmune hepatitis. Hepatology 1997;25:317-323.


14. Vázquez-García MN, Aláez C, Olivo A, Debaz H, Pérez-Luque E, Burguete A, et al. MHC class II sequences of susceptibility and protection in Mexicans with autoimmune hepatitis. J Hepatol 1998;28:985-990.


16. Lim YS, Oh HB, Choi SE, Kwon OJ, Heo YS, Lee HC, et al. Susceptibility to type 1 autoimmune hepatitis is associated with shared amino acid sequences at positions 70-74 of the HLA-DRB1 molecule. J Hepatol 2008;48:133-139.


17. Krawitt EL. Autoimmune hepatitis. N Engl J Med 2006;354:54-66.


20. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis. J Hepatol 2015;63:971-1004. Erratum in: J Hepatol 2015;63:1543-1544.
22. Feld JJ, Dinh H, Arenovich T, Marcus VA, Wanless IR, Heathcote EJ. Autoimmune hepatitis: effect of symptoms and cirrhosis on natural history and outcome. Hepatology 2005;42:53-62.


23. Muratori P, Fabbri A, Lalanne C, Lenzi M, Muratori L. Autoimmune liver disease and concomitant extrahepatic autoimmune disease. Eur J Gastroenterol Hepatol 2015;27:1175-1179.


24. Muratori P, Lalanne C, Barbato E, Fabbri A, Cassani F, Lenzi M, et al. Features and progression of asymptomatic autoimmune hepatitis in Italy. Clin Gastroenterol Hepatol 2016;14:139-146.


28. Yasui S, Fujiwara K, Okitsu K, Yonemitsu Y, Ito H, Yokosuka O. Importance of computed tomography imaging features for the diagnosis of autoimmune acute liver failure. Hepatol Res 2012;42:42-50.


29. Bittermann T, Lewis JD, Levy C, Goldberg DS. Sociodemographic and geographic differences in the US epidemiology of autoimmune hepatitis with and without cirrhosis. Hepatology 2023;77:367-378 Erratum in: Hepatology 2023 Feb 21. doi:
10.1097/HEP.0000000000000348.



32. Mieli-Vergani G, Vergani D, Baumann U, Czubkowski P, Debray D, Dezsofi A, et al. Diagnosis and management of pediatric autoimmune liver disease: ESPGHAN hepatology committee position statement. J Pediatr Gastroenterol Nutr 2018;66:345-360.


33. Czaja AJ, Manns MP. The validity and importance of subtypes in autoimmune hepatitis: a point of view. Am J Gastroenterol 1995;90:1206-1211.

34. Kim BH, Kim YJ, Jeong SH, Tak WY, Ahn SH, Lee YJ, et al. Clinical features of autoimmune hepatitis and comparison of two diagnostic criteria in Korea: a nationwide, multicenter study. J Gastroenterol Hepatol 2013;28:128-134.


35. Chung DL, Seo JK, Yang HR, Ko JS, Park SH. Clinical characteristics, histology and prognosis of autoimmune hepatitis in Korean children. Korean J Pediatr Gastroenterol Nutr 2004;7:186-196.


37. Jiménez-Rivera C, Ling SC, Ahmed N, Yap J, Aglipay M, Barrowman N, et al. Incidence and characteristics of autoimmune hepatitis. Pediatrics 2015;136:e1237-e1248.


39. Homberg JC, Abuaf N, Bernard O, Islam S, Alvarez F, Khalil SH, et al. Chronic active hepatitis associated with antiliver/kidney microsome antibody type 1: a second type of “autoimmune” hepatitis. Hepatology 1987;7:1333-1339.


40. Muratori P, Lalanne C, Fabbri A, Cassani F, Lenzi M, Muratori L. Type 1 and type 2 autoimmune hepatitis in adults share the same clinical phenotype. Aliment Pharmacol Ther 2015;41:1281-1287.


41. Gregorio GV, Portmann B, Reid F, Donaldson PT, Doherty DG, McCartney M, et al. Autoimmune hepatitis in childhood: a 20-year experience. Hepatology 1997;25:541-547.


42. Abu Faddan NH, Abdel-Baky L, Aly SA, Rashed HA. Clinico-laboratory study on children with auto-immune hepatitis in Upper Egypt. Arab J Gastroenterol 2011;12:178-183.


43. Nares-Cisneros J, Jaramillo-Rodríguez Y. Autoimmune hepatitis in children: progression of 20 cases in northern Mexico. Rev Gastroenterol Mex 2014;79:238-243 English, Spanish.


44. Czaja AJ. Behavior and significance of autoantibodies in type 1 autoimmune hepatitis. J Hepatol 1999;30:394-401.


47. Wang QX, Jiang WJ, Miao Q, Xiao X, Zhang HY, Huang SS, et al. Clinical and histological features of autoantibody-negative autoimmune hepatitis in Chinese patients: a single center experience. J Dig Dis 2013;14:175-180.


49. Boberg KM, Chapman RW, Hirschfield GM, Lohse AW, Manns MP, Schrumpf E; International Autoimmune Hepatitis Group. Overlap syndromes: the International Autoimmune Hepatitis Group (IAIHG) position statement on a controversial issue. J Hepatol 2011;54:374-385.


51. Trivedi PJ, Hirschfield GM. Review article: overlap syndromes and autoimmune liver disease. Aliment Pharmacol Ther 2012;36:517-533.


52. O’Brien C, Joshi S, Feld JJ, Guindi M, Dienes HP, Heathcote EJ. Long-term follow-up of antimitochondrial antibody-positive autoimmune hepatitis. Hepatology 2008;48:550-556.


53. Poupon R, Chazouilleres O, Corpechot C, Chrétien Y. Development of autoimmune hepatitis in patients with typical primary biliary cirrhosis. Hepatology 2006;44:85-90.


55. Abdalian R, Dhar P, Jhaveri K, Haider M, Guindi M, Heathcote EJ. Prevalence of sclerosing cholangitis in adults with autoimmune hepatitis: evaluating the role of routine magnetic resonance imaging. Hepatology 2008;47:949-957.


56. Bittencourt PL, Farias AQ, Porta G, Cançado EL, Miura I, Pugliese R, et al. Frequency of concurrent autoimmune disorders in patients with autoimmune hepatitis: effect of age, gender, and genetic background. J Clin Gastroenterol 2008;42:300-305.

57. Efe C, Wahlin S, Ozaslan E, Berlot AH, Purnak T, Muratori L, et al. Autoimmune hepatitis/primary biliary cirrhosis overlap syndrome and associated extrahepatic autoimmune diseases. Eur J Gastroenterol Hepatol 2012;24:531-534.


60. Czaja AJ, Carpenter HA. Distinctive clinical phenotype and treatment outcome of type 1 autoimmune hepatitis in the elderly. Hepatology 2006;43:532-538.


