1. Landi F, Onder G, Russo A, Liperoti R, Tosato M, Martone AM, et al. Calf circumference, frailty and physical performance among older adults living in the community. Clin Nutr 2014;33:539-544.


2. Mijnarends DM, Meijers JM, Halfens RJ, ter Borg S, Luiking YC, Verlaan S, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc 2013;14:170-178.


4. Beaudart C, Reginster JY, Slomian J, Buckinx F, Locquet M, Bruy├©re O. Prevalence of sarcopenia: the impact of different diagnostic cut-off limits. J Musculoskelet Neuronal Interact 2014;14:425-431.


6. Hemmingsson E, Udd├®n J, Neovius M. No apparent progress in bioelectrical impedance accuracy: validation against metabolic risk and DXA. Obesity (Silver Spring) 2009;17:183-187.


8. Pedersen BK. Exercise-induced myokines and their role in chronic diseases. Brain Behav Immun 2011;25:811-816.


9. Pedersen BK. Muscles and their myokines. J Exp Biol 2011;214(Pt 2):337-346.


10. Pedersen BK, Akerstr├Čm TC, Nielsen AR, Fischer CP. Role of myokines in exercise and metabolism. J Appl Physiol (1985) 2007;103:1093-1098.


11. Halmos T, Suba I. The secretory function of skeletal muscles and its role in energy metabolism and utilization. Orv Hetil 2014;155:1469-1477.


14. Edge S, Byrd D, Compton C, Fritz A, Greene F, Trotti A. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
15. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018;68:723-750.


17. Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Hammad A, Tamai Y, et al. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition 2016;32:1200-1205.


20. Lausen B, Schumacher M. Maximally selected rank statistics. Biometrics 1992;48:73-85.

21. Lausen B, Sauerbrei W, Schumacher V. Classification and regression trees (CART) used for the exploration of prognostic factors measured on different scales. Computational Statistics. Heidelberg: Physica-Verlag; 1994. p. 483-496.
22. Hosoyama T, Yamanouchi K, Nishihara M. Role of serum myostatin during the lactation period. J Reprod Dev 2006;52:469-478.


23. McNally EM. Powerful genes--myostatin regulation of human muscle mass. N Engl J Med 2004;350:2642-2644.


27. Loumaye A, de Barsy M, Nachit M, Lause P, Frateur L, van Maanen A, et al. Role of activin A and myostatin in human cancer cachexia. J Clin Endocrinol Metab 2015;100:2030-2038.


29. Jeanplong F, Osepchook CC, Falconer SJ, Smith HK, Bass JJ, McMahon CD, et al. Undernutrition regulates the expression of a novel splice variant of myostatin and insulin-like growth factor 1 in ovine skeletal muscle. Domest Anim Endocrinol 2015;52:17-24.


30. Furihata T, Kinugawa S, Fukushima A, Takada S, Homma T, Masaki Y, et al. Serum myostatin levels are independently associated with skeletal muscle wasting in patients with heart failure. Int J Cardiol 2016;220:483-487.


31. Zhou X, Wang JL, Lu J, Song Y, Kwak KS, Jiao Q, et al. Reversal of cancer cachexia and muscle wasting by ActRIIB antagonism leads to prolonged survival. Cell 2010;142:531-543.


32. Wagner KR, Fleckenstein JL, Amato AA, Barohn RJ, Bushby K, Escolar DM, et al. A phase I/IItrial of MYO-029 in adult subjects with muscular dystrophy. Ann Neurol 2008;63:561-571.


33. Hansen JS, Rutti S, Arous C, Clemmesen JO, Secher NH, Drescher A, et al. Circulating follistatin is liver-derived and regulated by the glucagon-to-insulin ratio. J Clin Endocrinol Metab 2016;101:550-560.


34. Zhang L, Liu K, Han B, Xu Z, Gao X. The emerging role of follistatin under stresses and its implications in diseases. Gene 2018;639:111-116.


36. Kalinkovich A, Livshits G. Sarcopenia--the search for emerging biomarkers. Ageing Res Rev 2015;22:58-71.


38. Grusch M, Drucker C, Peter-V├Čr├Čsmarty B, Erlach N, Lackner A, Losert A, et al. Deregulation of the activin/follistatin system in hepatocarcinogenesis. J Hepatol 2006;45:673-680.


39. Rossmanith W, Chabicovsky M, Grasl-Kraupp B, Peter B, Schausberger E, Schulte-Hermann R. Follistatin overexpression in rodent liver tumors: a possible mechanism to overcome activin growth control. Mol Carcinog 2002;35:1-5.


40. Fabregat I, Moreno-C├Āceres J, S├Īnchez A, Dooley S, Dewidar B, Giannelli G, et al. TGF-╬▓ signalling and liver disease. FEBS J 2016;283:2219-2232.