62. Zeng Q, Zhao L, Wang C, Gao M, Han X, Chen C, et al. Relationship between autoimmune liver disease and autoimmune thyroid disease: a cross-sectional study. Scand J Gastroenterol 2020;55:216-221.


63. Adiga A, Nugent K. Lupus hepatitis and autoimmune hepatitis (Lupoid Hepatitis). Am J Med Sci 2017;353:329-335.


64. Kofman S, Johnson GC, Zimmerman HJ. Apparent hepatic dysfunction in lupus erythematosus. AMA Arch Intern Med 1955;95:669-676.


65. Efe C, Purnak T, Ozaslan E, Ozbalkan Z, Karaaslan Y, Altiparmak E, et al. Autoimmune liver disease in patients with systemic lupus erythematosus: a retrospective analysis of 147 cases. Scand J Gastroenterol 2011;46:732-737.


66. Runyon BA, LaBrecque DR, Anuras S. The spectrum of liver disease in systemic lupus erythematosus. Report of 33 histologically-proved cases and review of the literature. Am J Med 1980;69:187-194.


67. Lim DH, Kim YG, Lee D, Min Ahn S, Hong S, Lee CK, et al. Immunoglobulin G levels as a prognostic factor for autoimmune hepatitis combined with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2016;68:995-1002.


68. Selmi C, Generali E, Gershwin ME. Rheumatic manifestations in autoimmune liver disease. Rheum Dis Clin North Am 2018;44:65-87.


69. Cristansson J. Corneal changes in a case of hepatitis. Acta Ophthalmol (Copenh) 1954;32:161-164.


70. Karp JK, Akpek EK, Anders RA. Autoimmune hepatitis in patients with primary Sjögren’s syndrome: a series of two-hundred and two patients. Int J Clin Exp Pathol 2010;3:582-586.


73. Perdigoto R, Carpenter HA, Czaja AJ. Frequency and significance of chronic ulcerative colitis in severe corticosteroid-treated autoimmune hepatitis. J Hepatol 1992;14:325-331.


75. Liberal R, Grant CR, Mieli-Vergani G, Vergani D. Autoimmune hepatitis: a comprehensive review. J Autoimmun 2013;41:126-139.


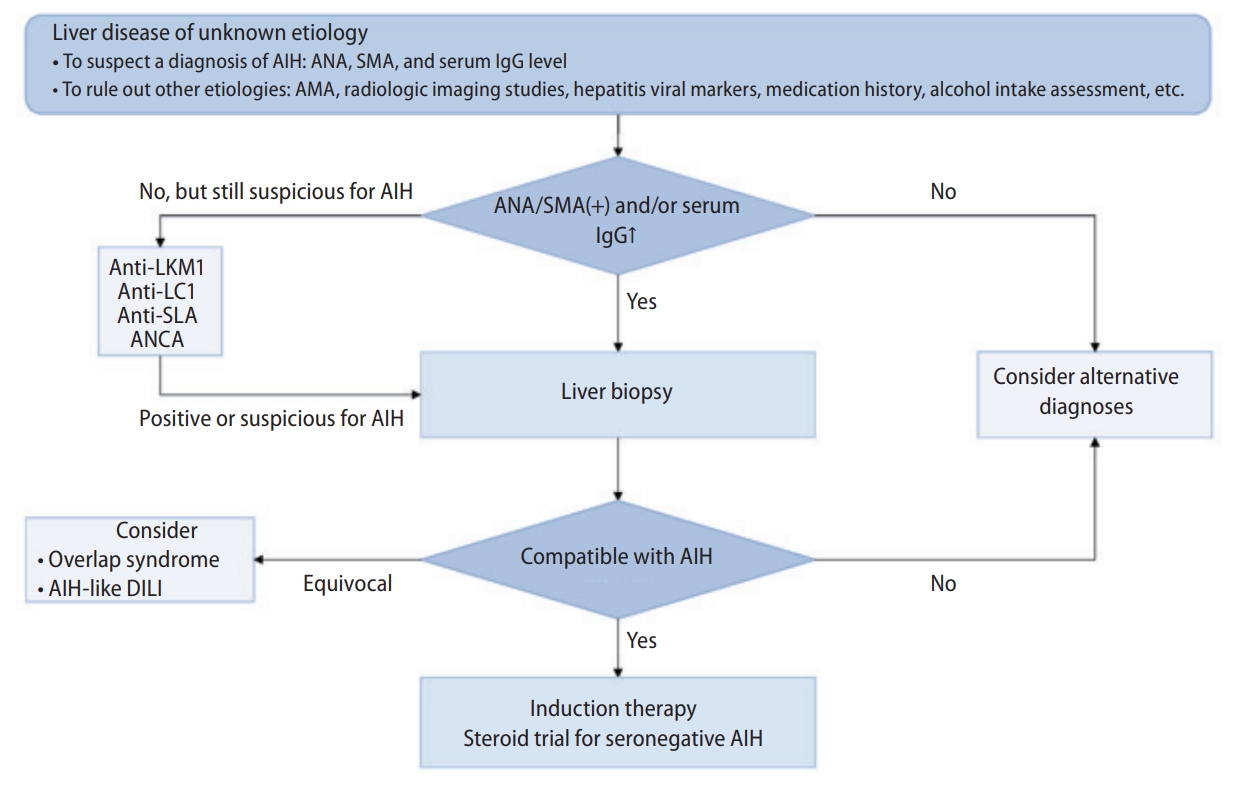
78. Lim K, Park JG. Diagnostic approach to autoimmune hepatitis. Korean J Med 2022;97:33-41.


80. Zachou K, Muratori P, Koukoulis GK, Granito A, Gatselis N, Fabbri A, et al. Review article: autoimmune hepatitis -- current management and challenges. Aliment Pharmacol Ther 2013;38:887-913.


81. Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al.; International Autoimmune Hepatitis Group. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 2008;48:169-176.


84. Björnsson E, Talwalkar J, Treeprasertsuk S, Neuhauser M, Lindor K. Patients with typical laboratory features of autoimmune hepatitis rarely need a liver biopsy for diagnosis. Clin Gastroenterol Hepatol 2011;9:57-63.


86. Terziroli Beretta-Piccoli B, Mieli-Vergani G, Vergani D. The clinical usage and definition of autoantibodies in immune-mediated liver disease: A comprehensive overview. J Autoimmun 2018;95:144-158.


87. Wies I, Brunner S, Henninger J, Herkel J, Kanzler S, Meyer zum Büschenfelde KH, et al. Identification of target antigen for SLA/LP autoantibodies in autoimmune hepatitis. Lancet 2000;355:1510-1515.


89. Targan SR, Landers C, Vidrich A, Czaja AJ. High-titer antineutrophil cytoplasmic antibodies in type-1 autoimmune hepatitis. Gastroenterology 1995;108:1159-1166.


90. Farias AQ, Gonçalves LL, Bittencourt PL, De Melo ES, Abrantes-Lemos CP, Porta G, et al. Applicability of the IAIHG scoring system to the diagnosis of antimitochondrial/anti-M2 seropositive variant form of autoimmune hepatitis. J Gastroenterol Hepatol 2006;21:887-893.


91. Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune hepatitis group report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 1999;31:929-938.


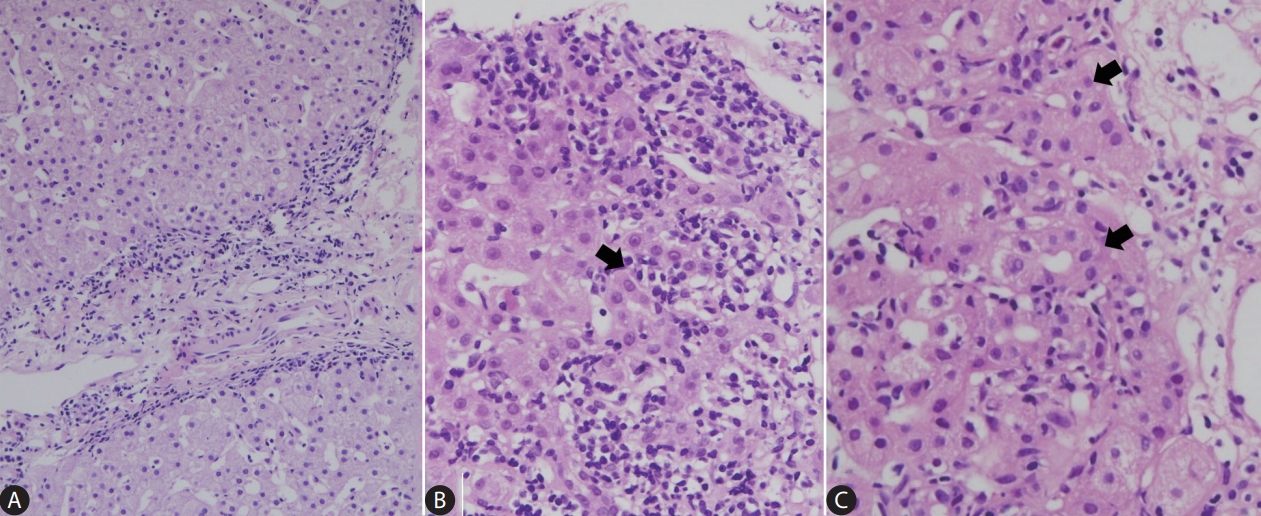
93. Lohse AW, Sebode M, Bhathal PS, Clouston AD, Dienes HP, Jain D, et al. Consensus recommendations for histological criteria of autoimmune hepatitis from the International AIH Pathology Group: Results of a workshop on AIH histology hosted by the European Reference Network on Hepatological Diseases and the European Society of Pathology: Results of a workshop on AIH histology hosted by the European Reference Network on Hepatological Diseases and the European Society of Pathology. Liver Int 2022;42:1058-1069.

94. Nguyen Canh H, Harada K, Ouchi H, Sato Y, Tsuneyama K, Kage M, et al.; Intractable Liver and Biliary Diseases Study Group of Japan. Acute presentation of autoimmune hepatitis: a multicentre study with detailed histological evaluation in a large cohort of patients. J Clin Pathol 2017;70:961-969.


95. Miyake Y, Iwasaki Y, Kobashi H, Yasunaka T, Ikeda F, Takaki A, et al. Autoimmune hepatitis with acute presentation in Japan. Dig Liver Dis 2010;42:51-54.


96. de Boer YS, van Nieuwkerk CM, Witte BI, Mulder CJ, Bouma G, Bloemena E. Assessment of the histopathological key features in autoimmune hepatitis. Histopathology 2015;66:351-362.


97. Guido M, Rugge M. Liver biopsy sampling in chronic viral hepatitis. Semin Liver Dis 2004;24:89-97.


98. Colloredo G, Guido M, Sonzogni A, Leandro G. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol 2003;39:239-244.


99. Palmer T, Georgiades I, Treanor D, Wright A, Shah M, Khosla R, et al. Improved tissue sections for medical liver biopsies: a comparison of 16 vs 18 g biopsy needles using digital pathology. J Clin Pathol 2014;67:415-419.


100. Johnson PJ, McFarlane IG. Meeting report: International autoimmune hepatitis group. Hepatology 1993;18:998-1005.


101. Czaja AJ. Performance parameters of the diagnostic scoring systems for autoimmune hepatitis. Hepatology 2008;48:1540-1548.


102. Miyake Y, Iwasaki Y, Kobashi H, Yasunaka T, Ikeda F, Takaki A, et al. Clinical features of autoimmune hepatitis diagnosed based on simplified criteria of the International Autoimmune Hepatitis Group. Dig Liver Dis 2010;42:210-215.


103. Lee YN, Kim YS, Kim SG, Lim JH, Jeong SW, Jang JY, et al. Diagnostic value and utility of the simplified international autoimmune hepatitis group (IAIHG) criteria for autoimmune hepatitis in Korea. Korean J Med 2011;81:340-350.
105. Kuiper EM, Zondervan PE, van Buuren HR. Paris criteria are effective in diagnosis of primary biliary cirrhosis and autoimmune hepatitis overlap syndrome. Clin Gastroenterol Hepatol 2010;8:530-534.


106. Chazouillères O, Wendum D, Serfaty L, Montembault S, Rosmorduc O, Poupon R. Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: clinical features and response to therapy. Hepatology 1998;28:296-301.


107. Kim MS, Kim YS, Kim SG, Byun JM, Yoon LY, Han DH, et al. The clinical significance of simplified scoring criteria as a diagnostic tool for overlap syndrome in Korea. Korean J Med 2013;84:211-220.

108. Czaja AJ. Cholestatic phenotypes of autoimmune hepatitis. Clin Gastroenterol Hepatol 2014;12:1430-1438.


109. Kaya M, Angulo P, Lindor KD. Overlap of autoimmune hepatitis and primary sclerosing cholangitis: an evaluation of a modified scoring system. J Hepatol 2000;33:537-542.


110. Björnsson E, Talwalkar J, Treeprasertsuk S, Kamath PS, Takahashi N, Sanderson S, et al. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology 2010;51:2040-2048.


112. Licata A, Maida M, Cabibi D, Butera G, Macaluso FS, Alessi N, et al. Clinical features and outcomes of patients with drug-induced autoimmune hepatitis: a retrospective cohort study. Dig Liver Dis 2014;46:1116-1120.


113. deLemos AS, Foureau DM, Jacobs C, Ahrens W, Russo MW, Bonkovsky HL. Drug-induced liver injury with autoimmune features. Semin Liver Dis 2014;34:194-204.


115. Liu ZX, Kaplowitz N. Immune-mediated drug-induced liver disease. Clin Liver Dis 2002;6:755-774.


118. Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, García-Ruiz E, et al.; Spanish Group for the Study of Drug-Induced Liver Disease. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology 2005;129:512-521.