41. Nishida N, Kudo M. Immune checkpoint blockade for the treatment of human hepatocellular carcinoma. Hepatol Res 2018;48:622-634.


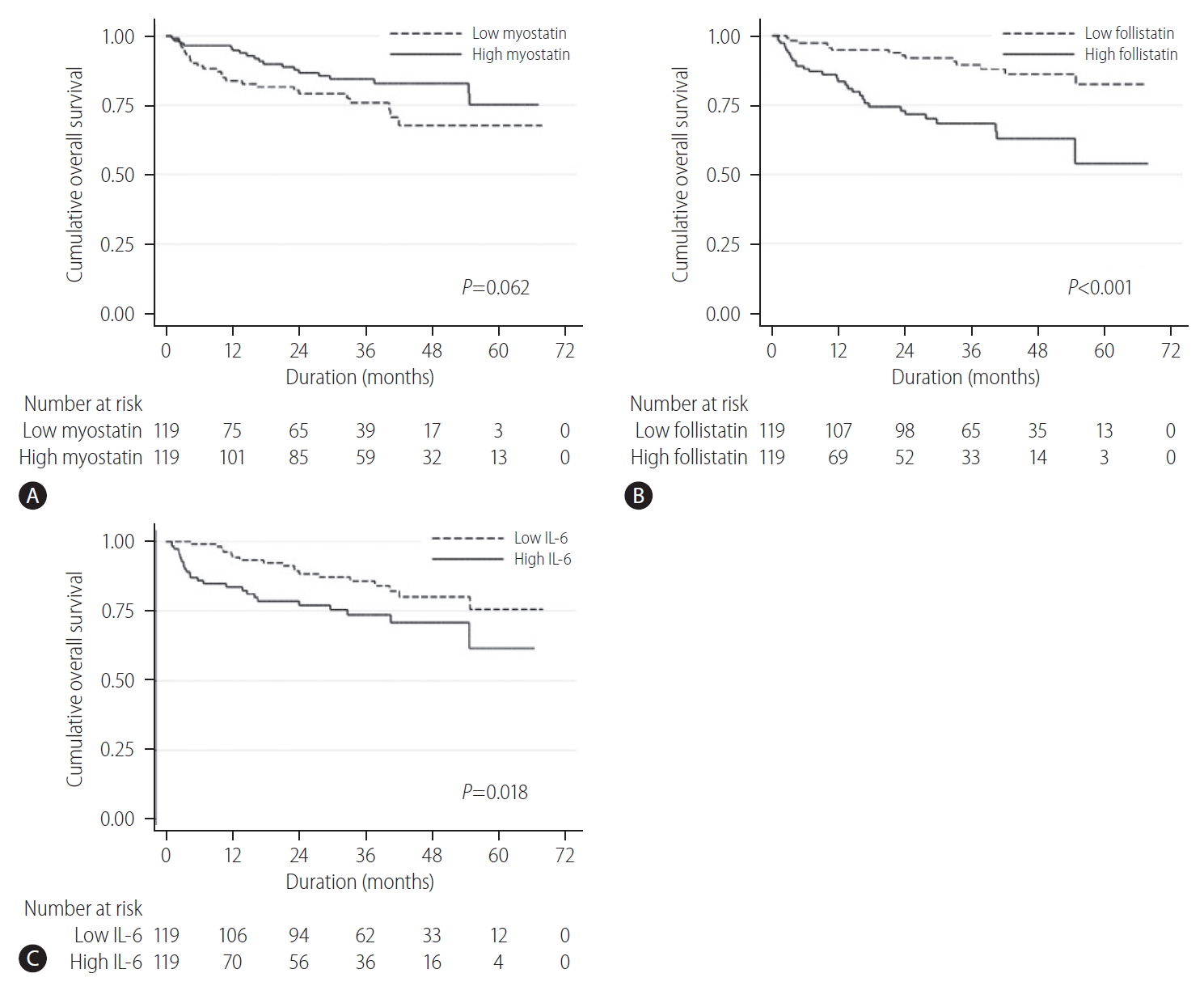
42. Tomoda T, Nouso K, Miyahara K, Kobayashi S, Kinugasa H, Toyosawa J, et al. Prognotic impact of serum follistatin in patients with hepatocellular carcinoma. J Gastroenterol Hepatol 2013;28:1391-1396.


44. Krabbe KS, Pedersen M, Bruunsgaard H. Inflammatory mediators in the elderly. Exp Gerontol 2004;39:687-699.


48. Delogu W, Caligiuri A, Provenzano A, Rosso C, Bugianesi E, Coratti A, et al. Myostatin regulates the fibrogenic phenotype of hepatic stellate cells via c-jun N-terminal kinase activation. Dig Liver Dis 2019;51:1400-1408.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Supplement1
Supplement1 Print
Print