119. Robles-Diaz M, Lucena MI, Kaplowitz N, Stephens C, Medina-Cáliz I, González-Jimenez A, et al.; Spanish DILI Registry; SLatinDILI Network; Safer and Faster Evidence-based Translation Consortium. Use of Hy’s law and a new composite algorithm to predict acute liver failure in patients with drug-induced liver injury. Gastroenterology 2014;147:109-118.e5.


123. Poynard T, Ngo Y, Perazzo H, Munteanu M, Lebray P, Moussalli J, et al. Prognostic value of liver fibrosis biomarkers: a meta-analysis. Gastroenterol Hepatol (N Y) 2011;7:445-454.


124. Poynard T, de Ledinghen V, Zarski JP, Stanciu C, Munteanu M, Vergniol J, et al.; Fibrosis-TAGS group. Relative performances of FibroTest, Fibroscan, and biopsy for the assessment of the stage of liver fibrosis in patients with chronic hepatitis C: a step toward the truth in the absence of a gold standard. J Hepatol 2012;56:541-548.


125. Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003;38:518-526.


126. Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al.; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006;43:1317-1325.


128. Parkes J, Roderick P, Harris S, Day C, Mutimer D, Collier J, et al. Enhanced liver fibrosis test can predict clinical outcomes in patients with chronic liver disease. Gut 2010;59:1245-1251.


129. Parkes J, Guha IN, Roderick P, Harris S, Cross R, Manos MM, et al. Enhanced Liver Fibrosis (ELF) test accurately identifies liver fibrosis in patients with chronic hepatitis C. J Viral Hepat 2011;18:23-31.


134. Hartl J, Denzer U, Ehlken H, Zenouzi R, Peiseler M, Sebode M, et al. Transient elastography in autoimmune hepatitis: Timing determines the impact of inflammation and fibrosis. J Hepatol 2016;65:769-775.


135. Hartl J, Ehlken H, Sebode M, Peiseler M, Krech T, Zenouzi R, et al. Usefulness of biochemical remission and transient elastography in monitoring disease course in autoimmune hepatitis. J Hepatol 2018;68:754-763.


137. Guo L, Zheng L, Hu L, Zhou H, Yu L, Liang W. Transient Elastography (FibroScan) performs better than non-invasive markers in assessing liver fibrosis and cirrhosis in autoimmune hepatitis patients. Med Sci Monit 2017;23:5106-5112.

140. Xing X, Yan Y, Shen Y, Xue M, Wang X, Luo X, et al. Liver fibrosis with two-dimensional shear-wave elastography in patients with autoimmune hepatitis. Expert Rev Gastroenterol Hepatol 2020;14:631-638.

145. Manns MP, Czaja AJ, Gorham JD, Krawitt EL, Mieli-Vergani G, Vergani D, et al.; American Association for the Study of Liver Diseases. Diagnosis and management of autoimmune hepatitis. Hepatology 2010;51:2193-2213.


146. Montano-Loza AJ, Carpenter HA, Czaja AJ. Improving the end point of corticosteroid therapy in type 1 autoimmune hepatitis to reduce the frequency of relapse. Am J Gastroenterol 2007;102:1005-1012.


147. Miyake Y, Iwasaki Y, Terada R, Okamaoto R, Ikeda H, Makino Y, et al. Persistent elevation of serum alanine aminotransferase levels leads to poor survival and hepatocellular carcinoma development in type 1 autoimmune hepatitis. Aliment Pharmacol Ther 2006;24:1197-1205.


148. Hoeroldt B, McFarlane E, Dube A, Basumani P, Karajeh M, Campbell MJ, et al. Long-term outcomes of patients with autoimmune hepatitis managed at a nontransplant center. Gastroenterology 2011;140:1980-1989.


150. Pape S, Snijders RJALM, Gevers TJG, Chazouilleres O, Dalekos GN, Hirschfield GM, et al.; International Autoimmune Hepatitis Group (IAIHG) collaborators. Systematic review of response criteria and endpoints in autoimmune hepatitis by the International Autoimmune Hepatitis Group. J Hepatol 2022;76:841-849.

151. Muratori L, Muratori P, Lanzoni G, Ferri S, Lenzi M. Application of the 2010 American Association for the study of liver diseases criteria of remission to a cohort of Italian patients with autoimmune hepatitis. Hepatology 2010;52:1857 author reply 1857-1858.


152. Verma S, Gunuwan B, Mendler M, Govindrajan S, Redeker A. Factors predicting relapse and poor outcome in type I autoimmune hepatitis: role of cirrhosis development, patterns of transaminases during remission and plasma cell activity in the liver biopsy. Am J Gastroenterol 2004;99:1510-1516.


153. Lüth S, Herkel J, Kanzler S, Frenzel C, Galle PR, Dienes HP, et al. Serologic markers compared with liver biopsy for monitoring disease activity in autoimmune hepatitis. J Clin Gastroenterol 2008;42:926-930.


154. Cook GC, Mulligan R, Sherlock S. Controlled prospective trial of corticosteroid therapy in active chronic hepatitis. Q J Med 1971;40:159-185.


155. Soloway RD, Summerskill WH, Baggenstoss AH, Geall MG, Gitnićk GL, Elveback IR, et al. Clinical, biochemical, and histological remission of severe chronic active liver disease: a controlled study of treatments and early prognosis. Gastroenterology 1972;63:820-833.


156. Murray-Lyon IM, Stern RB, Williams R. Controlled trial of prednisone and azathioprine in active chronic hepatitis. Lancet 1973;1:735-737.


158. Tage-Jensen U, Schlichting P, Aldershvile J, Andersen P, Dietrichson O, Hardt F, et al. Azathioprine versus prednisone in non-alcoholic chronic liver disease (CLD). Relation to a serological classification. Liver 1982;2:95-103.


159. Czaja AJ. Features and consequences of untreated type 1 autoimmune hepatitis. Liver Int 2009;29:816-823.


160. Kogan J, Safadi R, Ashur Y, Shouval D, Ilan Y. Prognosis of symptomatic versus asymptomatic autoimmune hepatitis: a study of 68 patients. J Clin Gastroenterol 2002;35:75-81.

161. Gordon V, Adhikary R, Appleby V, Das D, Day J, Delahooke T, et al.; UK Multi-Centre AIH Audit Group. Treatment and outcome of autoimmune hepatitis (AIH): Audit of 28 UK centres. Liver Int 2022 Mar 14;doi:
10.1111/liv.15241.

162. Schramm C, Weiler-Normann C, Wiegard C, Hellweg S, Müller S, Lohse AW. Treatment response in patients with autoimmune hepatitis. Hepatology 2010;52:2247-2248.


163. Lamers MM, van Oijen MG, Pronk M, Drenth JP. Treatment options for autoimmune hepatitis: a systematic review of randomized controlled trials. J Hepatol 2010;53:191-198.


165. Pape S, Gevers TJG, Belias M, Mustafajev IF, Vrolijk JM, van Hoek B, et al. Predniso(lo)ne dosage and chance of remission in patients with autoimmune hepatitis. Clin Gastroenterol Hepatol 2019;17:2068-2075.e2.


166. Zhang C, Wu SS, Dong XQ, Wu Z, Zhao H, Wang GQ. The efficacy and safety of different doses of glucocorticoid for autoimmune hepatitis: A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e18313.


167. Lohse AW, Mieli-Vergani G. Autoimmune hepatitis. J Hepatol 2011;55:171-182.


169. Stellon AJ, Hegarty JE, Portmann B, Williams R. Randomised controlled trial of azathioprine withdrawal in autoimmune chronic active hepatitis. Lancet 1985;1:668-670.


170. Stellon AJ, Keating JJ, Johnson PJ, McFarlane IG, Williams R. Maintenance of remission in autoimmune chronic active hepatitis with azathioprine after corticosteroid withdrawal. Hepatology 1988;8:781-784.


172. Johnson PJ, McFarlane IG, Williams R. Azathioprine for long-term maintenance of remission in autoimmune hepatitis. N Engl J Med 1995;333:958-963.


173. Heneghan MA, Allan ML, Bornstein JD, Muir AJ, Tendler DA. Utility of thiopurine methyltransferase genotyping and phenotyping, and measurement of azathioprine metabolites in the management of patients with autoimmune hepatitis. J Hepatol 2006;45:584-591.

175. Czaja AJ. Safety issues in the management of autoimmune hepatitis. Expert Opin Drug Saf 2008;7:319-333.


176. Manns MP, Woynarowski M, Kreisel W, Lurie Y, Rust C, Zuckerman E, et al.; European AIH-BUC-Study Group. Budesonide induces remission more effectively than prednisone in a controlled trial of patients with autoimmune hepatitis. Gastroenterology 2010;139:1198-1206.


177. Czaja AJ, Lindor KD. Failure of budesonide in a pilot study of treatment-dependent autoimmune hepatitis. Gastroenterology 2000;119:1312-1316.


178. Manns MP, Jaeckel E, Taubert R. Budesonide in autoimmune hepatitis: The right drug at the right time for the right patient. Clin Gastroenterol Hepatol 2018;16:186-189.


179. Peiseler M, Liebscher T, Sebode M, Zenouzi R, Hartl J, Ehlken H, et al. Efficacy and limitations of budesonide as a second-line treatment for patients with autoimmune hepatitis. Clin Gastroenterol Hepatol 2018;16:260-267.e1.


180. Geier A, Gartung C, Dietrich CG, Wasmuth HE, Reinartz P, Matern S. Side effects of budesonide in liver cirrhosis due to chronic autoimmune hepatitis: influence of hepatic metabolism versus portosystemic shunts on a patient complicated with HCC. World J Gastroenterol 2003;9:2681-2685.


181. Efe C, Ozaslan E, Kav T, Purnak T, Shorbagi A, Ozkayar O, et al. Liver fibrosis may reduce the efficacy of budesonide in the treatment of autoimmune hepatitis and overlap syndrome. Autoimmun Rev 2012;11:330-334.


182. Zachou K, Gatselis NK, Arvaniti P, Gabeta S, Rigopoulou EI, Koukoulis GK, et al. A real-world study focused on the long-term efficacy of mycophenolate mofetil as first-line treatment of autoimmune hepatitis. Aliment Pharmacol Ther 2016;43:1035-1047.


183. Yu ZJ, Zhang LL, Huang TT, Zhu JS, He ZB. Comparison of mycophenolate mofetil with standard treatment for autoimmune hepatitis: a meta-analysis. Eur J Gastroenterol Hepatol 2019;31:873-877.


184. Yeoman AD, Westbrook RH, Zen Y, Maninchedda P, Portmann BC, Devlin J, et al. Early predictors of corticosteroid treatment failure in icteric presentations of autoimmune hepatitis. Hepatology 2011;53:926-934.


185. Czaja AJ. Corticosteroids or not in severe acute or fulminant autoimmune hepatitis: therapeutic brinksmanship and the point beyond salvation. Liver Transpl 2007;13:953-955.


187. Ichai P, Duclos-Vallée JC, Guettier C, Hamida SB, Antonini T, Delvart V, et al. Usefulness of corticosteroids for the treatment of severe and fulminant forms of autoimmune hepatitis. Liver Transpl 2007;13:996-1003.


188. Yeoman AD, Westbrook RH, Zen Y, Bernal W, Al-Chalabi T, Wendon JA, et al. Prognosis of acute severe autoimmune hepatitis (AS-AIH): the role of corticosteroids in modifying outcome. J Hepatol 2014;61:876-882.


192. Hartl J, Ehlken H, Weiler-Normann C, Sebode M, Kreuels B, Pannicke N, et al. Patient selection based on treatment duration and liver biochemistry increases success rates after treatment withdrawal in autoimmune hepatitis. J Hepatol 2015;62:642-646.


196. Czaja AJ, Ammon HV, Summerskill WH. Clinical features and prognosis of severe chronic active liver disease (CALD) after corticosteroid-induced remission. Gastroenterology 1980;78:518-523.


197. Montano-Loza AJ, Carpenter HA, Czaja AJ. Consequences of treatment withdrawal in type 1 autoimmune hepatitis. Liver Int 2007;27:507-515.


199. van Gerven NM, Verwer BJ, Witte BI, van Hoek B, Coenraad MJ, van Erpecum KJ, et al.; Dutch Autoimmune Hepatitis Working Group. Relapse is almost universal after withdrawal of immunosuppressive medication in patients with autoimmune hepatitis in remission. J Hepatol 2013;58:141-147.


202. Hegarty JE, Nouri Aria KT, Portmann B, Eddleston AL, Williams R. Relapse following treatment withdrawal in patients with autoimmune chronic active hepatitis. Hepatology 1983;3:685-689.


204. Czaja AJ. Low-dose corticosteroid therapy after multiple relapses of severe HBsAg-negative chronic active hepatitis. Hepatology 1990;11:1044-1049.


206. Seela S, Sheela H, Boyer JL. Autoimmune hepatitis type 1: safety and efficacy of prolonged medical therapy. Liver Int 2005;25:734-739.


207. Buckley L, Humphrey MB. Glucocorticoid-Induced Osteoporosis. N Engl J Med 2018;379:2547-2556.


210. Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for management of chronic hepatitis B. Clin Mol Hepatol 2022;28:276-331. Erratum in: Clin Mol Hepatol 2022;28:940.
214. Wörns MA, Teufel A, Kanzler S, Shrestha A, Victor A, Otto G, et al. Incidence of HAV and HBV infections and vaccination rates in patients with autoimmune liver diseases. Am J Gastroenterol 2008;103:138-146.


219. Kim HT, Choi R, Won HH, Choe YH, Kang B, Lee K, et al. NUDT15 genotype distributions in the Korean population. Pharmacogenet Genomics 2017;27:197-200.


222. Chang JY, Park SJ, Jung ES, Jung SA, Moon CM, Chun J, et al. Genotype-based treatment with thiopurine reduces incidence of myelosuppression in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol 2020;18:2010-2018.e2.


228. Bodelier AG, Masclee AA, Bakker JA, Hameeteman WH, Pierik MJ. Azathioprine induced pneumonitis in a patient with ulcerative colitis. J Crohns Colitis 2009;3:309-312.


229. Green CJ, Mee AS. Re-introduction of azathioprine in previously intolerant patients. Eur J Gastroenterol Hepatol 2006;18:17-19.


230. Selvarajah V, Montano-Loza AJ, Czaja AJ. Systematic review: managing suboptimal treatment responses in autoimmune hepatitis with conventional and nonstandard drugs. Aliment Pharmacol Ther 2012;36:691-707.


232. Roberts SK, Lim R, Strasser S, Nicoll A, Gazzola A, Mitchell J, et al.; ALA Clinical Research Network. Efficacy and safety of mycophenolate mofetil in patients with autoimmune hepatitis and suboptimal outcomes after standard therapy. Clin Gastroenterol Hepatol 2018;16:268-277.


235. Vergani D, Terziroli Beretta-Piccoli B, Mieli-Vergani G. A reasoned approach to the treatment of autoimmune hepatitis. Dig Liver Dis 2021;53:1381-1393.


236. Fernandes NF, Redeker AG, Vierling JM, Villamil FG, Fong TL. Cyclosporine therapy in patients with steroid resistant autoimmune hepatitis. Am J Gastroenterol 1999;94:241-248.


237. Than NN, Wiegard C, Weiler-Normann C, Füssel K, Mann J, Hodson J, et al. Long-term follow-up of patients with difficult to treat type 1 autoimmune hepatitis on Tacrolimus therapy. Scand J Gastroenterol 2016;51:329-336.


238. Scott LJ, McKeage K, Keam SJ, Plosker GL. Tacrolimus: a further update of its use in the management of organ transplantation. Drugs 2003;63:1247-1297.


239. Brunet M, van Gelder T, Åsberg A, Haufroid V, Hesselink DA, Langman L, et al. Therapeutic drug monitoring of tacrolimus-personalized therapy: second consensus report. Ther Drug Monit 2019;41:261-307.


240. Efe C, Hagström H, Ytting H, Bhanji RA, Müller NF, Wang Q, et al. Efficacy and safety of mycophenolate mofetil and tacrolimus as second-line therapy for patients with autoimmune hepatitis. Clin Gastroenterol Hepatol 2017;15:1950-1956.e1.


241. Lohse AW, Sebode M, Jørgensen MH, Ytting H, Karlsen TH, Kelly D, et al.; European Reference Network on Hepatological Diseases (ERN RARE-LIVER); International Autoimmune Hepatitis Group (IAIHG). Second-line and third-line therapy for autoimmune hepatitis: A position statement from the European Reference Network on Hepatological Diseases and the International Autoimmune Hepatitis Group. J Hepatol 2020;73:1496-1506.


242. Hübener S, Oo YH, Than NN, Hübener P, Weiler-Normann C, Lohse AW, et al. Efficacy of 6-mercaptopurine as second-line treatment for patients with autoimmune hepatitis and azathioprine intolerance. Clin Gastroenterol Hepatol 2016;14:445-453.


245. de Boer YS, van Gerven NM, de Boer NK, Mulder CJ, Bouma G, van Nieuwkerk CM. Allopurinol safely and effectively optimises thiopurine metabolites in patients with autoimmune hepatitis. Aliment Pharmacol Ther 2013;37:640-646.


246. Neuhaus P, Klupp J, Langrehr JM. mTOR inhibitors: an overview. Liver Transpl 2001;7:473-484.


247. Chatrath H, Allen L, Boyer TD. Use of sirolimus in the treatment of refractory autoimmune hepatitis. Am J Med 2014;127:1128-1131.


248. Ytting H, Larsen FS. Everolimus treatment for patients with autoimmune hepatitis and poor response to standard therapy and drug alternatives in use. Scand J Gastroenterol 2015;50:1025-1031.


249. Weiler-Normann C, Schramm C, Quaas A, Wiegard C, Glaubke C, Pannicke N, et al. Infliximab as a rescue treatment in difficult-to-treat autoimmune hepatitis. J Hepatol 2013;58:529-534.


251. Björnsson ES, Gunnarsson BI, Gröndal G, Jonasson JG, Einarsdottir R, Ludviksson BR, et al. Risk of drug-induced liver injury from tumor necrosis factor antagonists. Clin Gastroenterol Hepatol 2015;13:602-608.


252. Burak KW, Swain MG, Santodomingo-Garzon T, Lee SS, Urbanski SJ, Aspinall AI, et al. Rituximab for the treatment of patients with autoimmune hepatitis who are refractory or intolerant to standard therapy. Can J Gastroenterol 2013;27:273-280. Erratum in: Can J Gastroenterol 2013;27:376.
253. Ramachandran J, Sajith KG, Pal S, Rasak JV, Prakash JA, Ramakrishna B. Clinicopathological profile and management of severe autoimmune hepatitis. Trop Gastroenterol 2014;35:25-31.


254. Saadah OI, Smith AL, Hardikar W. Long-term outcome of autoimmune hepatitis in children. J Gastroenterol Hepatol 2001;16:1297-1302.


255. Ferreira AR, Roquete ML, Toppa NH, de Castro LP, Fagundes ED, Penna FJ. Effect of treatment of hepatic histopathology in children and adolescents with autoimmune hepatitis. J Pediatr Gastroenterol Nutr 2008;46:65-70.


256. Mieli-Vergani G, Heller S, Jara P, Vergani D, Chang MH, Fujisawa T, et al. Autoimmune hepatitis. J Pediatr Gastroenterol Nutr 2009;49:158-164.


257. Vergani D, Mieli-Vergani G. Pharmacological management of autoimmune hepatitis. Expert Opin Pharmacother 2011;12:607-613.


260. Dumortier J, Arita CT, Rivet C, LeGall C, Bouvier R, Fabien N, et al. Long-term treatment reduction and steroids withdrawal in children with autoimmune hepatitis: a single centre experience on 55 children. Eur J Gastroenterol Hepatol 2009;21:1413-1418.


262. Maggiore G, Bernard O, Hadchouel M, Hadchouel P, Odievre M, Alagille D. Treatment of autoimmune chronic active hepatitis in childhood. J Pediatr 1984;104:839-844.


263. Maggiore G, Nastasio S, Sciveres M. Juvenile autoimmune hepatitis: Spectrum of the disease. World J Hepatol 2014;6:464-476.

264. Wehrman A, Waisbourd-Zinman O, Shah A, Hilmara D, Lin H, Rand EB. Steroid free treatment of autoimmune hepatitis in selected children. J Pediatr 2019;207:244-247.


265. Banerjee S, Rahhal R, Bishop WP. Azathioprine monotherapy for maintenance of remission in pediatric patients with autoimmune hepatitis. J Pediatr Gastroenterol Nutr 2006;43:353-356.


266. El-Koofy NM, El-Karaksy HM, Aboelsnoon MM, Ibrahim MA, Badawi NE, Fouad HM. Growth and final height in children with autoimmune hepatitis; A long term observation. Int J Pediatr 2022;10:15695-15709.
267. Manwani K, Mieli-Vergani G, Mancell S, Dhawan A, Hadzic N, Samyn M. Long-term growth in children and young people with autoimmune liver disease treated with daily steroids. J Pediatr Gastroenterol Nutr 2022;75:252-256.


268. Woynarowski M, Nemeth A, Baruch Y, Koletzko S, Melter M, Rodeck B, et al.; European Autoimmune Hepatitis-Budesonide Study Group. Budesonide versus prednisone with azathioprine for the treatment of autoimmune hepatitis in children and adolescents. J Pediatr 2013;163:1347-1353.e1.


270. Mohammad S. Budesonide as first-line therapy for non-cirrhotic autoimmune hepatitis in children: a decision analysis. Scand J Gastroenterol 2016;51:753-762.


271. Aw MM, Dhawan A, Samyn M, Bargiota A, Mieli-Vergani G. Mycophenolate mofetil as rescue treatment for autoimmune liver disease in children: a 5-year follow-up. J Hepatol 2009;51:156-160.


272. Richardson PD, James PD, Ryder SD. Mycophenolate mofetil for maintenance of remission in autoimmune hepatitis in patients resistant to or intolerant of azathioprine. J Hepatol 2000;33:371-375.


273. Hennes EM, Oo YH, Schramm C, Denzer U, Buggisch P, Wiegard C, et al. Mycophenolate mofetil as second line therapy in autoimmune hepatitis? Am J Gastroenterol 2008;103:3063-3070.


275. Baven-Pronk AM, Coenraad MJ, van Buuren HR, de Man RA, van Erpecum KJ, Lamers MM, et al. The role of mycophenolate mofetil in the management of autoimmune hepatitis and overlap syndromes. Aliment Pharmacol Ther 2011;34:335-343.


276. Zizzo AN, Valentino PL, Shah PS, Kamath BM. Second-line agents in pediatric patients with autoimmune hepatitis: A systematic review and meta-analysis. J Pediatr Gastroenterol Nutr 2017;65:6-15.


277. Alvarez F, Ciocca M, Cañero-Velasco C, Ramonet M, de Davila MT, Cuarterolo M, et al. Short-term cyclosporine induces a remission of autoimmune hepatitis in children. J Hepatol 1999;30:222-227.


278. Cuarterolo M, Ciocca M, Velasco CC, Ramonet M, González T, López S, et al. Follow-up of children with autoimmune hepatitis treated with cyclosporine. J Pediatr Gastroenterol Nutr 2006;43:635-639.


279. Debray D, Maggiore G, Girardet JP, Mallet E, Bernard O. Efficacy of cyclosporin A in children with type 2 autoimmune hepatitis. J Pediatr 1999;135:111-114.


280. Malekzadeh R, Nasseri-Moghaddam S, Kaviani MJ, Taheri H, Kamalian N, Sotoudeh M. Cyclosporin A is a promising alternative to corticosteroids in autoimmune hepatitis. Dig Dis Sci 2001;46:1321-1327.

282. Cuarterolo ML, Ciocca M, López S, Araujo M, Álvarez F. Autoimmune hepatitis in children: prednisone plus azathioprine versus cyclosporine: A randomized trial. J Pediatr Gastroenterol Nutr 2020;71:376-380.


283. Marlaka JR, Papadogiannakis N, Fischler B, Casswall TH, Beijer E, Németh A. Tacrolimus without or with the addition of conventional immunosuppressive treatment in juvenile autoimmune hepatitis. Acta Paediatr 2012;101:993-999.


286. Rajanayagam J, Lewindon PJ. Infliximab as rescue therapy in paediatric autoimmune hepatitis. J Hepatol 2013;59:908-909.


288. Mostamand S, Schroeder S, Schenkein J, Miloh T. Infliximab-associated immunomediated hepatitis in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2016;63:94-97.


289. Kurowski J, Melin-Aldana H, Bass L, Alonso EM, Ekong UD. Sirolimus as rescue therapy in pediatric autoimmune hepatitis. J Pediatr Gastroenterol Nutr 2014;58:e4-6.


291. van den Brand FF, Snijders RJALM, de Boer YS, Verwer BJ, van Nieuwkerk CMJ, Bloemena E, et al. Drug withdrawal in patients with autoimmune hepatitis in long-term histological remission: A prospective observational study. Eur J Intern Med 2021;90:30-36.


292. Çavuş B, Akyuz F, İliaz R, Atasoy A, Akyuz U, Demir K, et al. Is there any predictor for relapse after treatment withdrawal in autoimmune hepatitis patients in the real life? Int J Immunopathol Pharmacol 2022;36:3946320221077860.

293. Gregorio GV, Portmann B, Karani J, Harrison P, Donaldson PT, Vergani D, et al. Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: a 16-year prospective study. Hepatology 2001;33:544-553.


296. Bonney EA. Alternative theories: Pregnancy and immune tolerance. J Reprod Immunol 2017;123:65-71.


298. Braga A, Vasconcelos C, Braga J. Autoimmune hepatitis and pregnancy. Best Pract Res Clin Obstet Gynaecol 2020;68:23-31.


299. Westbrook RH, Yeoman AD, Kriese S, Heneghan MA. Outcomes of pregnancy in women with autoimmune hepatitis. J Autoimmun 2012;38:J239-244.


300. Terrabuio DR, Abrantes-Lemos CP, Carrilho FJ, Cançado EL. Follow-up of pregnant women with autoimmune hepatitis: the disease behavior along with maternal and fetal outcomes. J Clin Gastroenterol 2009;43:350-356.

302. Muratori P, Loffreda S, Muratori L, Ferrari R, Afandi K, Cassani F, et al. Spontaneous remission of autoimmune hepatitis during pregnancy. Dig Liver Dis 2002;34:608-609.


303. Caballero-Mateos AM, López Garrido MÁ, Becerra Massare P, de Teresa Galván J. Autoimmune severe acute fulminant hepatic failure (FHF) during pregnancy. Gastroenterol Hepatol 2018;41:259-260.


305. Llovet LP, Horta D, Eliz MG, Berenguer M, Fábrega E, Sáez-Royuela F, et al. Presentation and outcomes of pregnancy in patients with autoimmune hepatitis. Clin Gastroenterol Hepatol 2019;17:2819-2821.


308. El Jamaly H, Eslick GD, Weltman M. Systematic review with meta-analysis: autoimmune hepatitis in pregnancy. Scand J Gastroenterol 2021;56:1194-1204.


310. Park-Wyllie L, Mazzotta P, Pastuszak A, Moretti ME, Beique L, Hunnisett L, et al. Birth defects after maternal exposure to corticosteroids: prospective cohort study and meta-analysis of epidemiological studies. Teratology 2000;62:385-392.


313. Götestam Skorpen C, Hoeltzenbein M, Tincani A, Fischer-Betz R, Elefant E, Chambers C, et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis 2016;75:795-810.


314. Granito A, Muratori L, Pappas G, Muratori P, Ferri S, Cassani F, et al. Clinical features of type 1 autoimmune hepatitis in elderly Italian patients. Aliment Pharmacol Ther 2005;21:1273-1277.


315. Miyake Y, Iwasaki Y, Takaki A, Kobashi H, Sakaguchi K, Shiratori Y. Clinical features of Japanese elderly patients with type 1 autoimmune hepatitis. Intern Med 2007;46:1945-1949.


316. Schramm C, Kanzler S, zum Büschenfelde KH, Galle PR, Lohse AW. Autoimmune hepatitis in the elderly. Am J Gastroenterol 2001;96:1587-1591.


317. Chen J, Eslick GD, Weltman M. Systematic review with meta-analysis: clinical manifestations and management of autoimmune hepatitis in the elderly. Aliment Pharmacol Ther 2014;39:117-124.


323. Czaja AJ. Special clinical challenges in autoimmune hepatitis: the elderly, males, pregnancy, mild disease, fulminant onset, and nonwhite patients. Semin Liver Dis 2009;29:315-330.


325. To U, Silveira M. Overlap syndrome of autoimmune hepatitis and primary biliary cholangitis. Clin Liver Dis 2018;22:603-611.


326. Martínez Casas OY, Díaz Ramírez GS, Marín Zuluaga JI, Santos Ó, Muñoz Maya O, Donado Gómez JH, et al. Autoimmune hepatitis - primary biliary cholangitis overlap syndrome. Long-term outcomes of a retrospective cohort in a university hospital. Gastroenterol Hepatol 2018;41:544-552.


327. Al-Chalabi T, Portmann BC, Bernal W, McFarlane IG, Heneghan MA. Autoimmune hepatitis overlap syndromes: an evaluation of treatment response, long-term outcome and survival. Aliment Pharmacol Ther 2008;28:209-220.


330. Floreani A, Rizzotto ER, Ferrara F, Carderi I, Caroli D, Blasone L, et al. Clinical course and outcome of autoimmune hepatitis/primary sclerosing cholangitis overlap syndrome. Am J Gastroenterol 2005;100:1516-1522.


335. Zachou K, Azariadis K, Lytvyak E, Gatselis NK, Takahashi A, Robles M, et al. Nonalcoholic fatty liver disease and steatohepatitis in autoimmune hepatitis: Important player or innocent bystander? J Hepatol 2019;70:e396-397.
336. Adams LA, Lindor KD, Angulo P. The prevalence of autoantibodies and autoimmune hepatitis in patients with nonalcoholic Fatty liver disease. Am J Gastroenterol 2004;99:1316-1320.


339. Dalekos GN, Gatselis NK, Zachou K, Koukoulis GK. NAFLD and autoimmune hepatitis: Do not judge a book by its cover. Eur J Intern Med 2020;75:1-9.


340. Mendes F, Couto CA, Levy C. Recurrent and de novo autoimmune liver diseases. Clin Liver Dis 2011;15:859-878.


342. Cho CW, Kwon CHD, Kim JM, Choi GS, Joh JW, Lee SK. Comparative analysis of the clinical outcomes of liver transplantation for probable and definite auto-immune hepatitis by international diagnostic scoring criteria. Transplant Proc 2017;49:1126-1128.


343. Kwon JH, Hanouneh IA, Allende D, Yerian L, Diago T, Eghtesad B, et al. De novo autoimmune hepatitis following liver transplantation. Transplant Proc 2018;50:1451-1456.


345. Trouillot TE, Shrestha R, Kam I, Wachs M, Everson GT. Successful withdrawal of prednisone after adult liver transplantation for autoimmune hepatitis. Liver Transpl Surg 1999;5:375-380.


346. Hayashi M, Keeffe EB, Krams SM, Martinez OM, Ojogho ON, So SK, et al. Allograft rejection after liver transplantation for autoimmune liver diseases. Liver Transpl Surg 1998;4:208-214.


347. Vogel A, Heinrich E, Bahr MJ, Rifai K, Flemming P, Melter M, et al. Long-term outcome of liver transplantation for autoimmune hepatitis. Clin Transplant 2004;18:62-69.


348. Demetris AJ, Sebagh M. Plasma cell hepatitis in liver allografts: Variant of rejection or autoimmune hepatitis? Liver Transpl 2008;14:750-755.


349. Cholongitas E, Mamou C, Rodríguez-Castro KI, Burra P. Mammalian target of rapamycin inhibitors are associated with lower rates of hepatocellular carcinoma recurrence after liver transplantation: a systematic review. Transpl Int 2014;27:1039-1049.


350. Chen K, Sheng J, Ma B, Cao W, Hernanda PY, Liu J, et al. Suppression of hepatocellular carcinoma by mycophenolic acid in experimental models and in patients. Transplantation 2019;103:929-937.


351. Rigopoulou EI, Dalekos GN. Current trends and characteristics of hepatocellular carcinoma in patients with autoimmune liver diseases. Cancers (Basel) 2021;13:1023.

353. Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, et al.; ESMO Guidelines Committee. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28(suppl_4):iv119-iv142. Erratum in: Ann Oncol 2018;29(Suppl 4):iv264-iv266.
357. Jensen MD, Jepsen P, Vilstrup H, Grønbæk L. Increased cancer risk in autoimmune hepatitis: A Danish nationwide cohort study. Am J Gastroenterol 2022;117:129-137.


358. Ngu JH, Gearry RB, Frampton CM, Stedman CA. Mortality and the risk of malignancy in autoimmune liver diseases: a population-based study in Canterbury, New Zealand. Hepatology 2012;55:522-529.


360. Yeoman AD, Al-Chalabi T, Karani JB, Quaglia A, Devlin J, Mieli-Vergani G, et al. Evaluation of risk factors in the development of hepatocellular carcinoma in autoimmune hepatitis: Implications for follow-up and screening. Hepatology 2008;48:863-870.


363. Migita K, Watanabe Y, Jiuchi Y, Nakamura Y, Saito A, Yagura M, et al.; Japanese NHO-Liver-network study group. Hepatocellular carcinoma and survival in patients with autoimmune hepatitis (Japanese National Hospital Organization-autoimmune hepatitis prospective study). Liver Int 2012;32:837-844.


368. Wang KK, Czaja AJ, Beaver SJ, Go VL. Extrahepatic malignancy following long-term immunosuppressive therapy of severe hepatitis B surface antigen-negative chronic active hepatitis. Hepatology 1989;10:39-43.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement1
Supplement1 Print
Print




